替罗非班对急性ST段抬高型心肌梗死合并2型糖尿病患者的影响
2017-12-15肖立运李秀丽
肖立运,李秀丽
替罗非班对急性ST段抬高型心肌梗死合并2型糖尿病患者的影响
肖立运1,李秀丽1
目的分析替罗非班对急性ST 段抬高型心肌梗死(STEMI)合并2型糖尿病(T2DM)患者的影响。方法选取金乡县人民医院心内科于2012年1月~2014年1月收治的STEMI合并T2DM患者524例,其中男性310例,女性214例,年龄35~78(55.7±11.8)岁。所有患者随机分成A组(262例)和B组(262例)。两组均行急诊PCI,A组置入支架,B组在A组基础上指引导管局部注入替罗非班,术后维持24 h。心肌梗死溶栓治疗(TIMI)血流分级和校正的TIMI帧数(cTFC)评价再灌注情况。心电图测定ST段回落情况。术后2 h测定心肌肌钙蛋白I(cTnI)、肌酸激酶同工酶(CK-MB)、肌红蛋白。术前和术后3 d测定白介素-6(IL-6)、C-反应蛋白(CRP)、脑钠肽(BNP)。两组术后1周、6个月、1年心脏超声测定左室射血分数(LVEF)、左室收缩末期容积(LVESV)、左室舒张末期容积(LVEDV)。记录术后1个月内出血事件及主要不良心血管事件(MACE)。结果与A组比较,B组术后慢血流、无复流比例减少,TIMI 3级慢、快血流比例增加,差异有统计学意义(P均<0.05)。与A组比较,B组CKMB、cTnI以及肌红蛋白水平下降,ST段回落比例增加,差异有统计学意义(P均<0.05)。两组术后较术前CRP、IL-6以及BNP均升高,而A组升高更明显,差异有统计学意义(P均<0.05)。A组与B组术后1周LVESV、LVEDV、LVEF比较,差异无统计学意义(P均>0.05)。术后6个月、术后1年B组较A组LVESV、LVEDV减少,LVEF增加,差异有统计学意义(P均<0.05)。B组出血48例,A组出血27例,两组出血率比较(18.3% vs. 10.3%),差异无统计学意义(P>0.05)。A组MACE发生率高于B组(11.8%vs. 1.5%),差异有统计学意义。结论STEMI合并2型糖尿病患者急诊PCI术中应用替罗非班可明显改善术后冠状动脉血流情况,减轻心肌损伤和炎症反应,提高心功能,安全性高。
急性ST段抬高型心肌梗死;盐酸替罗非班;经皮冠状动脉介入术;无复流;2型糖尿病
急性ST段抬高型心肌梗死(STEMI)合并2型糖尿病(T2DM)患者多为老年人,且存在冠状动脉弥漫性病变,多支病变[1]。患者症状多不典型,发病隐匿,斑块破裂导致急性血栓。经皮冠状动脉介入治疗(PCI)大大提高了STEMI合并T2DM患者的生存率,但此类患者PCI术中或术后易出现慢血流甚至无复流,影响心肌再灌注,导致治疗效果差,预后不良等[2]。替罗非班为血小板糖蛋白(GP)Ⅱb/Ⅲa受体拮抗剂,有助于减少急诊PCI术中的冠状动脉血栓负荷和继发的远端微循环栓塞。本研究在PCI术中局部注入盐酸替罗非班,观察其对STEMI合并T2DM患者冠状动脉血流和炎症因子等影响。
1 资料与方法
1.1 研究对象与分组
选取金乡县人民医院心内科于2012年1月~2014年1月收治的STEMI合并T2DM患者524例,其中男性310例,女性214例,年龄35~78(55.7±11.8)岁。入选标准:①符合STEMI诊断标准,且符合急诊PCI指征;②符合1997年美国糖尿病协会提出的T2DM诊断标准;③接受急诊PCI。排除标准:有急诊PCI禁忌症;冠状动脉造影(CAG)显示左主干或多支病变;严重心肌梗死后心力衰竭(Killip分级≥Ⅲ级);严重糖尿病患者(糖尿病酮症酸中毒、高渗性昏迷、低血糖);血小板减少症和(或)血小板增多症。所有患者随机分成A组(262例)和B组(262例)。两组性别、年龄、吸烟比、肥胖、血压水平、血脂水平等方面比较,差异均无统计学意义(P均>0.05),具有可比性。
1.2 方法
1.2.1 治疗方法A组和B组术前常规给予阿司匹林300 mg、氯吡格雷600 mg负荷量。经桡动脉途径穿刺,置入支架。术后常规给予双联抗血小板治疗,拜阿司匹林0.1 mg/d,氯吡格雷75 mg/d,皮下注射低分子肝素钙;口服他汀类药物,如无禁忌症,常规服用β受体阻滞剂及ACEI或ARB;血糖控制:治疗期间均控制饮食,血糖明显偏高者给予短效胰岛素,血糖维持在6.1 mmol/L左右。A组:PCI术中血栓负荷较重给予血栓抽吸,再用球囊扩张病变处后置入支架。B组:在A组基础上指引导管局部注入替罗非班(鲁南恒康)10 μg/kg,术后继续0.1 μg/(kg·min)泵入24 h。
1.2.2 慢血流及无复流评价 心肌梗死溶栓治疗(TIMI)血流分级评价再灌注情况:0级(无灌注),1级(渗透而无灌注),2级(部分灌注),3级(完全灌注)。慢血流指PCI后局部冠状动脉远端血液灌注延迟现象,TIMI血流2级;无复流为TIMI血流0级和1级。校正的TIMI帧数(cTFC)计算:由手术者及助手独立进行计帧,以30帧/s计数,cTFC取平均值,cTFC是记录第一帧和最末帧之间的帧数,以造影剂完全接触到冠状动脉起始部血管壁的两侧并开始前向运动作为第一帧,以造影剂进入远端分支血管特定的解剖标志显影为最末帧,前降支较长时TIMI帧数除以1.7得到cTFC;cTFC<40帧为TIMI 1级,<23帧为TIMI 3级快血流,23<cTFC≤40为TIMI 3级慢血流。
1.2.3 心肌损伤和炎症标记物检测 术后2 h采用酶联免疫吸附法,使用雅培AEROSET全自动生化分析仪及配套试剂测定心肌肌钙蛋白I(cTnI)、肌酸激酶同工酶(CK-MB)、肌红蛋白。术前和术后3 d测定白介素-6(IL-6)、脑钠肽(BNP)、C-反应蛋白(CRP)水平。
1.2.4 心电图ST段回落 两组分别于入院时、PCI术后2 h内做常规心电图。ST段抬高以T-P段为等电位线,测量J点后80 ms的ST段抬高电压,单位为mm。ST段抬高指数(ΣSTI)计算方法:每一导联连续三个波群的ST段抬高值相加求其平均值,得到该导联的ST段抬高值,将同一份常规心电图各导联抬高的ST段振幅之和除以该份心电图ST段抬高的导联数的值即为ΣSTI。将直接PCI术后心电图与入院时心电图比较:ΣSTI回落<50%为ΣSTI 无回落,回落≥50%为ΣSTI回落[3,4]。
1.2.5 心脏超声检测和不良反应记录 两组术后1周、6个月、1年心脏超声测定左室射血分数(LVEF)、左室收缩末期容积(LVESV)、左室舒张末期容积(LVEDV)。记录两组患者术后1个月内出血事件及主要不良心血管事件(MACE),包括再次心肌梗死、死亡等。
1.3 统计学处理
采用SPSS 17.0统计软件进行数据分析,计量资料采用均数±标准差(±s)表示,两组间均数的比较采用t检验,计数资料采用例数(构成比)表示,组间比较采用χ2检验。P<0.05为差异有统计学意义。
2 结果
2.1 两组术后冠状动脉血流比较
与A组比较,B组术后慢血流、无复流比例减少,TIMI 3级慢、快血流比例增加,差异有统计学意义(P均<0.05),表1。
2.2 两组心肌损伤标志物比较
与A组比较,B组CK-MB、cTnI以及肌红蛋白水平下降,ST段回落比例增加,差异有统计学意义(P均<0.05),表2。
2.3 两组炎症因子水平比较
两组术后较术前CRP、IL-6以及BNP均升高,而A组升高更明显,差异有统计学意义(P均<0.05),表3。
2.4 两组超声指标比较
A组与B组术后1周LVESV、LVEDV、LVEF比较,差异无统计学意义(P均>0.05)。术后6个月、术后1年B组较A组LVESV、LVEDV减少,LVEF增加,差异有统计学意义(P均<0.05),表4。

表1 两组术后血流情况比较
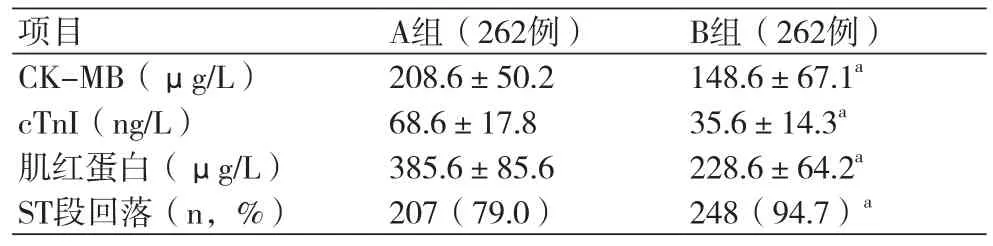
表2 两组患者心肌损伤标志物比较
2.5 出血事件及MACE发生率比较
B组出血48例,A组出血27例,两组出血率比较(18.3%vs.10.3%),差异无统计学意义(P>0.05)。B组死亡3例,再次心肌梗死1例;A组死亡10例,急性血栓形成、心源性休克、再次心肌梗死21例。A组MACE发生率高于B组(11.8%vs. 1.5%),差异有统计学意义(P<0.05)。
3 讨论
替罗非班是高选择性的血小板糖蛋白(GP)Ⅱb/Ⅲa受体拮抗剂,半衰期短,起效快,抑制了血小板最后通路,局部小剂量应用减轻病变部位的血栓负荷,减少术后微血栓发生。本研究中,应用替罗非班的B组较A组无复流现象明显减少,与其他研究结果一致[5,6]。
B组心肌损伤标志物低于A组,且ST段回落率优于A组,可能与其减少微血栓形成,减少慢血流或无复流,改善心肌再灌注,减轻心肌细胞凋亡或坏死有关。CRP、IL-6为重要的炎症因子。本研究中,两组急诊PCI术后炎症因子均有升高,但B组升高幅度较低,这与相关研究相符[7]。
研究表明[8,9],糖尿病合并STEMI患者血小板功能异常,具有较强的粘附性和聚集性,使得血小板表面Ⅱb/Ⅲa受体密度增加,血栓负荷较为严重。本研究中,B组较A组心功能改善明显,与应用替罗非班提高了再灌注水平,保存了大量存活心肌细胞,减少心肌细胞凋亡有关。
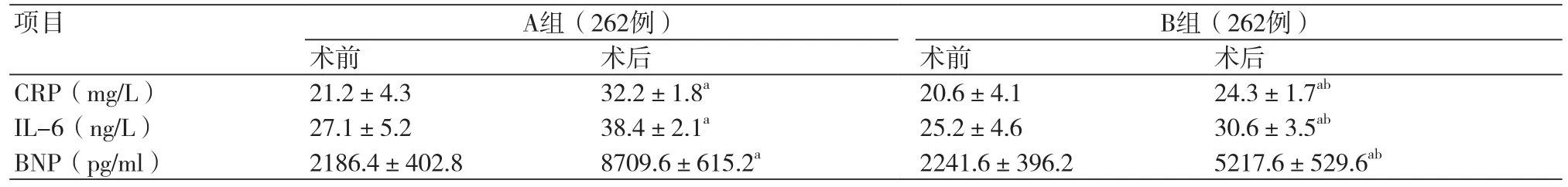
表3 两组PCI前后炎症因子比较

表4 两组不同时间段超声指标比较
观察术后1个月内MACE发生率,发现B组较A组明显减少,且严重出血方面无差异。替罗非班改善冠状动脉血流,有助于进一步改善STEMI合并糖尿病患者微循环,减轻心肌损伤,增加血管内皮细胞介导的扩血管作用[10-13],从而降低MACE发生风险。STEMI合并2型糖尿病患者急诊PCI术中应用替罗非班可明显改善术后冠状动脉血流情况,减轻心肌损伤和炎症反应,进一步提高心功能和改善心室重构,安全性高。
[1]Welsh P,Doolin O,Willeit P,et al. N-terminal pro-B-type natriuretic peoptide and the prediction of primary cardiovascular events:results From 15-year follow-upof WOSCOPS[J]. Eur Heart J,2013,34(6):443-50.
[2]Wang P,Zhang B,Jin L,et al. Association of various risk factors with prognosis and hospitalization cost in Chinese patients with acute myocardial infarction:a clinical analysis of627cases[J]. Exp Ther Med,2015,9(2):603.
[3]Bekkers SC,Yazdani SK,Virmani R,et al. Microvascular obstruction:underlying pathophysiology and clinical diagnosis[J]. J Am Coll Cardiol,2010,55(16):1649-60.
[4]Zencirci AE,Zencirci E,Degirmencioglu A,et al. The relationship Between Gensini score and ST-segment resolution in patients with Acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention[J]. Kardiol Pol,2014,72(6):494-503.
[5]Wang HL,Xing SY,Dong PS,et al. Safety and efficacy of intracoronary tirofiban administration in patients with serious thrombus burden and ST-elevation myocardial infarction undergoing percutaneous coronary intervention[J]. Eur Rev Med Pharmacol Sci,2014,18(23):3690.
[6]刘洋,刘恒亮,耿国英,等. 冠状动脉内注射替罗非班对老年糖尿病急性心肌梗死患者的影响[J]. 中华老年心脑血管病杂志,2013,15(8):799.
[7]Huikuri HV,Stein PK. Heart rate variability in risk stratification of cardiac patients[J]. Prog Cardiovasc Dis,2013,56(2):153-9.
[8]罗艳华. 抗血小板药物对冠心病患者介入术后无复流发生率的影响[J]. 现代医院,2015,15(10):14-5.
[9]Ishihara M,Fujino M,Ogawa H,et al. Clinical Presentation,Management and Outcome of Japanese Patients with Acute Myocardial Infarction in the Troponin Era - Japanese Registry of Acute Myocardial Infarction Diagnosed by Universal Definition (JMINUET)[J]. Circulation,2015,79(6):1255-62.
[10]Ren L,Ye H,Wang P,et al. Comparison of long-term mortality of acute ST-segment elevation myocardial infarction and non- ST- segment elevation acute coronary syndrome patients after percutaneous coronary intervention[J]. Int J Clin Exp Med,2014,7(12):5588.
[11]Hudzik B,Szkodzinski J,Gorol J,et al. Platelet- to- lymphocyte ratio is a marker of poor prognosis in patients with diabetes mellitus and ST-elevation myocardial infarction[J]. Biomark Med,2015,9(3):199.
[12]Ali S,Ussher JR,Baggio LL,et al. Cardiomyocyte glucagon receptor signaling modulates outcomes in mice with experimental myocardial infarction[J]. Mol Metab,2015,4(2):132.
[13]Kunichika H,Ben-Yehuda O,Lafitte S,et al. Effects of glyeoptein Ⅱb/Ⅲa inhibition on microvascular folw after coronary reperfusion. A quantitative myocardial contrast echocardingraph study[J]. Am Coll Cardiol,2004,4(2):276-83.
Influence of tirofiban on patients with acute ST-segment elevation myocardial infarction complicated by type 2 diabetes mellitus
Xiao Liyun*, Li Xiuli.
*Department of Cardiology, People's Hospital of Jinxiang County,Jining 272000, China.
Corresponding author: Xiao Liyun, E-mail: xiaofengxiuli@163.com
ObjectiveTo analyze the influence of tirofiban on patients with acute ST-segment elevation myocardial infarction (STEMI) complicated by type 2 diabetes mellitus (T2DM).MethodsThe patients with acute STEMI complicated by T2DM (n=524, male 310, female 214, aged from 35 to 78 and average age=55.7±11.8) were chosen from the Department of Cardiology of People’s Hospital of Jinxiang County from Jan. 2012 to Jan. 2014. All patients were randomly divided into group A and group B (each n=262). Two groups were given emergency percutaneous coronary intervention (PCI), and group A was given stenting and group B was additionally given local tirofiban injection maintained for 24 h. The reperfusion status was reviewed by using thrombolytic test for myocardial infarction (TIMI) and corrected TIMI frame count (CTFC), and ST-segment resolution was detected by using electrocardiogram (ECG). The levels of cardiac troponin I (cTnI), creatine kinase-MB isoenzyme (CK-MB)and myoglobin (MYO) were detected after the operation for 2 h. The changes of interleukin-6 (IL-6), C-reactive protein (CRP) and brain natriuretic peptide (BNP) were detected before and after the operation for 3 d. The levels of left ventricular ejection fraction (LVEF), left ventricular end-systolic volume (LVESV) and left ventricular enddiastolic volume (LVEDV) were detected by using echocardiogram after the operation for 1 week, 6 months and 1 y.The bleeding events and major adverse cardiovascular events (MACE) were recorded after the operation for 1 month.ResultsThe percentage of patients with slow flow and no reflow decreased, and percentage of patients with slow flow and fast flow of TIMI grade 3 increased in group B compared with group A (all P<0.05). The levels of CK-MB,cTnI and MYO decreased, and percentage of ST-segment resolution increased in group B compared with group A (all P<0.05). The levels of CRP, IL-6 and BNP increased in 2 groups after the operation, which was more significant in group A (all P<0.05). The comparison in LVESV, LVEDV and LVEF had no statistical difference between group A and group B after the operation for 1 week (all P>0.05). LVESV and LVEDV decreased and LVEF increased in group B compared with group A after the operation for 6 months and 1 y (all P<0.05). There were 48 cases of bleeding in group B and 27 in group A (18.3% vs. 10.3%, P>0.05). The incidence of MACE was higher in group A than that in group B (11.8% vs. 1.5%).ConclusionTirofiban administrated during emergency PCI can significantly improve post-operation coronary flow, relieve myocardial injury and inflammatory reactions and promote heart function with higher safety in patients with STEMI complicated by T2DM.
Acute ST-segment elevation myocardial infarction; Tirofiban hydrochloride; Percutaneous coronary intervention; No-reflow; Type 2 diabetes mellitus
R542.22
A
1674-4055(2017)11-1331-03
济宁市科学技术研究“十一五”规划科研启动基金项目B(02201462)
1272000 济宁,金乡县人民医院心内科
肖立运,E-mail:xiaofengxiuli@163.com
10.3969/j.issn.1674-4055.2017.11.11
姚雪莉