血嗜酸性粒细胞计数与冠状动脉旁路移植手术后肺炎风险
2018-08-27谭淑芳张丽芝黄林洁石健庭唐恬恬林小玲
谭淑芳, 张丽芝, 黄林洁, 陈 茗, 张 蔚, 石健庭, 唐恬恬, 林小玲△
(中山大学孙逸仙纪念医院1手术室,2呼吸内科, 广东 广州 510120)
Eosinophils play an important role in defense against various pathogens, including parasitic, bacterial and viral infections. Low blood eosinophil count was considered as a reliable predictor of sepsis and increased mortality in critically ill medical patients[1-3]. However, the relationship between blood eosinophil count and risk of pneumonia in the patients with chronic obstructive pulmonary disease (COPD) is controversial. It was reported that blood eosinophil count of 0.34×109/L and higher was associated with high risk of pneumonia hospitalization in the patients with COPD and forced expiratory volume in the first second (FEV1)<50% of the predicted value[4]. Conversely, a meta-analysis study found that the risk of pneumonia slightly increased in the patients with COPD and blood eosinophil count below 2%[5]. Since eosinophils are also involved in the persistent airway inflammation in the patients with COPD and high blood eosinophil count is associated with more exacerbation risk and inhaled corticosteroids which increase risk of pneumonia[6], researches about the relationship of eosinophils and risk of pneumonia in patients with COPD are likely to produce heterogeneous results. It is better to investigate the relationship between blood eosinophil count and risk of pneumonia in the non-COPD patients.
Although percutaneous coronary intervention (PCI) has been rapidly developed for the patients with coronary artery disease in recent decades, coronary artery bypass graft (CABG) surgery remains the standard procedure in the patients with complex lesions[7]. Postoperative pneumonia is the prevailing nosocomial infection and increases morbidity and mortality in the patients with CABG surgery[8]. As reported, the risk factors of nosocomial pneumonia in the patients with cardiac surgery include age (>70 years), COPD, preoperative left ventricular ejection fraction (LVEF, <60%), red blood cell transfusions, length of mechanical ventilation (more than 2 d), receipt of antacids and so on[9-10]. However, no attention to blood eosinophil count is reported. It has been reported that preoperative low blood eosinophil count is an independent predictor of early mortality for CABG surgery[11]. So far, the relationship between eosinophil count and risk of post-operative pneumonia following CABG surgery is unclear.
In this retrospective cohort study, we aimed to investigate the relationship between blood eosinophil count and risk of postoperative pneumonia following CABG surgery. We also tried to explore the potential role of blood eosinophil count as a marker of hospital mortality in the patients with CABG surgery.
MATERIALS AND METHODS
1 Subjects
This retrospective cohort study was performed in the Sun Yat-sen Memorial Hospital of Sun Yat-sen University. The medical records of the patients who underwent coronary artery bypass graft surgery from January 2008 to December 2017 were collected and reviewed. The study protocol was approved by the Ethic Committee of Sun Yat-sen Memorial Hospital (EC number: SYSEC-KY-KS-2018-026).
2 Diagnosis of postoperative pneumonia
The clinical diagnosis of postoperative pneumonia was defined as the presence of new infiltration on the chest X-ray together with symptoms and signs of a lower respiratory tract infection in a patient who underwent CABG surgery. The symptoms and signs of a lower respiratory tract infection included: fever (>38 ℃) or hypothermia (<36 ℃), white blood cell (WBC) >10×109/L or <4×109/L and purulent respiratory secretions.
3 Exclusion criteria
We excluded: (1) age <18 years old; (2) the patient with pneumonia at admission before CABG surgery; (3) the patients with human immunodeficiency virus (HIV) infection; (4) the patient with immuno-suppressive therapy (injected or oral glucocorticoids or other immunosuppressive agents, not including inhaled corticosteroids); (5) the patient with malignant tumor; (6) the patient with parasitic infection (diagnosed by parasite egg count in stool routine).
4 Data collection
Besides blood eosinophil count (in percentage of all leukocytes), other clinical and laboratory data of the patients who underwent CABG surgery were collected and analyzed, including sex, age, underlying disease, history of cigarette smoking, alcohol abuse and inhaled corticosteroids, blood pressure and heart rate at admission, body mass index (BMI), results of laboratory investigation, chest X-ray findings, LVEF, emergency operation, blood transfusion, intra-aortic balloon pump (IABP), cardiopulmonary bypass (CPB), analgesic drugs, antacids, nasogastric tube, reintubation, tracheotomy, length of mechanical ventilation and ICU stay, diagnosis of postoperative pneumonia, pathogens isolated and identified from blood or respiratory secretions, and the clinical outcome.
The results of laboratory measurement collected before surgery were blood leucocyte count, hemoglobin, total bilirubin, serum albumin, blood urea nitrogen (BUN), creatinine, and C-reactive protein (CRP).
5 Statistical analysis
All analyses were performed by the SPSS 22.0 software. Quantitative variables of normal distribution were expressed as mean±standard deviation (SD), and Studentt-test was used to compare the data. Quantitative variables of non-normal distribution were expressed as medians (25th and 75th percentiles), and Rank Sum test was used to compare the data. Qualitative data were presented as frequencies and percentages, and compared by Chi-square test. Variables withPvalues <0.05 were then introduced into a forward, stepwise, multivariate logistic regression model.P<0.05 was considered to be statistically significant.
RESULTS
1 General characteristics
As shown in Figure 1, a total of 613 patients who underwent CABG surgery from January 2008 to December 2017 in our hospital were screened for eligibility, of which 31 patients were later excluded (10 patients were due to pneumonia at admission before CABG surgery, 1 patients was due to immunosuppressive therapy, 18 patients were due to malignant tumor, and 2 patients were due to parasite infection). The remaining 582 patients were enrolled in the study and divided into 2 groups: high and low eosinophil counts defined by a cut-point in percentage of all leukocytes of 2%, which has been widely used[12]. The patients with preoperative blood eosinophil counts of less than 2% were 220, and those with eosinophil counts of 2% or more were 362.
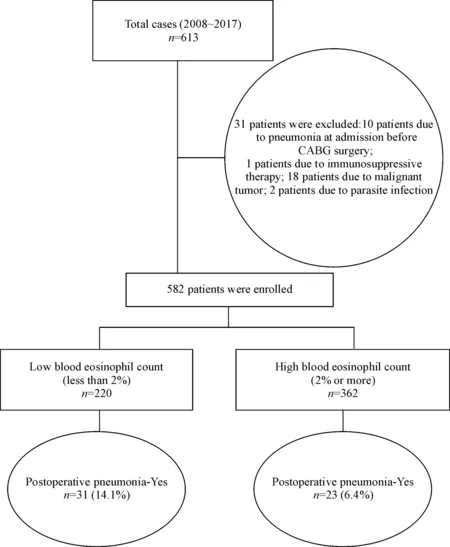
Figure 1.Study flow diagram.
The incidence of postoperative pneumonia in the patients with low blood eosinophil count was much higher than the patients with high blood eosinophil count. Thirty-one (14.1%) patients with blood eosinophil counts less than 2% developed postoperative pneumonia as compared with 23 (6.4%) patients with blood eosinophil counts of 2% or more (P=0.002). However, hospital mortality of the patients with high or low blood eosinophil count had no difference: 13 (5.9%) deaths with blood eosinophil counts less than 2% compared with 13 (3.6%) with blood eosinophil counts of 2% or more (P=0.189), as shown in Table 1.

Table 1.Postoperative pneumonia and death in the patients with low or high blood eosinophil count
2 Clinical characteristics for the patients who underwent CABG surgery
Table 2 showed the variables of the patients who underwent CABG surgery. The variables were significantly different between the patients with postoperative pneumonia and without pneumonia, including low blood eosinophil count (P=0.002), nasogastric tube (P<0.001), reintubation (P=0.012), tracheotomy (P=0.025) and mechanical ventilation ≥ 24 h (P=0.006).
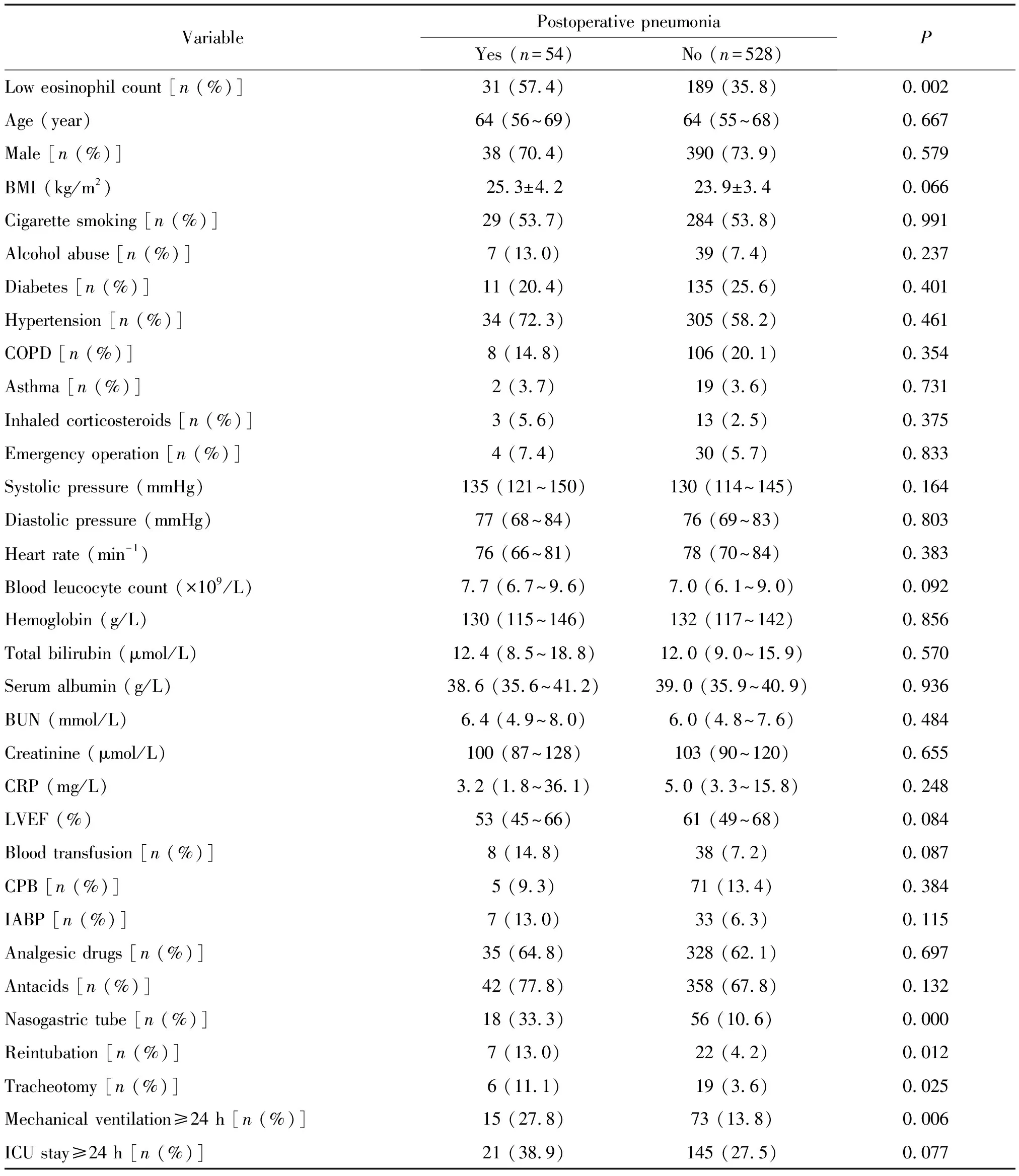
Table 2.Variables for the patients who underwent CABG surgery with or without postoperative pneumonia
BMI: body mass index; COPD: chronic obstructive pulmonary disease; BUN: blood urea nitrogen; CRP: C-reactive protein; LVEF: left ventricular ejection fraction; CPB: cardiopulmonary bypass; IABP: intra-aortic balloon pump.
3 Independent risk factors to develop postoperative pneumonia
A multivariate logistic regression analysis which included low blood eosinophil count, nasogastric tube, reintubation, tracheotomy and mechanical ventilation ≥ 24 h as the risk factors was performed. As showed in Table 3, low blood eosinophil count (OR=3.521, 95% CI: 1.213~10.223,P=0.021) was identified as an independent risk factor for postoperative pneumonia following CABG surgery, as well as nasogastric tube (OR=6.490, 95% CI: 2.757~15.280,P<0.001) and mechanical ventilation≥24 h (OR=3.496, 95% CI: 1.156~10.178,P=0.035).
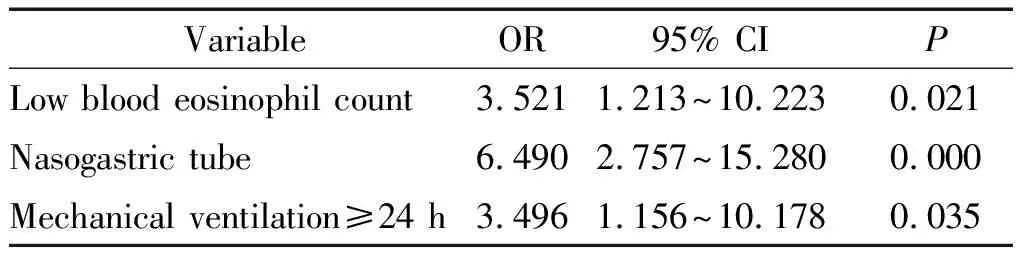
Table 3.Independent risk factors for postoperative pneumonia development by multivariate logistic regression analysis
OR: odds ratio; CI: confidence interval.
4 Etiology
All patients who developed postoperative pneumonia following CABG surgery underwent a blood culture and a respiratory secretion culture. A total of 44 species of bacteria and 13 species of fungi were isolated and identified in 26 of 54 patients (48.1%) who developed pneumonia. The number of the detected pathogens was showed in Table 4. The most common pathogens werePseudomonasaeruginosa,StaphylococcusepidermidisandCandidaalbicans.
DISCUSSION
In the present study, preoperative low blood eosinophil count was identified as an independent risk factor for postoperative pneumonia development in the patients who underwent CABG surgery. However, it was not a predictor of hospital mortality for the patients with CABG surgery.
In this retrospective cohort study, we found that preoperative blood eosinophil count was associated with the risk of postoperative pneumonia following CABG surgery. The patients with low blood eosinophil count suffered more risk of postoperative pneumonia following CABG surgery. Eosinophils play complex roles in both systemic inflammatory diseases and pathogenic infections. On the one hand, in the patients with COPD, high blood eosinophil count may reflect persistent eosi-nophilic inflammation in the airway and severe lung function impairment, which increase the susceptibility to pneumonia. On the other hand, eosinophils probably provide a strong defense against invading microbes. This can partly explain the conflicting results of researches about blood eosinophil count and risk of pneumonia in the patients with COPD[4-5]. In the patients with severe COPD, the damage in airway induced by the effect of eosinophils exceeds their protection against pathogen, so higher blood eosinophil count is associated with more risk of pneumonia. In the patients with moderate or mild COPD, since the damage in the airway induced by eosinophils is counterbalanced by their protection against pathogens, there may be no connection between blood eosinophil count and risk of pneumonia. In the patients with mild COPD or non-COPD, eosinophils mainly behave as a defender of our body against invading microbes, so higher blood eosinophil count decreases risk of pneumonia. This matches the case in our study. In short, the relationship between blood eosinophil count and risk of pneumonia probably differs by group with different grades of COPD or non-COPD. Furthermore, the mechanism of low blood eosinophil count increasing the risk of pneumonia may be due to its functional characterization. Eosinophils can release cytotoxins through degranulation to modulate the immune response, phagocytose the invading pathogens, kill them intracellularly and help to antigen presentation. In addition, eosinophils have the capacity to regulate the function of T cells.
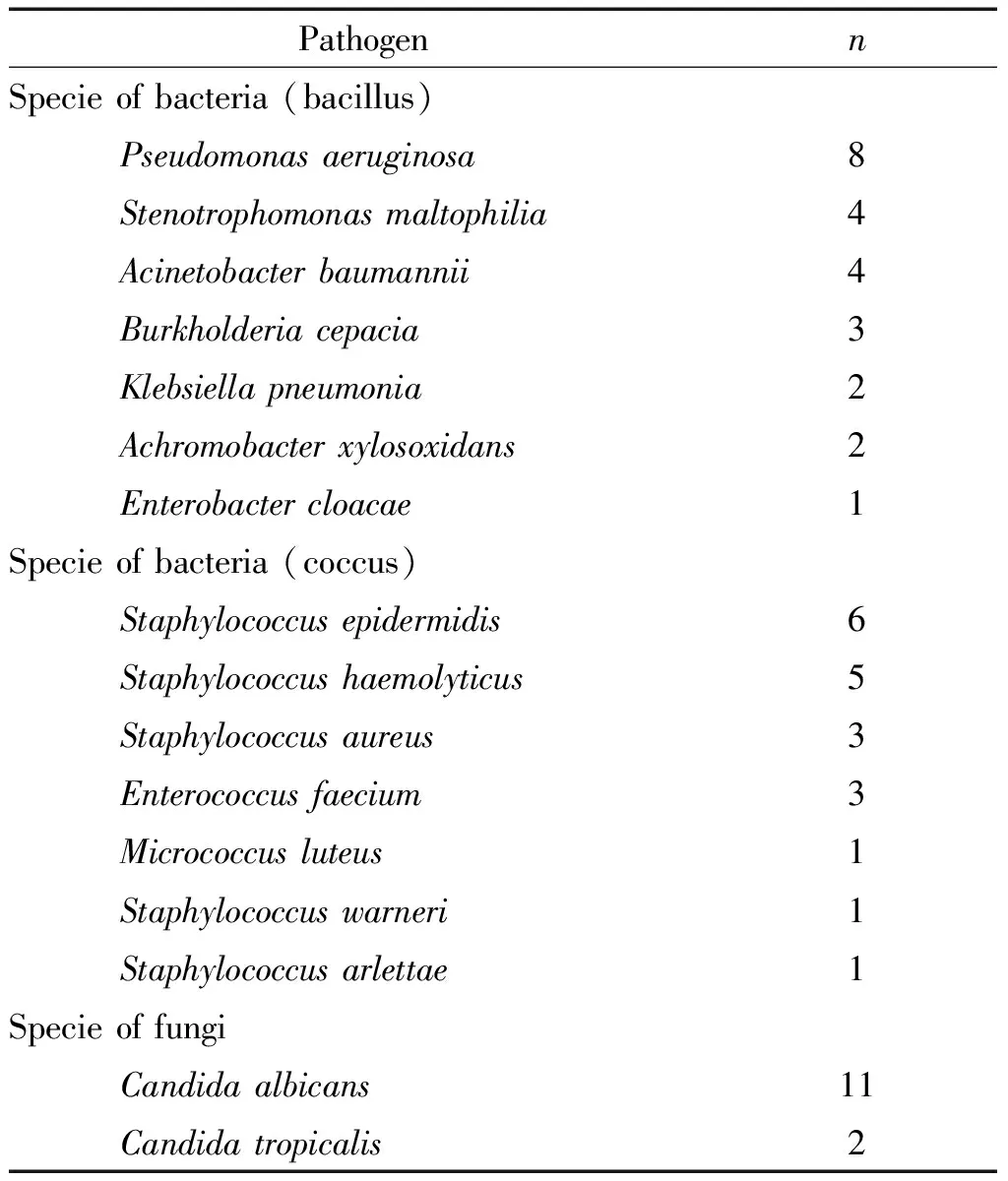
Table 4.The pathogens detected in the patients with postoperative pneumonia from blood or respiratory secretions
It has been reported that high eosinophil count is associated with reduced mortality, but after 6 months with increased mortality in the patient with symptomatic coronary artery disease[12]. However, in this study we did not determine blood eosinophil count as a predictor of hospital mortality for the patients who underwent CABG surgery. This could be attributed to differences on intervention, observational time point, study design and population. The research mentioned above studied on the patients admitted for elective or urgent PCI. Short- (6 months) and long-term (up to 74 months) mortality was analyzed by Cox regression analysis. However, our study focused on the patients with CABG who had more complex and serious lesions. We analyzed hospital mortality during hospital stay following CABG surgery by multivariate logistic regression analysis.
In accordance with previous studies[13-14], nasogastric tube and mechanical ventilation ≥ 24 h were also identified as independent risk factors for postoperative pneumonia following CABG surgery in our study. Nasogastric tube increases gastric reflux and aspiration which is related to lower respiratory tract infection. Ventilator circuits and humidifiers are important sources of pathogens, and prolonged ventilation increases patients’ exposure to pathogens.
Etiology of postoperative pneumonia following CABG surgery in our study is similar to that of hospital acquired pneumonia in other study[15]. It should be noted that most cases ofCandidaalbicanswere mixed infection with bacterial microbes in this study and it might not be the main pathogen of pneumonia.
There were limitations in our study. First, it was a retrospective study in a single center. The results may not be applied to other institutes. In addition, the sample size is relatively small, so it may be deficient to detect minor difference. Furthermore, we excluded the patients with parasitic infection by parasite egg count in stool routine, which may lead to missed diagnosis. Therefore, a multicenter prospective study should be implemented to analyze the relationship between low blood eosinophil count and risk of pneumonia in the general population.
In conclusion, we determined in this retrospective cohort study that low blood eosinophil count was associated with increased risk of postoperative pneumonia following CABG surgery. More study should be conducted to such group and effective strategies could be taken to reduce the risk of postoperative pneumonia.
