血、尿中性粒细胞明胶酶相关脂质运载蛋白与胱抑素C对肝硬化并发急性肾损伤的诊断价值
2017-11-22许长红江坤仁
许长红, 江坤仁
(1 武汉市汉南区红十字会医院 内科, 武汉 430090; 2 武汉市汉南区人民医院 内科, 武汉 430090)
血、尿中性粒细胞明胶酶相关脂质运载蛋白与胱抑素C对肝硬化并发急性肾损伤的诊断价值
许长红1, 江坤仁2
(1 武汉市汉南区红十字会医院 内科, 武汉 430090; 2 武汉市汉南区人民医院 内科, 武汉 430090)
目的检测血、尿中性粒细胞明胶酶相关脂质运载蛋白(NGAL)、胱抑素C(CysC)水平,分析其对肝硬化患者并发急性肾损伤(AKI)的早期诊断价值。方法选择2015年1月-2017年3月于武汉市汉南区红十字会医院就诊的肾功能正常的肝硬化患者236例,依据入院后48 h内是否并发AKI分为AKI组78例,非AKI组158例,选择同期健康体检者100例为对照组。采用ELISA法检测血清NGAL(sNGAL)和尿液NGAL(uNGAL)及血清CysC浓度,并将血肌酐(SCr)浓度和肾小球滤过率(GFR)进行组间比较。计量资料多组间比较采用单因素方差分析,进一步两组间比较采用SNK-q检验;相关分析采用Pearson相关分析法;利用受试者工作特征曲线(ROC曲线)分析相关指标的诊断价值。结果入院48 h,AKI组sNGAL、uNGAL、CysC同非AKI组和对照组相比,差异均有统计学意义(P值均<0.05);将AKI组依照肾损伤标准进行分期,分期高的患者sNGAL、uNGAL浓度显著高于分期低的患者,差异均有统计学意义(P值均<0.05);与入院前比较,入院6 h时sNGAL、uNGAL及CysC水平开始升高,而Scr与GFR入院48 h才开始变化,即sNGAL、uNGAL与CysC开始上升时间明显早于Scr与GFR(P值均<0.05)。AKI组患者sNGAL、uNGAL及CysC浓度与SCr呈正相关(r值分别为0.650、0.681、0.581,P值均<0.05)。ROC曲线示,sNGAL曲线下面积为0.845±0.435,最佳阈值为542.68 μg/L,敏感度为0.824,特异度为0.794;uNGAL曲线下面积为0.836±0.326,最佳阈值为75.12 μg/L,敏感度为0.816,特异度为0.766;CysC曲线下面积为0.818±0.267,最佳阈值为1.48 mg/L,敏感度为0.808,特异度为0.732。结论NGAL与CysC可以作为肝硬化患者发生AKI的早期诊断指标,对了解肝硬化患者的肾功能损伤状况及制订相应措施具有重要意义。
肝硬化; 肾功能不全, 急性; 中性粒细胞明胶酶相关脂质运载蛋白; 胱抑素C; 诊断
失代偿期肝硬化患者可能出现腹水、肝肾综合征、自发性腹膜炎等并发症[1],其中急性肾损伤(acute kidney injure,AKI)是最常见的并发症,主要机制为肾毒性损伤、血流动力学障碍等导致肾小管上皮细胞坏死,最终使肾小球滤过率(GFR)下降[2]。Nadkarni等[3]研究证实,肝硬化患者病死率与AKI具有明显相关性。目前,诊断AKI的敏感性及特异性较高的生物学标志物已有相关报道[4],中性粒细胞明胶酶相关脂质运载蛋白(neutrophil gelatinase-associated lipocalin,NGAL)水平变化可及时反映肾功能情况,尤其在监测肾脏疾病严重程度及治疗方面发挥了至关重要的作用[5]。而胱抑素C(cystatin C,CysC)是反映GFR的特异性及敏感性指标,能早期反映肾功能的真实情况[6]。本研究主要通过收集肝硬化并发AKI患者的临床资料,探讨血、尿NGAL及CysC水平对肝硬化并发AKI的早期诊断价值。
1 资料与方法
1.1 研究对象 选取2015年1月-2017年3月于武汉市汉南区红十字会医院住院治疗的肾功能正常的肝硬化患者。肝硬化的诊断标准[7]:既往有病毒性肝炎病史、大量饮酒等;有肝功能减退及门静脉高压的临床表现;生化检查示Alb下降、血清胆红素升高及PT延长等;B超或CT提示肝硬化或内镜发现胃底静脉曲张;肝活组织检查有肝小叶形成。肝硬化基础上的AKI诊断标准[8]:患者肾功能在48 h内恶化,尿量连续6 h<0.5 ml/kg或血清肌酐(SCr)增至原来的1.5倍或升高绝对值≥26.5 μmol/L(0.3 mg/L)。依据2012年全球肾脏病预后组织(KDIGO)制订的AKI分期标准[9]将AKI分为3期,即1期:SCr升高≥26.5 μmol/L(0.3 mg/L)或升高1.5~1.9倍,且尿量<0.5 ml·kg-1·h-1,时间6~12 h;2期:SCr升高2.0~2.9倍,且尿量<0.5 ml·kg-1·h-1,时间≥12 h;3期:SCr升高≥353.6 μmol/L(4 mg/L)或需要肾脏替代治疗,或患者<18岁,估计GFR降低到<35 ml·min-1·1.73 m-2,或SCr升高≥3倍,且尿量<0.3 ml·kg-1·h-1,时间≥24 h或无尿≥12 h。排除标准:其他疾病引起的AKI,如肝肾综合征、急慢性肾小球肾炎、肾病综合征、泌尿系结石或肿瘤等;伴有脏器功能不全,恶病质或处于急性感染期患者等。选择同期门诊健康体检者作为对照组。本研究经本院医学伦理会审批通过,患者或家属均签署知情同意书。
1.2 指标检测 对2组患者入院6、12、24、48 h分别抽取肘静脉血5 ml检测相关生化指标,包括SCr、CysC、血清NGAL(sNGAL)及留取清晨中段尿液行尿NGAL(uNGAL)检测。CysC采用免疫比浊法测定,SCr采用酶法测定,sNGAL及uNGAL均采用ELISA法,GFR采用计算法,根据Cockcroft-Gault方程:GFR=(140-年龄)×体质量/72×SCr×0.84(女性0.85)。以上相关操作均按试剂盒说明进行,各指标由本院引进的日本日立7600型全自动生化分析仪进行检测。
2 结果
2.1 一般资料 共收集肝硬化组患者236例,其中男143例,女93例,年龄35~75岁,平均(49.43±13.73)岁;对照组100例,其中男59例,女41例,年龄34~73岁,平均(48.65±14.98)岁。2组患者在性别、年龄、体质量等方面差异均无统计学意义(P值均>0.05),具有可比性。依据患者48 h内SCr上升水平将肝硬化组分为AKI组(78例)和非AKI组(158例),AKI组中1期28例,2期38例,3期12例。
2.2 入院48 h的SCr、GFR、CysC、sNGAL、uNGAL水平比较 结果显示,非AKI组及对照组患者的SCr、CysC、sNGAL、uNGAL水平均低于AKI组,而非AKI组GFR高于AKI组(P值均<0.05);对照组SCr、CysC、sNGAL、uNGAL水平均低于非AKI组,而GFR高于非AKI组(P值均<0.05)(表1)。
2.3 AKI组不同分期的患者入院48 h的SCr、GFR、CysC、sNGAL及uNAGL水平比较 结果显示,不同时期患者的SCr、GFR、CysC、sNGAL、uNGAL水平差异均具有统计学意义(P值均<0.05)(表2)。
2.4 肝硬化患者在不同时间点sNGAL、uNAGL、CysC、SCr、GFR水平变化 与入院时相比,入院6 h时sNGAL、uNGAL与CysC水平已开始升高,而SCr与GFR变化不明显,在48 h才开始变化(P值均<0.05)(表3)。
2.5 AKI组患者入院48 h sNGAL、uNGAL及CysC与SCr的Pearson相关性分析 结果显示,sNGAL、uNGAL及CysC均与SCr呈正相关(r=0.650,P=0.013;r=0.681,P=0.009;r=0.581,P=0.011)(图1~3)。
2.6 sNGAL、uNGAL及CysC诊断肝硬化继发AKI的ROC曲线分析 sNGAL的AUC为0.845±0.435,最佳阈值为542.68 μg/L,敏感度为0.824,特异度为0.794;uNGAL的AUC为0.836±0.326,最佳阈值为75.12 μg/L,敏感度为0.816,特异度为0.766;CysC的AUC为0.818±0.267,最佳阈值为1.48 mg/L,敏感度为0.808,特异度为0.732(图4)。
3 讨论
AKI是肝硬化常见并发症之一,常见为服用利尿剂、消化道出血、腹泻等致血容量不足以及肾毒性药物直接造成肾缺血灌注所致[10]。肝硬化患者一旦发生AKI,其预后较差,病死率较高,若早期诊断治疗,肾功能损伤可逆转,极大改善患者预后及生存质量[11]。故寻找早期能够诊断AKI的生物学标志物至关重要。

表1 3组间入院48 h的SCr、GFR、CysC、sNGAL、uNGAL比较分析
注:与AKI组比较,1)P<0.05;与非AKI组比较,2)P<0.05

表2 AKI组不同分期的患者入院48 h的SCr、GFR、CysC、pNAGL及uNAGL比较分析
注:与1期比较,1)P<0.05;与2期比较,2)P<0.05

表3 不同时间点sNGAL、uNAGL、CysC、SCr、GFR变化比较
注:与入院时比较,1)P<0.05;与入院6 h比较,2)P<0.05;与入院12 h比较,3)P<0.05;与入院24 h比较,4)P<0.05

图1 AKI组患者sNGAL与SCr的相关性
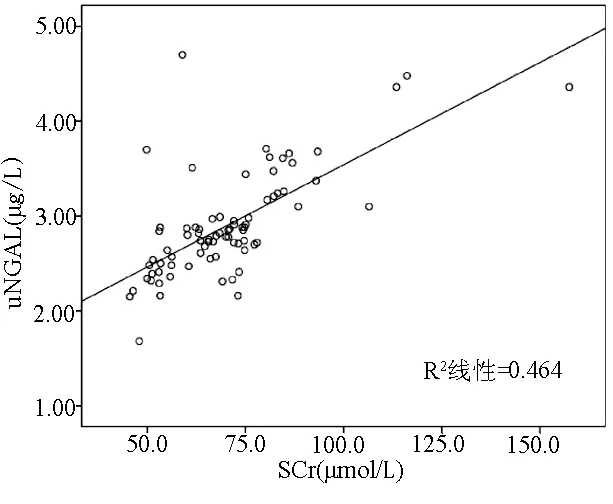
图2 AKI组患者uNGAL与SCr的相关性
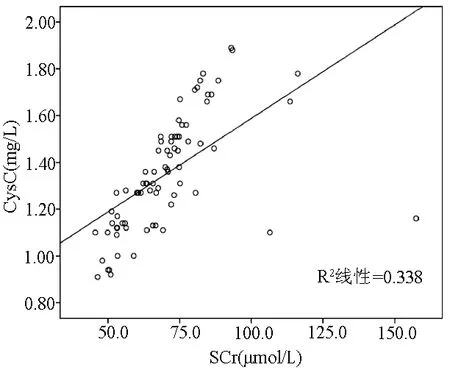
图3 AKI组患者CysC与SCr的相关性
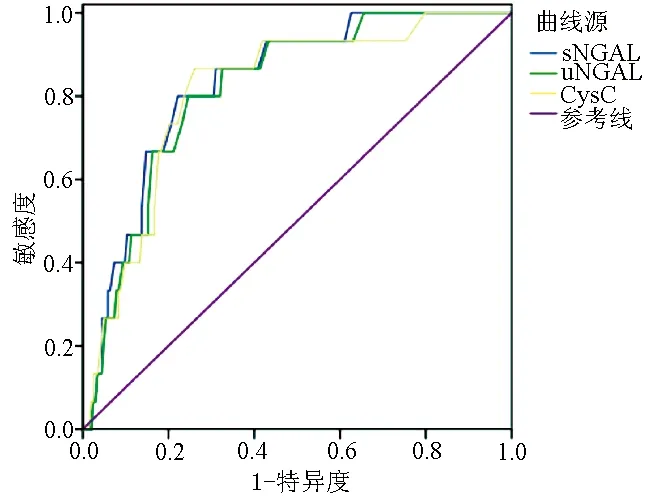
图4 sNGAL、uNGAL及CysC诊断肝硬化继发AKI的ROC曲线
目前SCr作为检测肾功能的指标不够准确,与患者性别、种族、健康营养状态等有关,另在反映肾功能方面其开始上升时间较为延迟,故不能特异性及敏感性的反映肾功能真实情况[1]。NGAL是由197个氨基酸残基组成的分泌性小分子蛋白物质[12]。生理状态下,在人类中性粒细胞、肾小管细胞及胃壁细胞等均可表达,机体中NGAL参与免疫、趋化、抑制氧化应激等作用[13]。刘华杰等[14]研究证实,肾小管上皮细胞可表达少量NGAL,当肾组织缺血缺氧性损伤时,血液及尿液中NGAL水平明显升高。目前NGAL已作为早期诊断肾小管损伤的特异性及敏感性检测指标,其开始上升时间较早,对于诊断AKI较SCr迅速有效,而肝硬化并发AKI以肾前性和肾性为主,故NGAL诊断肝硬化并发AKI具有较强的理论依据。CysC恒定表达于有核细胞中,可自由通过肾小球基底膜,在近曲小管被完全重吸收,肾小管自身不分泌CysC,一旦尿液中检测出CysC可提示AKI[15-16]。
本研究比较AKI组、非AKI组及对照组SCr、GFR、CysC、sNGAL、uNGAL水平发现,非AKI组及对照组患者SCr、CysC、sNGAL、uNGAL水平均低于AKI组,说明AKI组患者SCr、CysC、sNGAL、uNGAL水平均明显升高。对照组SCr、CysC、sNGAL、uNGAL水平均低于非AKI组,而GFR高于非AKI组,说明肝硬化患者肾功能指标较正常者轻度偏高,即肝硬化可能为肾损伤的危险因素之一。本研究通过对AKI组不同KDIGO标准分期的患者SCr、GFR、CysC、sNGAL及uNAGL比较发现,不同分期患者SCr、GFR、CysC、sNGAL、uNGAL水平差异均具有统计学意义,随着病情严重程度的增加,CysC、sNGAL、uNGAL亦不同程度升高,此与国内学者赵炜[17]研究结论相一致。本研究通过对肝硬化并发AKI患者入院6、12、24及48 h的NGAL、SCr、CysC及GFR水平比较发现,入院6 h时sNGAL、uNGAL与CysC水平开始升高,而此时SCr与GFR变化不明显,说明NGAL、CysC可以早期反映肾功能改变情况,而SCr、GFR入院48 h才明显改变(P值均<0.05),明显滞后于NGAL、CysC(入院6 h)。另外,本研究发现,sNGAL、uNGAL及CysC均与SCr呈正相关(r值分别为0.650、0.681、0.581,P值均<0.05)。由此说明,尚可以用sNGAL、uNGAL及CysC替代SCr用于早期反映肾功能真实情况。最后本研究通过利用sNGAL、uNGAL及CysC用于诊断肝硬化继发AKI的ROC曲线显示,sNGAL、uNGAL及CysC三者对于诊断AKI具有较高的敏感性及特异性,与葛斌等[18]报道相符。
综上所述,sNGAL、uNGAL及CysC较SCr及GFR更为准确反映早期肾功能不全,尤其用于诊断肝硬化并发AKI具有较高的特异性及敏感性,为AKI的早期发现及治疗提供了强有力的依据,有利于降低患者病死率及致残率,值得临床推广。
[1] BELCHER JM. Acute kidney injury in liver disease: role of biomarkers[J]. Adv Chronic Kidney Dis, 2015, 22(5): 368-375.
[2] FIRU SG, STREBA CT, FIRU D, et al. Neutrophil gelatinaseassociated lipocalin(NGAL)-a biomarker of renal dysfunction patients with liver cirrhosis: do we have enough proof[J]. J Med Life, 2015, 8(Suppl 1): 15-20.
[3] NADKARNI GN, SIMOES PK, PATEL A, et al. National trends of acute kidney injury requiring dialysis in decompensated cirrhosis hospitalizations in the United States[J]. Hepatol Int, 2016,10(3): 525-531.
[4] WAN ZH, WANG JJ, XIE GM, et al. Significance of serum cystatin C level for early diagnosis of acute kidney injury in patients with acute-on-chronic liver failure[J]. J Clin Hepatol, 2014, 30(7): 666-669. (in Chinese)
万志红, 王建军, 谢国明, 等. 血清胱抑素C对慢加急性肝衰竭患者肾损伤的早期诊断意义[J]. 临床肝胆病杂志, 2014, 30(7): 666-669.
[5] PATEL ML, SACHAN R, VERMA A, et al. Neutrophil gelatinase-associated lipocalin as a biomarker of disease progression in patients with chronic kidney disease[J]. Indian J Nephrol, 2016, 26(2): 125-130.
[6] QU AH, WANG YG, WANG LY, et al. The value of Cystatin C for assessing condition of acute kidney injury in patients with liver cirrhosis[J]. Acta Acod Med Qingdao Univ, 2016, 52(3): 325-328. (in Chinese)
曲爱华, 王义国, 汪丽云, 等. 胱抑素C对肝硬化急性肾损伤病情评估的价值[J]. 青岛大学医学院学报, 2016, 52(3): 325-328.
[7] ZHANG SE. Diagnostic criteria and treatment options for cirrhosis[J]. Mod J Integr Tradit Chin West Med, 2002, 11(10): 953-954. (in Chinese)
张书娥. 肝硬化的诊断标准和治疗方案[J]. 现代中西医结合杂志, 2002, 11(10): 953-954.
[8] JI LJ, QIAN ZP, WANG JF. Advances in early diagnosis of acute renal injury due to cirrhosis[J]. Chin Hepatol, 2016, 21(12): 1081-1084. (in Chinese)
纪留娟, 钱志平, 王介非. 肝硬化急性肾损伤早期诊断的研究进展[J]. 肝脏, 2016, 21(12): 1081-1084.
[9] ZANG H, WAN ZH, XIN SJ. Early clinical diagnosis of liver cirrhosis with acute kidney injury[J]. Chin J Infect Dis, 2015, 33(9): 566-568. (in Chinese)
臧红, 万志红, 辛绍杰. 肝硬化急性肾损伤的早期临床诊断[J]. 中华传染病杂志, 2015, 33(9): 566-568.
[10] LUO JH, WU N. Value of serum kidney injury molecule-1 level in early predicting renal dysfunction secondary to liver cirrhosis[J]. Lab Med Clin, 2015, 12(2): 188-190. (in Chinese)
罗俊华, 吴娜. 肾损伤分子-1对肝硬化继发肾功能损害早期预测的价值[J]. 检验医学与临床, 2015, 12(2): 188-190.
[11] PU CW, WANG BY, QIAO L, et al. Recent progress in research of biomarkers of acute kidney injury in liver cirrhosis[J]. Chin J Hepatol, 2013, 21(10): 796-798. (in Chinese)
蒲春文, 王炳元, 乔梁, 等. 肝硬化并发急性肾损伤标志物的研究进展[J]. 中华肝脏病杂志, 2013, 21(10): 796-798.
[12] NAYAK NM, MADHUMITHA S, ANNIGERI RA, et al. Clinical utility of urine neutrophil gelatinase-associated lipocalin measured at admission to predict outcomes in heterogeneous population of critically ill patients[J]. Indian J Nephrol, 2016, 26(2): 119-124.
[13] HONORE PM, SPAPEN HD. Neutrophil gelatinase-associated lipocalin elimination by renal replacement therapy: minding the membrane![J]. Crit Care, 2016, 20(1): 87.
[14] LIU HJ, WANG P, SHEN YL, et al. Combination of urine neutrophil gelatinase lipocalin associated lipocalin, kidney injury molecular-1 and interleukin-18 in the diagnosis of acute kidney injury in children after cardiopulmonary bypass[J]. J Clin Pediatr, 2014, 32(6): 517-523. (in Chinese)
刘华杰, 王平, 沈云琳, 等. 中性粒细胞明胶酶相关脂质运载蛋白、肾损伤分子1和白介素18在诊断心肺分流术后急性肾损伤中的意义[J]. 临床儿科杂志, 2014, 32(6): 517-523.
[15] DU W, XING JY, SUN YB, et al. Effects of timing of renal replacement therapy on outcomes in patients with acute kidney injury: a meta analysis[J]. Acta Acad Med Qingdao Univ, 2015, 51(3): 341-344. (in Chinese)
杜伟, 邢金燕, 孙运波, 等. RRT时机对急性肾损伤病人预后影响的Meta分析[J]. 青岛大学医学院学报, 2015, 51(3): 341-344.
[16] PENG HY, ZONG XX, PEI L. Diagnostic value of combined detection of serum cystatin C and microalbuminuria in diabetic patients with early renal injury[J]. Chin J Med Offic, 2015, 43(6): 648-649.(in Chinese)
彭海英, 宗先旭, 裴莉. 血清胱抑素 C和尿微量白蛋白联合检测在糖尿病患者早期发现肾损伤中的诊断价值[J]. 临床军医杂志, 2015, 43(6): 648-649.
[17] ZHAO W. Clinical significance of plasma and urine neutrophil gelatinase-associated lipocalin levels in diagnosis of acute kindney injury in patients with cirrhosis[J]. J Clin Hepatol, 2015, 31(11): 1874-1877. (in Chinese)
赵炜. 血、尿中性粒细胞明胶酶相关脂质运载蛋白对肝硬化急性肾损伤的诊断价值[J]. 临床肝胆病杂志, 2015, 31(11): 1874-1877.
[18] GE B, LIU Y, FENG JF, et al. Research progress of NGAL in the diagnosis of acute renal injury in patients with liver cirrhosis[J]. Int J Lab Med, 2017, 38(4): 508-510. (in Chinese)
葛斌, 刘艳, 俸家富, 等. NGAL在诊断肝硬化患者急性肾功能损伤中的研究进展[J]. 国际检验医学杂志, 2017, 38(4): 508-510.
引证本文:XU CH, JIANG KR. Value of serum and urinary neutrophil gelatinase-associated lipocalin and cystatin C in diagnosis of liver cirrhosis complicated by acute kidney injury[J]. J Clin Hepatol, 2017, 33(11): 2136-2140. (in Chinese)
许长红, 江坤仁. 血、尿中性粒细胞明胶酶相关脂质运载蛋白与胱抑素C对肝硬化并发急性肾损伤的诊断价值[J]. 临床肝胆病杂志, 2017, 33(11): 2136-2140.
(本文编辑:朱 晶)
Valueofserumandurinaryneutrophilgelatinase-associatedlipocalinandcystatinCindiagnosisoflivercirrhosiscomplicatedbyacutekidneyinjury
XUChanghong,JIANGKunren.
(DepartmentofInternalMedicine,TheRedCrossHospitalofHannanDistrict,Wuhan430090,China)
ObjectiveTo investigate the value of serum neutrophil gelatinase-associated lipocalin (sNGAL), urinary neutrophil gelatinase-associated lipocalin (uNGAL), and serum cystatin C (CysC) in the early diagnosis of acute kidney injury (AKI) in patients with liver cirrhosis.MethodsA total of 236 patients with liver cirrhosis and normal renal function who visited The Red Cross hospital of Hannan District from January 2015 to March 2017 were enrolled, and according to the presence or absence of AKI within 48 hours after admission, these patients were divided into AKI group with 78 patients and non-AKI group with 158 patients. Another 100 healthy subjects who underwent physical examination were enrolled as control group. ELISA was used to measure sNGAL, uNGAL, and serum CysC, and serum creatinine (SCr) and glomerular filtration rate (GFR) were compared between groups. A one-way analysis of variance was used for comparison of continuous data between multiple groups, and the SNK-qtest was used for further comparison between two groups. A Pearson correlation analysis was also performed, and the receiver operating characteristic (ROC) curve was used to evaluate the diagnostic value of these indices.ResultsAt 48 hours after admission, there were significant differences in sNGAL, uNGAL, and CysC between the AKI group and the non-AKI group/control group (allP<0.05). The patients in the AKI group were stratified by AKI stage based on the criteria for kidney injury, and the patients with a higher stage had significantly higher levels of sNGAL and uNGAL than those with a lower stage (bothP<0.05). The levels of sNGAL, uNGAL, and CysC started to increase at 6 hours after admission, while Scr and GFR started to change at 48 hours after admission, i.e., sNGAL and uNGAL increased significantly earlier than Scr and GFR (P<0.05). In the AKI group, sNGAL, uNGAL, and CysC were positively correlated with SCr (r=0.650, 0.681, and 0.581, allP<0.05). According to the ROC curve analysis, sNGAL had an area under the ROC curve (AUC) of 0.845±0.435, an optimal cut-off value of 542.68 μg/L, a sensitivity of 0.824, and a specificity of 0.794, uNGAL had an AUC of 0.836±0.326, an optimal cut-off value of 75.12 μg/L, a sensitivity of 0.816, and a specificity of 0.766, and CysC had an AUC of 0.818±0.267, an optimal cut-off value of 1.48 mg/L, a sensitivity of 0.808, and a specificity of 0.732.ConclusionNGAL and CysC can be used as indices for the early diagnosis of AKI and have great significance in evaluating renal injury and developing treatment measures for patients with liver cirrhosis.
liver cirrhosis; renal insufficiency, acute; neutrophil gelatinase-associated lipocalin; cystatin C; diagnosis
R575.2; R692
A
1001-5256(2017)11-2136-05
10.3969/j.issn.1001-5256.2017.11.017
2017-05-10;
2017-06-03。
许长红(1967-),男,主治医师,主要从事肝硬化方面的研究。