Neuroprotective and neuroregenerative potential of pharmacologically-induced hypothermia with D-alanine D-leucine enkephalin in brain injury
2018-01-13GrantLiskaMarciCrowleyJulianTuazonCesarBorlongan
M. Grant Liska, Marci G. Crowley, Julian P. Tuazon, Cesar V. Borlongan
Center of Excellence for Aging and Brain Repair, University of South Florida College of Medicine, Tampa, FL, USA
Abstract Neurovascular disorders, such as traumatic brain injury and stroke, persist as leading causes of death and disability – thus, the search for novel therapeutic approaches for these disorders continues. Many hurdles have hindered the translation of effective therapies for traumatic brain injury and stroke primarily because of the inherent complexity of neuropathologies and an inability of current treatment approaches to adapt to the unique cell death pathways that accompany the disorder symptoms. Indeed, developing potent treatments for brain injury that incorporate dynamic and multiple disorder-engaging therapeutic targets are likely to produce more effective outcomes than traditional drugs. The therapeutic use of hypothermia presents a promising option which mayfit these criteria. While regulated temperature reduction has displayed great promise in preclinical studies of brain injury, clinical trials have been far less consistent and associated with adverse effects, especially when hypothermia is pursued via systemic cooling. Accordingly,devising better methods of inducing hypothermia may facilitate the entry of this treatment modality into the clinic. The use of the delta opioid peptide D-alanine D-leucine enkephalin (DADLE) to pharmacologically induce temperature reduction may offer a potent alternative, as DADLE displays both the ability to cause temperature reduction and to confer a broad profile of other neuroprotective and neuroregenerative processes. This review explores the prospect of DADLE-mediated hypothermia to treat neurovascular brain injuries, emphasizing the translational steps necessary for its clinical translation.
Key Words: stroke; traumatic brian injury; neurodegeneration; temperature management; regenerative medicine;delta opioids; metabolic suppression; cerebrovascular disease; neurovascular disease
Introduction
Brain injuries, such as traumatic brain injury (TBI) and stroke, impose a devastating impact on our healthcare system. Of all injury-related deaths in the US, it was found that 1/3 had a diagnosis of TBI, accounting for roughly 50,000 deaths per year (Abdullah and Husin, 2011; Coronado et al., 2011). Beyond the mortality of TBI, chronic cognitive,behavioral, and functional symptoms can accompany TBI progression, presenting a significant burden to millions of patients suffering the ongoing effects of their injury (Elder,2015). Stroke presents an equally pressing medical concern;as the second leading cause of death worldwide, stroke affects an estimated 795,000 Americans annually (Sacco and Dong, 2014). Similar to TBI, stroke is associated with progressive secondary deficits (Sun et al., 2014). Despite the prevalence of TBI and stroke, therapeutic options are extremely limited for these disorders. Acute TBI treatment is relegated to physiological response management – such as regulation of intracranial pressure (ICP) and fever reduction– while chronic patient treatment is comprised mainly of symptom management and rehabilitation therapy (Haddad and Arabi, 2012). Ischemic stroke has a single Federal Drug Administration (FDA)-approved treatment – recombinant tissue plasminogen activator (tPA) – yet this treatment option is crippled by a narrow therapeutic window which inhibits its use on a large scale (Frey, 2005). Moreover, while tPA encourages reperfusion to ischemic tissue, it is not effective in promoting the recovery of already-damaged tissue.Thus, a pressing clinical need exists for therapeutics which can aid in the protection of neural tissue from brain injury and/or promote neuroregenerative processes which facilitate functional recovery.
The inherent complexity of neuropathologies have plagued the development of effective therapies for brain injury; TBI and stroke – as with many neurological disorders –are associated with dynamic disorder progression pathways which are not entirely understood (Xu et al., 2011; Pankevich et al., 2014). The signaling pathways which mediate cell death following initial insult are numerous and highly interconnected. Moreover, heterogeneous cell populations,highly interdependent cell-to-cell relationships, and bloodbrain barrier (BBB) interactions combine to make effective drug development challenging. This has been made evident in clinic trials, where the numerous attempts to translate effective therapies for brain injury have been largely unsuccessful, especially when using simple receptor-ligand drug approaches (Furlan, 2012; Chollet et al., 2014). The majority of these failed drugs were inadequate in their ability to offer dynamic therapeutic profiles that target acute, sub-acute,and chronic pathology, which is likely a prerequisite for ini-tiating truly robust recovery from brain injury.
As a result, developing treatment options which both prevent neural death and facilitate sustained neuroregeneration will likely require us to use innovative intervention techniques which move past traditional drug-development paradigms. The regulated use of hypothermia has been proposed as one such therapeutic modality. A large body of preclinical evidence supports the potential of temperature reduction in promoting recovery from brain injury (for review in TBI,see Choi et al. (2012), for review in stroke, see Yenari and Han (2013)), yet its widespread use has been hindered by inconclusive clinical trials (Peterson et al., 2008; Dumitrascu et al., 2016). Alternative methods of reducing body temperature, such as pharmacological agents, might offer a superior approach. Of particular interest, the synthetic opioid D-alanine D-leucine enkephalin (DADLE) may be more effective in its ability to confer neuroprotection and neuroregeneration within a clinical setting. In this review, we will begin by discussing specific aspects of TBI and stroke pathology which are amenable to the therapeutic mechanisms of hypothermia. Then, we will review the stand-alone merits of therapeutic hypothermia before discussing the advantages of alternative hypothermia-inducing agents such as DADLE for reducing body temperature. Finally, we will review the various neuroprotective mechanisms of DADLE which may contribute to sustained functional recovery after brain injury independent of its hypothermic effects.
Brain Injury Pathology – Why Does Hypothermic Induction Make Sense?
TBI and stroke have many post-injury cell death mechanisms in common, and thus the therapeutic research into one disorder state is often times applicable to the other(Sayeed and Stein, 2009; Albert-Weissenberger et al., 2013;Prakash and Carmichael, 2015). Immediately following TBI,a necrotic core is formed which is not subject to therapeutic preservation. Stroke results in an ischemic core which develops more gradually as the oxygen and nutrient deprivation lead to primary energy failure – but it is too generally unamenable to intervention unless delivered extremely quickly.Acute cellular injury mechanisms following TBI and stroke include energy failure, excitotoxicity, free radical generation, mitochondrial disruption, and BBB damage (Werner and Engelhard, 2007; Mărgăritescu et al., 2009; Sierra et al., 2011; Xing et al., 2012a); these precipitate secondary injury cascades such as an upregulation of pro-inflammatory mediators, decreased trophic factors, and more widespread BBB perturbations (Siesjo and Siesjo, 1996; Werner and Engelhard, 2007). Sub-acute and chronic pathology of TBI and stroke are defined by an ongoing inflammatory response which contributes to progressive cell death (Arvin et al., 1996; Jin et al., 2010). Halting the outward expansion of cell death and aberrant inflammation from the initial injury are effective means of improving patient outcomes for both TBI and stroke. Apparent from completed clinic trials on neuroprotective agents is the necessity of “multi-pronged”therapeutic strategies which target multiple injury mechanism listed above, as single receptor-ligand approaches have been largely unsuccessful in delivering significant functional recovery.
Non-traditional intervention modalities such as hypothermia are successful in targeting broad pathology mechanism,conferring neuroprotection by modulating the numerous temperature sensitive injury mechanisms (i.e., excitotoxicity, free radical generation, neuroinflammation, and apoptosis) (Dietrich and Bramlett, 2016). In addition to its neuroprotective roles, accumulating evidence suggests that hypothermia may also confer neuroregenerative benefits(Silasi and Colbourne, 2011). Furthermore, by slowing the physiological rate of pathological progression, hypothermia and metabolic suppression may exist as effective adjunctive therapies by artificially extending the intervention time window (Karnatovskaia et al., 2014). Later sections will outline therapeutic hypothermia’s neuroprotective and neuroregenerative properties.
Regulated Hypothermia – Indications for ItsTherapeutic Potential in Brain Injury
The concept of therapeutic body cooling for neuroprotection dates back to the 1940’s (Fay and Susman, 1945). The ability of an acute reduction in body temperature to provide therapeutic benefits has been supported by ample preclinical evidence, particularly in encouraging the preservation of neurological function during times of ischemia/hypoxia. Indeed, various experimental models of brain injury including focal TBI, diffuse TBI, transient global ischemia, focal ischemia, and hemorrhagic stroke have shown responsiveness to therapeutic hypothermia, with corroborating in vitro studies(Celik et al., 2006; Kim et al., 2013b; Liu et al., 2013, 2016;Wei et al., 2013; Jia et al., 2014, 2015; Li et al., 2015b; Sun et al., 2015; Lee et al., 2016). Complimenting this, various studies have demonstrated that even mild increases in body temperature following experimental injury can exacerbate pathology and heighten histopathological and behavioral abnormalities (Fischer and Beckey, 1990; Wang et al., 2009;Meng et al., 2012). Hypothermia is now employed by many healthcare institutions globally for conditions such as after cardiac arrest, neonatal hypoxic-ischemic encephalopathy,and for certain neurosurgical maneuvers (Shankaran et al.,2012b; Kitagawa et al., 2016).
Acute neuroprotective effects of hypothermia
A reduction in body temperature acutely following brain injury poses diverse therapeutic effects. Chief among these is a reduction in ICP, especially following TBI; vasoconstriction in response to the decreased temperature cause a reduction in cerebral blood flow, thus lowering injury-induced hypertension (Flynn et al., 2015). Increased ICP is highly correlated with worse outcomes (Lafrenaye et al.,2014), and regulation of cerebral hypertension is a priority in the acute treatment of patients with brain injury (Bullock and Povlishock, 2007; Jain et al., 2009). Furthermore, hypo-thermia induces a reduction in cerebral metabolism at an estimated 8% per degree Celsius, reducing the energy needs of vulnerable neurons and making them less susceptible to energy failure (Saigal et al., 2015). This is applicable to both the peri-infarct neurons in the ischemic brain, and neurons within the TBI brain which are affected by the diffuse hypoxia associated with post-traumatic micro-ischemias(Veenith et al., 2016).
Additionally, hypothermia acts to moderate the acute inflammatory response following brain injury, reducing cerebral interleukin (IL)-1β, IL-12, IL-23, and tumor necrosis factor-alpha (TNF-α) levels, decreasing expression of the reactive M1 microglial phenotype, and reducing the number of circulating lymphocytes (Stamm et al., 1985; Zhang et al.,2008; Lee et al., 2016). Moreover, gene array analysis after stroke showed genetic alterations in inflammatory genes like osteopontin, early growth response-1, and macrophage inflammatory protein-3alpha (Ohta et al., 2007). While the acute inflammatory immune response is recognized as neuroprotective, hypothermia may dampen its intensity, thereby lessening its contribution to the neurodegeneration seen in the sub-acute and chronic pathological phases (Gundersen et al., 2001). Other molecular mechanism of hypothermia includes a reduction in matrix metalloprotein-9 (MMP-9), a protein associated with BBB dysfunction and the promotion of brain edema, as demonstrated in preclinical models of TBI and stroke (Wagner et al., 2003; Truettner et al., 2005;Jia et al., 2010). Additionally, modest reductions in body temperature lessen the generation of reactive species and attenuate excitotoxicity – two processes associated with widespread neural damage – if administered very acutely(Dietrich and Bramlett, 2016). In all, a reduction in ICP,decreased metabolic demand, attenuated inflammatory response, preservation of BBB integrity, and multiple molecular mechanisms help in minimizing the initial damage of brain injury and reducing the damage deficit which neuroregenerative therapies must overcome.
Neuroregenerative Effects of Hypothermia
In contrast to neuroprotective strategies which aim to prevent the death of vulnerable cells, neuroregenerative processes enhance signaling pathways, promoting the reorganization and reformation of damaged tissue (Mueller et al., 2009). Intervening in the acute phase post-brain injury with neuroprotective therapies is the most effective way to minimize the development of severe neurological deficits.Substantial functional recovery, however, will likely necessitate a biphasic approach, wherein neuroprotective mechanisms are exerted in the acute phase and neuroregenerative cascades are also initiated which help sustain functional recovery throughout disorder progression by combating degenerative processes.
Basic science efforts have demonstrated that in addition to the more intuitive neuroprotective effects of therapeutic hypothermia on brain injury, this treatment modality also promotes diverse neuroregenerative pathways. Neurotrophic factors are a driving force behind neural survival,function, differentiation, and regeneration. Thus, studies reporting increased levels of brain-derived neurotrophic factor (BDNF) (Vosler et al., 2005), nerve growth factor(NGF) (D’Cruz et al., 2002), glial-derived neurotrophic factor (GDNF) (Schmidt et al., 2004), neurotrophin (Husted and Andreasen, 1976), and vascular endothelia growth factor (VEGF) (Li et al., 2017) may be favorable indicators of hypothermia’s neuroregenerative properties. Following ischemia and TBI, endogenous reparative efforts include a rise in neurogenesis within the subventricular zone and subgranular zone of the hippocampus (Jin et al., 2006; Zheng et al., 2013). Treatments which support this endogenous repair process are appealing, seeing that the brain’s inherent capacity to enhance neurogenesis is supportive, but insuffi-cient, for substantial recovery (Marlier et al., 2015). Multiple studies have reported therapeutic hypothermia as enhancing neurogenesis (Kuo et al., 2010; Silasi and Colbourne, 2011;Xiong et al., 2011; Bregy et al., 2012; Silasi et al., 2012), as well as reducing apoptosis of newborn cells (Chen et al.,2016). In fact, a reduction in apoptosis has been proposed as the primary mechanism explaining how therapeutic cooling could cause the observed increase in surviving newborn neurons (Yenari and Han, 2013); reductions in pro-apoptotic proteins Bcl-2, activated Cas3, FasL, Fas, and SMAC (second mitochondria-derived activator of caspases) complex have been found to result even mild hypothermic treatment(Li and Wang, 2011; Xiong et al., 2011; Chen et al., 2016).In addition to prevent newborn apoptosis, this widespread reduction in pro-apoptotic factors has a protective effect on vulnerable mature neurons throughout the affected tissue.
The existence of living neurons does little to promote functional recovery unless concurrent synaptogenic, axonogenic, and neuroplastic processes promote their network integration (Emsley et al., 2004). While the amount of research regarding hypothermia’s effects on synaptogenesis and axon outgrowth is small, some studies have reported promisingfindings; investigations with organotypic brain slices found that deep hypothermia at 17°C was associated with an upregulation in neurite outgrowth (Schmitt et al., 2010), while a separate study found drastic changes in the hippocampal expression profile of genes related to synapses organization and biogenesis in TBI rats treated with hypothermia (Feng et al., 2010). These studies suggests an important, albeit incompletely-verified, role of hypothermia in promoting axonal outgrowth, synaptic formation, and possibly repairing network connectivity.
Glial cells are increasingly recognized as a pivotal component to the proper function of neurons (Xing et al.,2012b). A deep understanding of how hypothermia affects cell types such as astrocytes and oligodendrocytes has yet to be reached. However, oligodendrocyte death and white matter degeneration are closely associated with worse outcomes after brain injury (Lotocki et al., 2011; Johnson et al.,2013). Indeed, white matter preservation/regeneration is critical to maintaining healthy brain functional in humans(Fields, 2008). Hypothermia has been shown in vitro to promote oligodendrocyte precursor cell survival compared to normothermic conditions (Imada et al., 2010), while an in vivo study reported a decrease in oligodendrocyte death following fetal hypoxic insult when treated with hypothermia (Bennet et al., 2007). Concerning astrocytes, increases in connexin 43 – the predominant protein component of astrocytic gap junctions – have been shown to be associated with the pathophysiology of TBI, especially within the CA1 and CA2 regions of the hippocampus (Li et al., 2015b). One study using a weight-drop model of TBI found that mild hypothermia was able to normalize connexin 43 levels (visualized Immunohistochemically in astrocytes) as well as reduce brain edema (Li et al., 2015b). Reduction in connexin 43 activity has similarly been found to be neuroprotective in models of ischemic brain injury (Li et al., 2015a). Hypothermia has also been demonstrated to affect specific glial protein signaling pathways which contribute to its neuroprotective effects (Kim et al., 2013a).
By reducing the occurrence of apoptosis in vulnerable neurons, glial cells, and immature precursor cells, hypothermia may be able to both preserve existing brain tissue as well as sustain endogenous repair mechanisms. Numerous supportive processes may promote these regenerative efforts,such as increased angiogenesis, which has been demonstrated in multiple models of neural injury (Xie et al., 2007; Kuo et al., 2010; Kao et al., 2011). Taken together, the neuroregenerative benefits of hypothermia are likely to contribute to the notable sustained improvements seen in preclinical brain injury models and in select clinical trials.
Clinical Trials of Hypothermia – Room for Improvement
Clinical trials of therapeutic hypothermia for the sake of neurological injury began before the turn of the twenty-first century (Schwab et al., 1999) and many trials remain ongoing at the present time. While induced hypothermia is a common practice in the clinic, particularly for surgical application (Hypothermia after Cardiac Arrest Study, 2002),it has not yet been FDA-approved for the treatment of neurological disorders. Numerous studies have attempted to use purposeful and controlled hypothermia as a therapy after TBI and stroke with contradictory results.
Subsequent to severe TBI, hypothermia treatment improved patient outcomes in several studies (Clifton et al.,2002; Lee et al., 2010; Yan et al., 2010; Flynn et al., 2015).Therapeutic hypothermia has been reported to be more effective in severe TBI than mild to moderate TBI (Yan et al., 2010), and is known to effectively reduce ICP (Lee et al., 2010). However, not all clinical trials concluded with such promising outcomes. One trial reported no significant difference between hypothermia treatment and traditional therapy (Clifton et al., 2011); another trial presented evidence that hypothermia actually worsened patient outcomes in TBI (Andrews et al., 2015). Efficacy of therapeutic hypothermia for TBI in younger patients is also up for debate.For example, one study found treatment to be effective in young patients with evacuated mass lesion (Suehiro et al.,2015), yet another found no improvements after hypothermia for pediatric TBI (Beca et al., 2015).
Clinical trials for therapeutic hypothermia in stroke/ischemia have reached similarly uncertain results. Positivefindings included the presence fewer infarctions in neonatal hypoxic-ischemic encephalopathy (Rutherford et al., 2010;Shankaran et al., 2012a), improved outcomes in both hemorrhagic (Abdullah and Husin, 2011), and ischemic stroke patients (van der Worp et al., 2014), and reduced “poor outcomes” after thrombolysis (Piironen et al., 2014). It was also reported that inducing hypothermia in patients with massive cerebral hemispheric infarction did not significantly improve mortality, however, treatment groups displayed improved neurological functions compared to the non-treated group (Su et al., 2016). When compared to patients treated with tPA alone, there was no added improvement with hypothermia and tPA co-treatment (Bi et al., 2011).
Apparent from these clinical trials is the unpredictability of hypothermic treatment in brain injury. In addition to the variations seen between patients of the same brain injury classification, opposing outcomes may be attributed to the fact that the majority of the clinical trials had unique protocols. Therapeutic hypothermia procedures may differ in many aspects including time point after injury, duration under hypothermia, severity of hypothermia, rate of cooling and warming, and local versus widespread hypothermia. Understanding how these differences effect patient outcomes to optimize therapeutic use of hypothermia will be imperative to establish this form of therapy as a treatment for neurological insults. Few studies have already looked into to such comparisons such as a severe TBI clinical trial that reported five days of hypothermia was more effective than 2 days(Jiang et al., 2006). Another study found that hypothermia treatment for 24 hours within 6 hours after stroke effectively improved outcomes (van der Worp et al., 2014).
Despite the promising preclinical evidence presented to indicate the potential of traditional hypothermia in TBI and stroke, pharmacological means of reducing body temperature may be superior in their ability to be applied quickly and consistently, possibly facilitating the therapeutic effects of temperature reduction.
Drug-Induced Hypothermia and D-Alanine D-Leucine Enkephalin
Traditional means of inducing hypothermia include surface cooling with ice packs, cooling caps or fans, cold-liquid consumption, bypass, or IV lines (Karnatovskaia et al., 2014).Each of these has drawbacks, including the need for sedation to minimize patient discomfort, muscular paralysis to inhibit shivering, or imprecision of temperature management (Karnatovskaia et al., 2014). The use of pharmacological agents is an appealing option as pharmacological agents do not cause the discomfort of surface cooling, can befinely dosed based off of extensive pre-clinical research, and are less likely to induce shivering (Zhang et al., 2013). Furthermore, longterm states of hypothermia are inadvisable; pharmacological means of hypothermia may be more sustainable into the sub-acute and chronic phase of disorder pathology. Similar to conventional methods of therapeutic hypothermia, pharmacologically-induced hypothermia has been shown to exert neuroprotective benefits in models of TBI, hemorrhagic stroke, and ischemic stroke (Wei et al., 2013; Cao et al., 2014;Lee et al., 2014; Gu et al., 2015). A range of drugs have been explored for their propensity to reduce body temperature including cannabinoid agonists (Rawls et al., 2002), ion channel agonists (Muzzi et al., 2012), neurotensin receptor agonist(Wei et al., 2013), helium gas (Berganza and Zhang, 2013),endogenous metabolites (Panas et al., 2010), and delta opioid agonists (Sanchez and Arnt, 1992). Among these, opioid agonist are especially promising candidates due to their history of clinical applications and their extensive preclinical record of affording potent neuroprotection (Zhang et al., 2002;Rosenblum et al., 2008; Zhu et al., 2009; Staples et al., 2013).
The synthetic delta opioid agonist DADLE has demonstrated therapeutic efficacy in neuropathologies (Borlongan et al., 2000, 2001, 2009). Despite DADLE being known to induce metabolic suppression and hibernation-like states,its direct effect on body temperature was unknown until recently. DADLE was administered to uninjured rats, inducing a decrease in body temperature from an average of 37°C to 34°C after 90 minutes, verifying its ability to pharmacologically induce hypothermia (Zhang et al., 2013). Importantly, DADLE has been shown to afford neuroprotection in the absence of hypothermia (i.e., with experimental protocols which maintained temperature at 37°C (Su et al.,2007; Zheng et al., 2012). This indicates that DADLE, in addition to exerting the dynamic therapeutic effects associated with hypothermia, retains the ability to confer the broad neuroprotective properties which will be discussed in the following section. While it is intuitive that a hypothermic state induced by DADLE would confer the same neuroprotective effects as traditional hypothermia, it is essential that experiments are conducted to independently verify this. As therapeutic hypothermia’s neuroprotective capacity has already been demonstrated in the clinic, pharmacological induction of hypothermia with DADLE may present a means of heightening this treatment modality’s safety, effectiveness,precision, and long-term sustainability in patients.
Beyond Hypothermia – AdditionalTherapeutic Benefits of D-Alanine D-Leucine Enkephalin
DADLE is unique in its ability to provide neuroprotection in the most acute phases of disease through the hypothermic mechanisms discussed thus far, while also utilizing multipronged neuroprotective and neuroregenerative mechanisms to sustain therapeutic effects throughout disorder progression. This is of great value, as the complexity of traumatic lesions may necessitate treatment strategies that are initiated shortly after injury and maintained for extended durations. Indeed, drug-induced hypothermia with DADLE could target both acute, sub-acute, and chronic neuronal injury cascades, facilitating robust functional recovery. DADLE exerts therapeutic effects both by receptor-mediated pathways via the delta opioid receptor (DOR – recently termed DOP) and receptor-independent mechanisms. These mechanisms are diverse, and much progress has been made in understanding the details and signaling pathways which underlie DADLE’s benefits mediated both by DOR activation and independent of DOR.
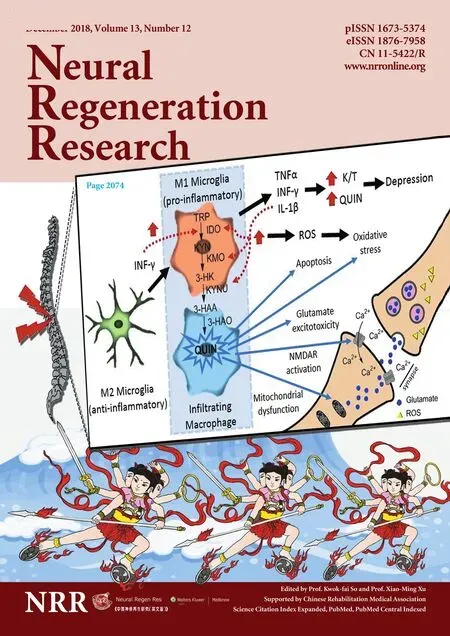
DADLE has been most recognized for its ability to confer neuroprotection following ischemic stroke (Crowley et al.,2017), yet its applicability to other neurological disorders such as TBI is intriguing. In the acute phase of brain injury, stimulation of DORs decreases K+leakage attenuates Ca2+dysregulation, and inhibits glutamate release – three processes associated with initial depolarization and loss of ionic homeostasis (Chao et al., 2009; Chao and Xia, 2010).Furthermore, DOR activation reduces Na+influx by modulation of voltage-gated Na+channels and inhibiting N-methyl-D-aspartate (NMDA) receptors (Chao et al., 2009; Chao and Xia, 2010) offering neuroprotection via presynaptic(inhibition of glutamate release) and postsynaptic (Na+voltage-gated channels and NMDA receptors) mechanisms(Borlongan et al., 2004; He et al., 2013). Mitochondrial dysregulation is increasingly recognized as a pivotal contributor to post ischemic and post-TBI (Sims and Muyderman,2010; Cheng et al., 2012). DADLE may exert DOR-mediated anti-oxidant effects (Tsao et al., 1998; Maslov and Rebrova,2000), helping to abrogate the oxidative stress-induced mitochondrial instability which follows brain injury (Zhu et al.,2009). DOR activation with DADLE displays anti-inflammatory effects which seem to occur via modulation of pro-infl ammatory cytokines such as TNF-α, IL-1β, IL-6 (Wang et al., 2014), and upregulated secretion of anti-inflammatory cytokines such IL-4, and IL-13 (Shrivastava et al., 2017).
Neuroregenerative and anti-apoptotic properties have also been linked to DADLE treatment (Zheng et al., 2012;Zhang et al., 2013). DOR activation with DADLE has been shown to enhance neural survival in models of brain injury (Zhang et al., 2000; Borlongan et al., 2009), possibly via a novel signal transducer and activator of transcription(STAT)5B-G protein signaling pathway reported to underlie the increase in neural survival, neurite outgrowth, and differentiation associated with DOR activation (Pallaki et al.,2017). Moreover, in a recent study using a transient global ischemia stroke model, intracerebral injection of DADLE increased cell proliferation within the CA1 region and enhanced neuronal differentiation within the hippocampus 28 days post-injury, resulting in marked improvements in spatial memory (Wang et al., 2016). Finally, DADLE has been revealed to increase NGF – known to have neuroregenerative effects (Zhou et al., 2003; Fantacci et al., 2013) – via the P13K/Akt and MAPK signaling pathways (Sen et al., 2013).While the acute protective mechanisms of DADLE are well known, it is also evident that the present literature supports a potentially potent role of DADLE in encouraging neuroregeneration. Further verification and increased understanding of these therapeutic properties are necessary though, and will require extensive basic science research.
Future Directions in Translating D-Alanine D-Leucine Enkephalin for Treating Neurological Disorders
Translating pharmacologically-induced hypothermia with DADLE into the clinic for brain injury will require a number of practical pharmacological protocols to be addressed.Most important will be determining the appropriate dosage,optimal time of administration, and number of treatments which best facilitate safe and effective functional recovery.Indeed, the data from the clinical trials discussed previously suggest that the efficacy of treatment depends on the time of initiation following injury, duration, depth of temperature drop, and warming protocols (or drug tapering protocols,in the case of pharmacologically-induce hypothermia). Additionally, a better understanding of the effects of factors such as age and injury severity should also be investigated,as clinical trials have seen differential effects of hypothermic treatment with respect to these factors (Yan et al., 2010; Suehiro et al., 2015).
Other clinically-relevant concerns include the immunosuppressive nature of body temperature reduction; even moderate sustained drops in body temperature have been shown to increase the likelihood of developing infections,which may pose a serious threat to patient who are already immunocompromised (Geurts et al., 2014). Furthermore,as DADLE is known to have non-specific interactions, its unique biological behavior should be explored.
Translating DADLE into the clinic will also require a better understanding of how exactly it confers its therapeutic effects, as discussed above. The various studies which have reported DADLE’s neuroprotective properties have inconsistently accounted for body temperature; as such, it is diffi-cult to discern exactly which neuroregenerative mechanisms of this opioid agonist are dependent on its hypothermic effects, and those which are a result of DOR signaling or other biological interactions. Basic science efforts to better understand the processes which underlie DADLE’s therapeutic effects will be essential to designing ideal treatment plans which appropriately utilize its dynamic mechanisms.The use of DADLE in combination with other therapeutic agents is also an intriguing area of potential research. As discussed earlier, neuropathology is notoriously resistant to simple receptor-ligand style treatments, and thus DADLE’s efficacy may be enhanced with adjunctive therapy options which target complimentary cell death pathways.
Conclusion
Neurological disorders such as stroke and TBI are extremely limited in their available therapeutic options. This unmet clinical need has resulted from decades of failed clinical trials for these disorders. Traditional drug development approaches using agents which target a single pathological mechanism are unlikely to provoke substantial recovery due to the complexity of disorder progression and neurodegeneration which accompanies these neurovascular injuries.TBI and stroke share many features during disorder progression such as chronic neuroinflammation, BBB breakdown,mitochondria dysfunction, and buildup of reactive species -events which collectively precipitate to secondary cell death and chronic deficits. Therapeutic hypothermia represents an innovative treatment technique that is able mitigate neurodegeneration on multiple fronts, potentially overcoming the limitations of traditional drugs. Induced hypothermia offers diverse neuroprotective benefits such as suppressing the immune response and reducing metabolic demands. Additionally, evidence exists that hypothermia promotes neurogenesis,neurite outgrowth, and synaptogenesis. The inconclusive results of completed clinical trials using hypothermia, however, suggest that room for improvement exists in how this therapy is administered. An intriguing approach which may offer unique benefits is to utilize drug-inducible hypothermia as an alternative treatment modality. The compound DADLE – a synthetic delta opioid and metabolic suppressant– has already shown promise as a therapy for neurological injuries independent of its hypothermia-inducing properties.Thus, DADLE is unique in its capacity to provide effective temperature reduction as well as supplementary therapeutic mechanisms such as preservation of ionic homeostasis, antioxidant effects, and anti-inflammation. This dynamic therapeutic profile of DADLE may allow for the clinical potential of hypothermia to be harnessed toward promoting functional recovery in patients suffering from TBI or stroke.
Author contributions:Manuscript concept: CVB; literature search and initial manuscript preparation: MGL and MGC; critical revision and final approval of the manuscript: JPT and CVB.
Conflicts of interest:The authors declare no conflicts of interest.
Financial support:The work was supported by NIH R01NS071956, NIH R01 NS090962, NIH R21NS089851, NIH R21 NS094087, DOD W81XWH-11-1-0634, and VA Merit Review I01 BX001407 (to CVB).
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-Non-Commercial-ShareAlike 4.0 License, which allows others to remix,tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
杂志排行
中国神经再生研究(英文版)的其它文章
- Huangqinflavonoid extraction for spinal cord injury in a rat model
- Lithium promotes recovery of neurological function after spinal cord injury by inducing autophagy
- Analysis of transcriptome sequencing of sciatic nerves in Sprague-Dawley rats of different ages
- Exogenous brain-derived neurotrophic factor attenuates cognitive impairment induced by okadaic acid in a rat model of Alzheimer’s disease
- Partial improvement in performance of patients with severe Alzheimer’s disease at an early stage of fornix deep brain stimulation
- Epigenetic marks are modulated by gender and time of the day in the hippocampi of adolescent rats:a preliminary study