Spectrum of gastrointestinal involvement in Stevens - Johnson syndrome
2019-02-27AshishKumarJhaAryaSuchismitaRajeevKumarJhaVikasKumarRaj
Ashish Kumar Jha, Arya Suchismita, Rajeev Kumar Jha, Vikas Kumar Raj
Abstract Stevens - Johnson syndrome (SJS) or toxic epidermal necrolysis (TEN) is a severe adverse drug reaction associated with involvement of skin and mucosal membranes, and carries significant risk of mortality and morbidity. Mucus membrane lesions usually involve the oral cavity, lips, bulbar conjunctiva and the anogenitalia. The oral/anal mucosa and liver are commonly involved in SJS or TEN. However, intestinal involvement is distinctly rare. We herein review the current literature regarding the gastrointestinal involvement in SJS or TEN. This review focuses mainly on the small bowel and colonic involvement in patients with SJS or TEN.
Key words: Stevens - Johnson syndrome; Toxic epidermal necrolysis; Lyell's syndrome;Gastrointestinal involvement; Colon; Ileum
INTRODUCTION
Stevens - Johnson syndrome (SJS) comprises a widespread, cutaneous eruption with features resembling erythema multiforme in combination with constitutional symptoms such as fever and malaise, and mucosal lesions classically affecting the eyes, mouth, and genitalia[1]. Toxic epidermal necrolysis (TEN) is defined by involvement of at least 30% of total body surface area (TBSA) of the skin, and frequently involves at least two mucus membranes[2]. The skin involvement in SJS and SJS/ TENS overlap is < 10% and 10%-30% of TBSA, respectively. Fuchs syndrome or atypical SJS a very rare entity is defined as SJS-like mucositis without skin involvement[3].
Extracutaneous manifestations of the SJS or TEN can occur and may involve the conjunctiva, buccal mucosa, trachea, gastrointestinal (GI) tract, and genitourinary tract. Mucus membrane lesions usually involve the oral cavity, lips, bulbar conjunctiva and the anogenitalia. The mucosal lesions may go parallel, may follow or even precede the rash[4,5]. We herein review the current literature regarding the GI involvement in SJS or TEN. This review focuses mainly on the small bowel and colonic involvement in patients with SJS or TEN, which are distinctly rare.
ETIOPATHOGENESIS
SJS or TEN have been postulated to be a hypersensitivity reaction triggered by a variety of stimuli[4,6]. The most common precipitants are drugs followed by infections with mycoplasma, herpes and cytomegalo virus[7]. Beta lactam/sulfonamide antibiotics, NSAIDs (diclofenac, ketorolac, sulindac, piroxicam, and oxyphenbutazone), chlormezanone, and aromatic anticonvulsant are the most common drugs responsible for SJS or TEN.
The pathogenesis of SJS or TEN appears to be an immune mediated process.Damage of keratinocytes and mucosal epithelium is mediated by a cell-mediated and cytotoxic immune process. Activated T-cells stimulate extensive apoptosis by direct cell-cell interactions (via CD95 and Fas ligand-mediated signaling pathway), and by secretion of factors such as perforin, granulysin and cytokines (TNFa)[8-10]. The skin and other tissues appears to be affected by common mechanism of the Fas-ligand and the perforin-granulysin pathways. The mechanism by which SJS or TEN affects the intestine is identical to one that causes skin lesions. The pathologic features of both the skin and GI lesions are similar to acute graft-vs-host disease such as full-thickness epithelial necrosis and detachment, epithelial crypt cells necrosis, and a relative sparing of lamina propria. However, lymphomononuclear cell infiltrations of lamina propria can be present in some patients[11,12]. The colonic mucosa is found to constitutively express CD95[13]. The mechanism of delayed and/or persistent intestinal inflammation is not clear.
SPECTRUM OF GASTROINTESINAL INVOLVEMENT
Extent of Disease
GI complications are not uncommon in SJS or TEN and are usually mild. Some of the GI manifestations can be observed in about 10% of patients with SJS or TEN[4,14].Severe GI involvement of SJS or TEN is rare but potentially life-threatening. In a study by Yamane et al[14], GI involvement noted in 9 (10%) of patients with SJS or TEN (n =87). Common GI symptoms were diarrhea, intestinal bleeding, and severe appetite loss. One patient was expired due to perforation of intestine, DIC and pneumonia[14].The oral/anal mucosa and liver are frequently involved in patients with SJS or TEN[14,15]. Esophageal involvement in patients with SJS or TEN is not so rare.Esophageal ulcer and chronic esophageal stricture formation have been described in SJS or TEN[16-20]. Small bowel and colonic involvement are distinctly rare. We were able to find detailed reports of about 25 cases [age (range) 8-81 years; male: female ratio of 7:18] of SJS or TEN with GI involvement (Table 1 and Table 2)[11,12,21-39]. Details of patients with small bowel and colonic involvement are summarized in Table 2. Small bowel and colonic lesions are often associated with lesions in the other parts of GI tract. Isolated involvement of the small bowel and colon does occur but is quite uncommon. The “skip” involvement of the GI tract has been described in SJS or TEN with the distal stomach and small and/or large bowel involvement, and sparing of the esophagus and proximal stomach[37].
Clinical presentation
GI manifestations usually reveals within two weeks of cutaneous lesions, but it can present many weeks after initial cutaneous symptoms. Symptoms may persist for months after disappearance of skin lesions, and duration of as long as 9 mo have been described (Table 1 and Table 2). Passage of a tubular mass of necrotic epithelium and fibrinous exudates in the stool was reported after 25 d of skin lesion[35].
The usual presenting symptoms include GI bleeding (hemetemesis, melena, and hematochezia), diarrhea, abdominal pain, abdominal distension and dysphagia.Diarrhoea is usually profuse and watery. Patients may also present with blood mixed in with the stool. Inflammation of GI tract such as esophagitis, gastritis, duodenitis,jejunitis, ileitis and colitis are common GI lesions (60%). Ulcers in the colon, small bowel, esophagus and stomach are responsible for GI bleeding in these patients (36%).Patients can be diagnosed with ulcers in multiple locations. Large bowel is most common site of ulcer followed by small bowel and stomach. Intestinal perforation and strictures (single or multiple) have been reported in three (12%) and two (8%)patients, respectively. Mesentric ischaemia, intestinal infarction, intraabdominal abscess, ileoileal intussusceptions, and subacute intestinal obstruction (one patient each) have also been described in SJS. Patients can also presents with protein-losing enteropathy, malabsorption syndromes, and hypoalbumenia. Evaluation of a patient presented with diarrhea, protein-losing enteropathy and malabsorption syndrome revealed multiple ileal strictures, pseudodiverticular sacs and pseudomembranes formation. Stricture, intestinal wall edema, intussusception and luminal stenosis caused by erosion and sublation of intestinal mucosa are the reasons for intestinal obstruction in these patients[31,36,39]. Laprotomy and necropsy of a patient presented with subacute intestinal obstruction showed hemorrhage, petechie, ecchymosis, and congestion in the stomach, small bowel, proximal large bowel and gall bladder[39].Heye et al[40]showed an association between perforation of sigmoid diverticulitis and SJS, though the casual relationship was unclear.
SJS or TEN is mostly treated with prolonged antibiotic course and immunosuppressive drugs and the GI symptoms may appear late in the course of illness. The differential diagnosis in such clinical scenario often includes infective colitis especially viral, antibiotic associated diarrhea, pseudomembranous colitis and first episode of inflammatory bowel disease.
Endoscopic and histopathological features
There are various endoscopic findings observed in patients with SJS/TEN. These include the hyperemia, erythema, congestion, friability, erosions, superficial or deep ulcerations and necrotic plaque formation with mucosal sloughing (Figure 1) (Table 1). Ulcer may be irregular, friable and covered with white fibrin-like exudates[21].Whitish plaques and pseudomembrane formation over the damaged mucosa are the other endoscopic findings in SJS or TEN. Although colonic pseudomembrane has not been reported yet, ulcerations with adherent pseudomembrane have been described in the esophagus and ileum[16,36].
Histopathological (HPE) features of biopsy or autopsy specimen include mucosal ulceration with epithelial necrosis and lymphomononuclear cell infiltrations in early stage, and severe necrotic ulcerations, lymphomononuclear infiltration of the lamina propria and inflamed granulation tissue, later in the course[11,12,37]. Lamina propria is relatively spared in these patients. HPE of healing colonic ulcer showed marked crypt architectural distortion and significant crypt loss, suggesting injury to the crypt stem cell population[21].
HEPATIC AND PANCREATIC MANIFESTATIONS
Hepatic complications of SJS or TEN includes asymptomatic hepatic enzymes elevation, hepatitis, cholestastic hepatitis, and hepatic failure. In a study by Yamane et al[14], hepatitis was the most common complication in seen in 47% of patients with SJS or TEN. Cholestatic liver disease, which may precede the skin manifestations of SJS or TEN, has been reported in nearly 12 cases of SJS or TEN[41-45]. Acute liver failure also has been described in association with SJS or TEN; however the exact casualrelationship was not established[46].
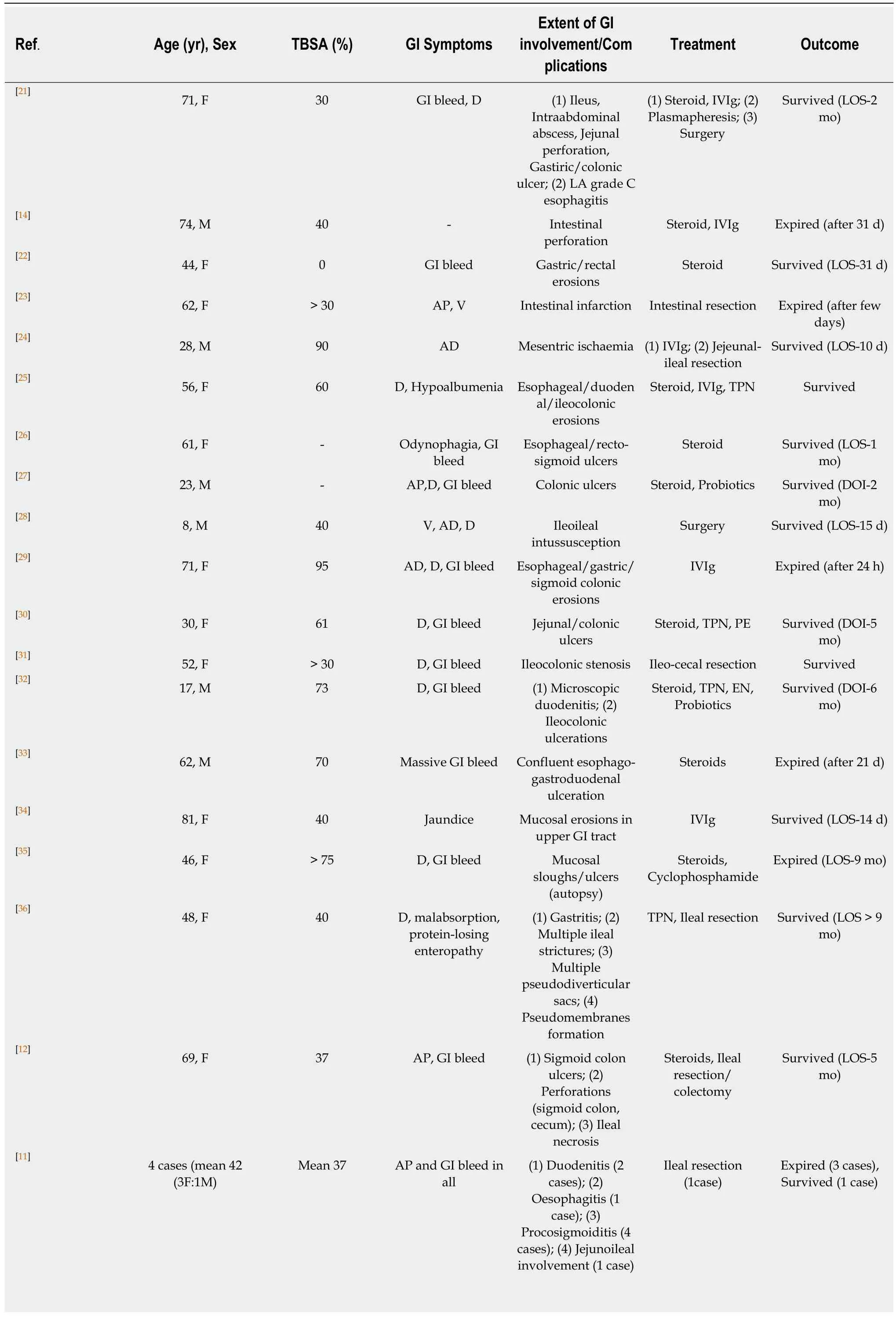
Table 1 Reported cases of Stevens - Johnson syndrome or toxic epidermal necrolysis with gastrointestinal involvement
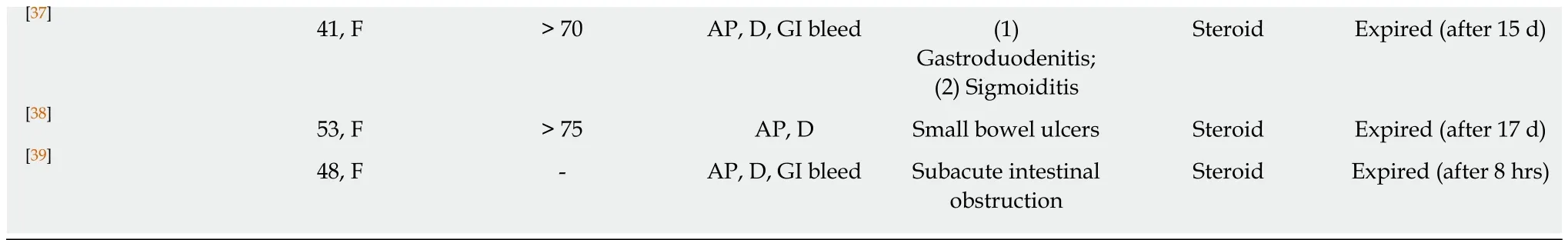
TBSA: Total body surface area; GI: Gastrointestinal; M: Male; F: Female; TPN: Total parenteral nutrition; LOS: Length of stay; D: Diarrhea; V: Vomiting; AP:Abdominal pain; AD: Abdominal distension; IVIg: Intravenous immunoglobulin; PE: Plasma exchange; EN: Enteral nutrition; DOI: Duration of illness.
Pancreas involvement is rarely described in patients with SJS or TEN. A few cases of asymptomatic pancreatic enzymes elevation and acute pancreatitis are described in SJS or TEN[47-49]. In a study by Dylewski et al[47], enteral nutrition was tolerated by all patients of TEN with asymptomatic pancreatic enzymes elevation. Therefore, in the absence of symptomatic pancreatitis, patients with SJS or TEN can be supported with enteral nutrition[47].
MANAGEMENT
Treatment of SJS or TEN is still controversial. Withdrawal of offending drugs and admission in a burn intensive care unit is recommended. Disease severity and prognosis can be assessed with the SCORTEN criteria[50].The treatment of SJS or TEN is largely supportive. Supportive care include the management of airway, fluid and electrolyte balance, monitoring of renal function, nutritional supplementation,adequate analgesia, care of skin and mucosal surfaces, and prevention of infection.Currently used medical therapy comprised of systemic corticosteroids, intravenous immunoglobulins (IVIg), cyclosporine, plasmapheresis, plasma exchange, antitumor necrosis factor drugs and N-acetylcysteine, but none has been established as the most effective therapy. Systemic steroids are used as standard of care for treatment of SJS or TEN. A few case series have reported favorable outcomes in patients treated with corticosteroids and immunoglobulin[8,51,52]. But, data does not support use of steroid as sole therapy, and are no longer recommended[53]. A meta-analysis showed no survival benefit among SJS or TEN patients treated with intravenous immunoglobulin[54].
Patients of SJS or TEN with GI involvement may be treated conservatively or may require surgery. Conservative treatment consists of supportive measures, systemic steroids, intravenous immunoglobulin, probiotics, plasma exchange, and supplemental nutrition. Role of steroid in patients with SJS or TEN with GI involvement is trickier. Steroids may exacerbate mucosal sloughing, GI bleeding and perforation in SJS or TEN. Huang et al[54]showed decreased rates of GI complications of SJS or TEN after steroids were removed from their treatment protocol. Therefore,the choice of treatment depends on the available guidelines and the experience of the treating physician. A multidisciplinary approach is warranted, and treatment should be determined on an individual basis. Out of 25 patients, surgery was performed in eight (32%) cases. It is worth mentioning that in the patients who required a surgical intervention (8 patients) for GI manifestations, all but one patient was survived (Table 1).
PROGNOSIS
Patients with SJS or TEN and intestinal involvement have a poor prognosis. Nearly half (44%) of reported cases had fatal outcome (Table 2). Patients who survived have increased risk of late GI complications. These include strictures of the esophagus,ileum and anal canal as well as ileal pseudodiverticulae[15,17,36].
CONCLUSION
GI complications are not uncommon in SJS or TEN and are usually mild. Severe GI involvement of SJS or TEN is rare but potentially life-threatening. GI manifestations usually reveal within two weeks of cutaneous lesions, but these symptoms may be delayed. These patients may be treated conservatively or may require surgery. The conservative treatment is mainly supportive and current data does not support use of steroid or IVIg. A multidisciplinary approach is warranted and treatment should bedetermined on an individual basis.
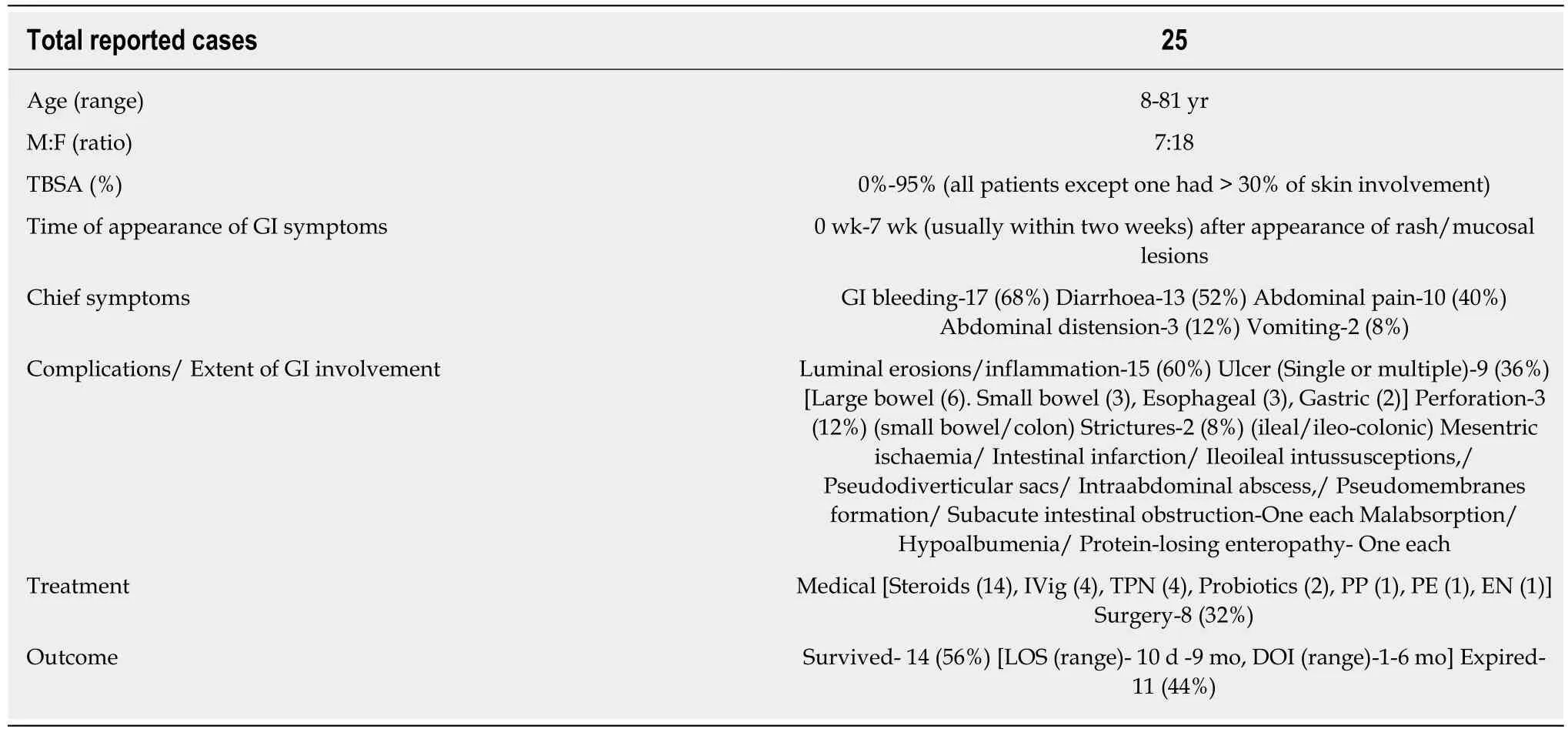
Table 2 Spectrum of gastrointestinal involvement in Stevens - Johnson syndrome or total parenteral nutrition
FUTURE DIRECTIONS
Pathogenesis of SJS or TEN is still not clear. Mechanism of patchy/skip involvement of GI tract are unknown. Better understanding of pathogenesis may help to develop a new and effective therapy for this dangerous disease. Because of rarity of disease, the randomized controlled trials regarding the efficacy of various drugs are difficult to perform. Therefore, multicentre randomized controlled trials are warranted to compare the efficacy of available treatment options.

Figure 1 Colonoscopy images. A-C: Colonoscopy images showing erythema, congestion and exudates.
杂志排行
World Journal of Gastrointestinal Endoscopy的其它文章
- Role of endoscopy in acute gastrointestinal bleeding in real clinical practice: An evidence-based review
- Role of endoscopy in the management of primary sclerosing cholangitis
- Radiofrequency and malignant biliary strictures: An update
- Endoscopic ultrasound-guided drainage of the biliary system:Techniques, indications and future perspectives
- No significant difference in clinically relevant findings between Pillcam® SB3 and Pillcam® SB2 capsules in a United States veteran population
- Age, socioeconomic features, and clinical factors predict receipt of endoscopic retrograde cholangiopancreatography in pancreatic cancer
