Tailored pancreatic reconstruction after pancreaticoduodenectomy: a single-center experience of 892 cases
2017-10-09AymanElNakeebAhmadSultanEhabAtefAliSalemMostaffaAbuZeidAhmedAbuElEneenGamalElEbidyandMohamedAbdelWahab
Ayman El Nakeeb, Ahmad M Sultan, Ehab Atef, Ali Salem, Mostaffa Abu Zeid,Ahmed Abu El Eneen, Gamal El Ebidy and Mohamed Abdel Wahab
Mansoura, Egypt
Tailored pancreatic reconstruction after pancreaticoduodenectomy: a single-center experience of 892 cases
Ayman El Nakeeb, Ahmad M Sultan, Ehab Atef, Ali Salem, Mostaffa Abu Zeid,Ahmed Abu El Eneen, Gamal El Ebidy and Mohamed Abdel Wahab
Mansoura, Egypt
BACKGROUND: Pancreatic reconstruction following pancreaticoduodenectomy (PD) is still debatable even for pancreatic surgeons. Ideally, pancreatic reconstruction aer PD should reduce the risk of postoperative pancreatic fistula (POPF)and its severity if developed with preservation of both exocrine and endocrine pancreatic functions. It must be tailored to control the morbidity linked to the type of reconstruction.is study was to show the best type of pancreatic reconstruction according to the characters of pancreatic stump.
METHODS: We studied all patients who underwent PD in our center from January 1993 to December 2015. Patients were categorized into three groups depending on the presence of risk factors of postoperative complications: low-risk group (absent risk factor), moderate-risk group (presence of one risk factor) and high-risk group (presence of two or more risk factors).
RESULTS: A total of 892 patients underwent PD for resection of periampullary tumor. BMI >25 kg/m2, cirrhotic liver, sopancreas, pancreatic duct diameter <3 mm, and pancreatic duct location from posterior edge <3 mm are risk variables for development of postoperative complications. POPF developed in 128 (14.3%) patients. Delayed gastric emptying occurred in 164 (18.4%) patients, biliary leakage developed in 65 (7.3%) and pancreatitis presented in 20 (2.2%). POPF in low-, moderate- and high-risk groups were 26 (8.3%), 65(15.7%) and 37 (22.7%) patients, respectively. Postoperative morbidity and mortality were significantly lower with pan-creaticogastrostomy (PG) in high-risk group, while pancreaticojejunostomy (PJ) decreases incidence of postoperative steatorrhea in all groups.
CONCLUSIONS: Selection of proper pancreatic reconstruction according to the risk factors of patients may reduce POPF and postoperative complications and mortality. PG is superior to PJ as regards short-term outcomes in high-risk group but PJ provides better pancreatic function in all groups and therefore, PJ is superior in low- and moderate-risk groups.
(Hepatobiliary Pancreat Dis Int 2017;16:528-536)
periampullary tumor;
pancreaticogastrostomy;
pancreaticojejunostomy;
pancreaticoduodenectomy;
postoperative pancreatic fistula
Introduction
Pancreaticoduodenectomy (PD) is the main line of treatment of periampullary tumors. PD is a complex operation which involves extensive dissection,resection and multiple reconstructions.[1-5]e mortality rate has reduced to 3%-5% in many published series while the rate of postoperative complications remains high, from 40% to 50%.[3-7]In most of patients, morbidity and mortality aer PD are linked to features of pancreatic remnant and type of pancreatic reconstruction.[3-6]Postoperative pancreatic fistula (POPF) aer PD remains a problem even at high-volume centers.[4-8]e rate of POPffollowing PD is ranging from 5% to 35%. POPF and its disastrous sequelae impact surgical outcome, hospital stay and cost.[5-9]
Ideally, the pancreatic reconstruction aer PD should reduce the risk of POPF and its severity if occurred and also, preserve exocrine and endocrine pancreatic functions.[8-12]Several technical modulations of the pancreaticreconstructions have been performed to prevent postoperative morbidities including: surgical techniques (isolated Roux loop pancreaticojejunostomy [PJ], binding PJ, reconstruction by pancreaticogastrostomy [PG], and uses of pancreatic duct stent), somatostatin administration, and use of adhesive sealants.[13-17]e most common types of pancreatic reconstruction are PJ and PG.[1-4]Many meta-analyses of both types of reconstruction showed no superiority of any technique as regards short-term outcomes. Long-term outcomes, including structural and functional outcomes of the remaining pancreas, have yet to be fully studied.[17-21]
Methods
Study design
We studied all patients who underwent PD for periampullary tumor in Gastroenterology Surgical Center, Mansoura University, Egypt, from January 1993 to December 2015. Patient data were recorded in a prospectively maintained database for all patients undergoing PD since 2000 and before 2000, the data were recorded from the archive files of patients. Informed consent was signed from all patients aer explanation of the surgical procedure.e current study was approved by institutional review board of Mansoura University.
Preoperative assessment
Preoperative assessment for diagnosis and staging included: clinical assessment, laboratory investigations, and radiological investigations. Preoperative biliary drainage was carried out by endoscopic retrograde cholangiopancreatography when biliary obstruction was associated with cholangitis or liver dysfunction as described in our previous publications.[4,23]
Surgical procedures
Operative details including different types of pancreatic reconstruction either simple PJ, PG, or isolated Roux loop PJ and different techniques either duct to mucosa or invaginated type.[23,24]e types of reconstruction depend on surgeon choice or on randomization in the randomized study.
Simple PJ
PJ was performed in two layers aer creation of 2-3 cm jejunostomy (in invagination PJ) or a small jejunostomy equal to pancreatic duct diameter (in duct to mucosa PJ)without pancreatic stenting. Biliary reconstruction was performed by end-to-side hepaticojejunostomy (HJ) (retrocolic) in the same jejunal loop caudal to the PJ. Gastric reconstruction was performed by an antecolic end-toside gastrojejunostomy (GJ) 30 cm distal to the HJ.[23,24]
PG
Isolated Roux loop PJ
A separate Roux loop was created for the end-to-side HJ and the end-to-side antecolic GJ in one loop.e PJ loop was anastomosed to the main loop.is technique was done in our center from January 2011 to May 2013.[23]
Postoperative management
All patients were transferred to the intensive care unit postoperatively. Antibiotics and analgesics were given to all patients. Sandostatin was given to most of patients postoperatively. Abdominal drains were monitored daily.Oral fluid was started once bowel sounds restarted and regular diet was provided later on.
Abdominal ultrasound was performed postoperatively. Serum amylase and liver function (albumin, alanine aminotransferase, bilirubin) were tested in postoperative days 1 and 5. Ultrasound-guided tubal drainage was done for abdominal collections.
Follow-up was scheduled at day 7, 90 and 180 postoperatively, and then yearly.
Definitions
POPF was defined by International Study Group of Pancreatic Fistula (ISGPF) as any measurable volume offluid on or aer postoperative day 3 with amylase content greater than three times the normal upper limit of serum amylase level, and classified into three grades A, B, C.[4,25,26]We defined the patients who had been operated prior to the ISGPF definitions based on the recorded postoperative data and course.
Delayed gastric emptying was defined as persisted need of nasogastric tube for 8 days, the failure to tolerate a solid diet by postoperative day 14, or reinsertion of a nasogastric tube.[7,25,26]
Postpancreatectomy hemorrhage was graded as A,B or C according to the International Study Group of Pancreatic Surgery (ISPGS) consensus definition. Postpancreatectomy hemorrhage was defined as severe in the case of a large volume blood loss (drop in hemoglobin level by ≥3 g/dL), requiring transfusion of more than 3 U of packed red blood cells or in cases of interventional treatment.[25,26]
Pancreatic endocrine function was evaluated by follow up whether the patients had diabetes mellitus.Pancreatic exocrine function was evaluated clinically,the follow up of patients included the development of steatorrhea (more than three stools per day, fecal output of >200 g/day for at least 3 days, pale or yellow stools,and stools with a pasty or greasy appearance).[23]e evidences for the diagnosis of pancreatic exocrine insufficiency is weak because fecal elastase levels are unreliable post-surgery and the center does not have C13 breath testing.e diagnosis of pancreatic exocrine insufficiency depends on clinical development of steatorrhea or the need of exogenous pancreatic enzymes.
Assessments
Statistical analysis
Results
Of 892 patients underwent PD, 516 were pancreatic head mass, 288 were ampullary tumor, 53 were duodenal tumor and 35 were cholangiocarcinoma (Table 1).
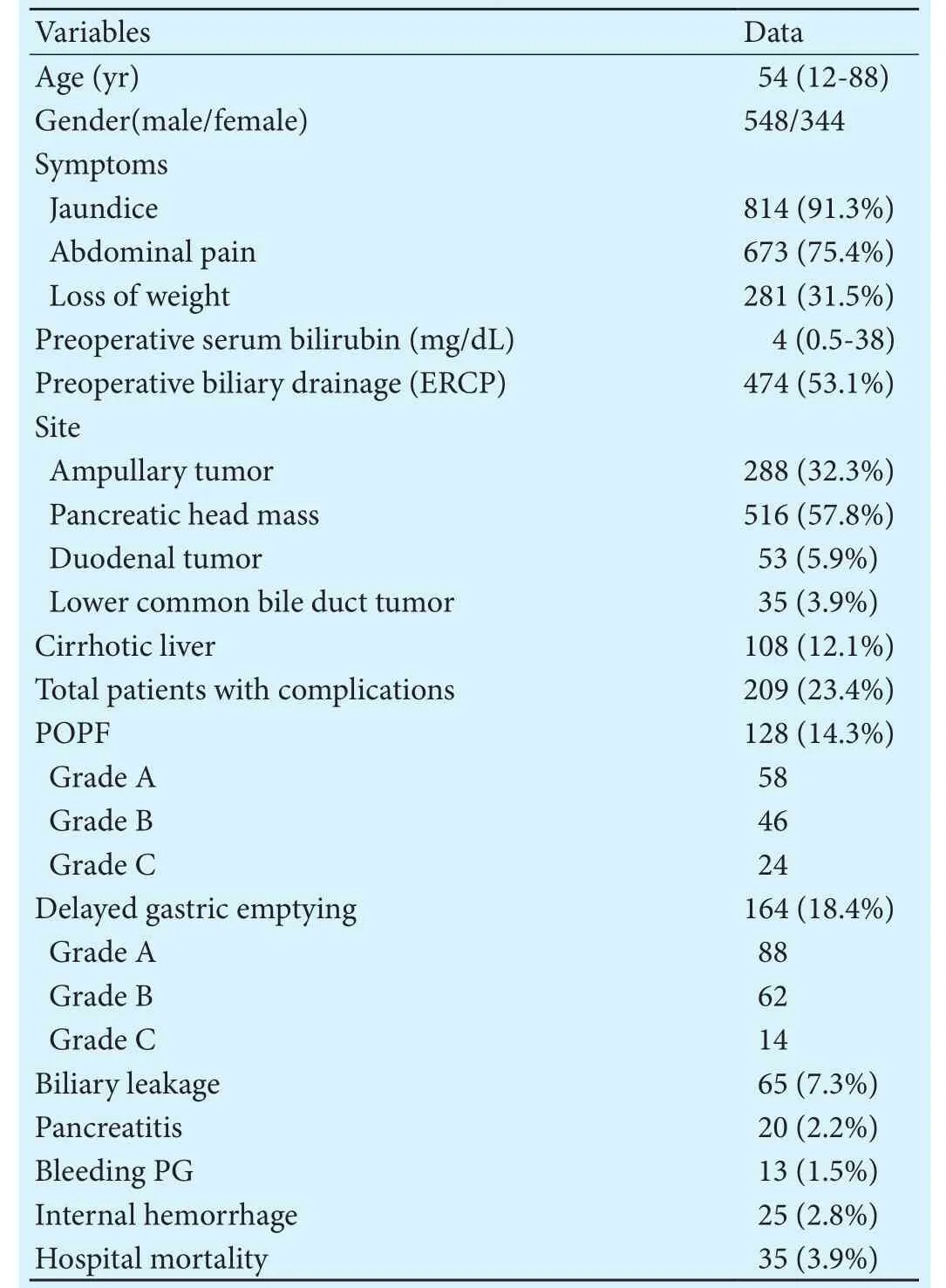
Table 1.Demographic data

Table 2.Univariate and multivariate analysis of risk factors of development of POPF
Low-risk patients
Overall complications were encountered in 48 (15.3%)patients. POPF developed in 26 (8.3%) patients. Delayed gastric emptying occurred in 29 (9.2%) patients (Table 3).No significant difference among the three types of pancreatic reconstruction as regards postoperative complications, hospital mortality, drain removal, starting oral feeding and the median hospital stay. However, the severity of POPF was significantly observed more in PG and simple PJ than in isolated Roux loop PJ. In patients with PG, 95/238 (39.9%) patients presented with postoperative steatorrhea aer one year, versus 10/57 (17.5%)patients with simple PJ, and 2/14 (14.3%) patient with isolated Roux loop PJ (P=0.002).ese patients needpancreatic enzymes supplement.ere was no significant difference as regards the rate of diabetes mellitus among the three types of pancreatic reconstruction (Table 3).
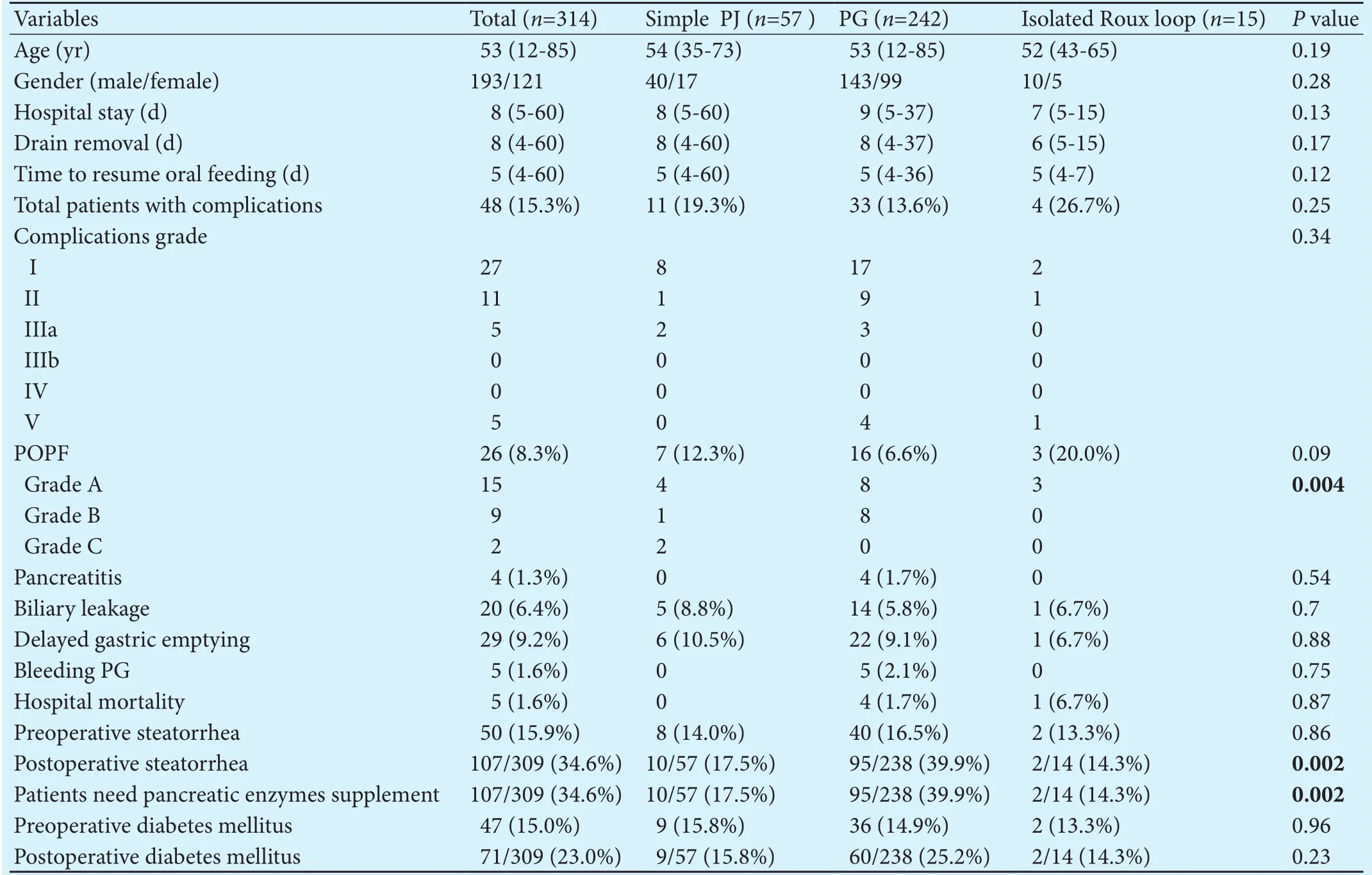
Table 3.Surgical outcomes for low-risk patients
Moderate-risk patients
Overall complications were encountered in 103 (24.8%)patients. POPF developed in 65 (15.7%) patients. Delayed gastric emptying occurred in 93 (22.4%) patients(Table 4). No significant difference among the three types of pancreatic reconstruction as regards postoperative complications, hospital mortality, drain removal, starting oral feeding and the median hospital stay. In patients with PG, 123/327 (37.6%) patients presented with postoperative steatorrhea aer one year, versus 12/47 (25.5%)patient with simple PJ, and 3/26 (11.5%) patient with isolated Roux loop PJ (P=0.006).ese patients need pancreatic enzymes supplement.ere was no significant difference as regards the rate of diabetes mellitus among the three types of pancreatic reconstruction (Table 4).
High-risk patients
Overall complications were encountered in 58 (35.6%)patients. POPF developed in 37 (22.7%) patients. Delayed gastric emptying occurred in 42 (25.8%) patients.e overall complications were significantly less observed in patients with PG (P=0.0001, Table 5). POPF developed in 13 (34.2%) patients with simple PJ, 21 (17.6%) with PG,and 3 (50.0%) patients with isolated Roux loop PJ. Delayed gastric emptying presented more in patients with simple PJ and isolated Roux loop PJ than in PG (Table 5).e hospital mortality was 15 (9.2%) patients in this group, 7 (18.4%) with simple PJ versus 6 (5.0%) with PG and 2 (33.3%) with isolated Roux loop PJ (P=0.002).e causes of death were systemic inflammatory response syndrome secondary to POPF in 11 patients, one due to liver failure, one due to cardiac arrest, one due to pulmonary embolism, and one due to respiratory failure secondary to severe lung infection.e median hospital stay and time of drain removal were significantly shorter in patients with PG than those with other pancreatic reconstruction (P<0.05). In patients with PG, 42/113 (37.2%)presented with postoperative steatorrhea aer one year,versus 3/31 (9.7%) with simple PJ, and 0 with isolated Roux loop PJ (P=0.03).ese patients need pancreatic enzymes supplement.ere was no significant difference as regards the rate of diabetes mellitus among the three types of pancreatic reconstruction (Table 5).
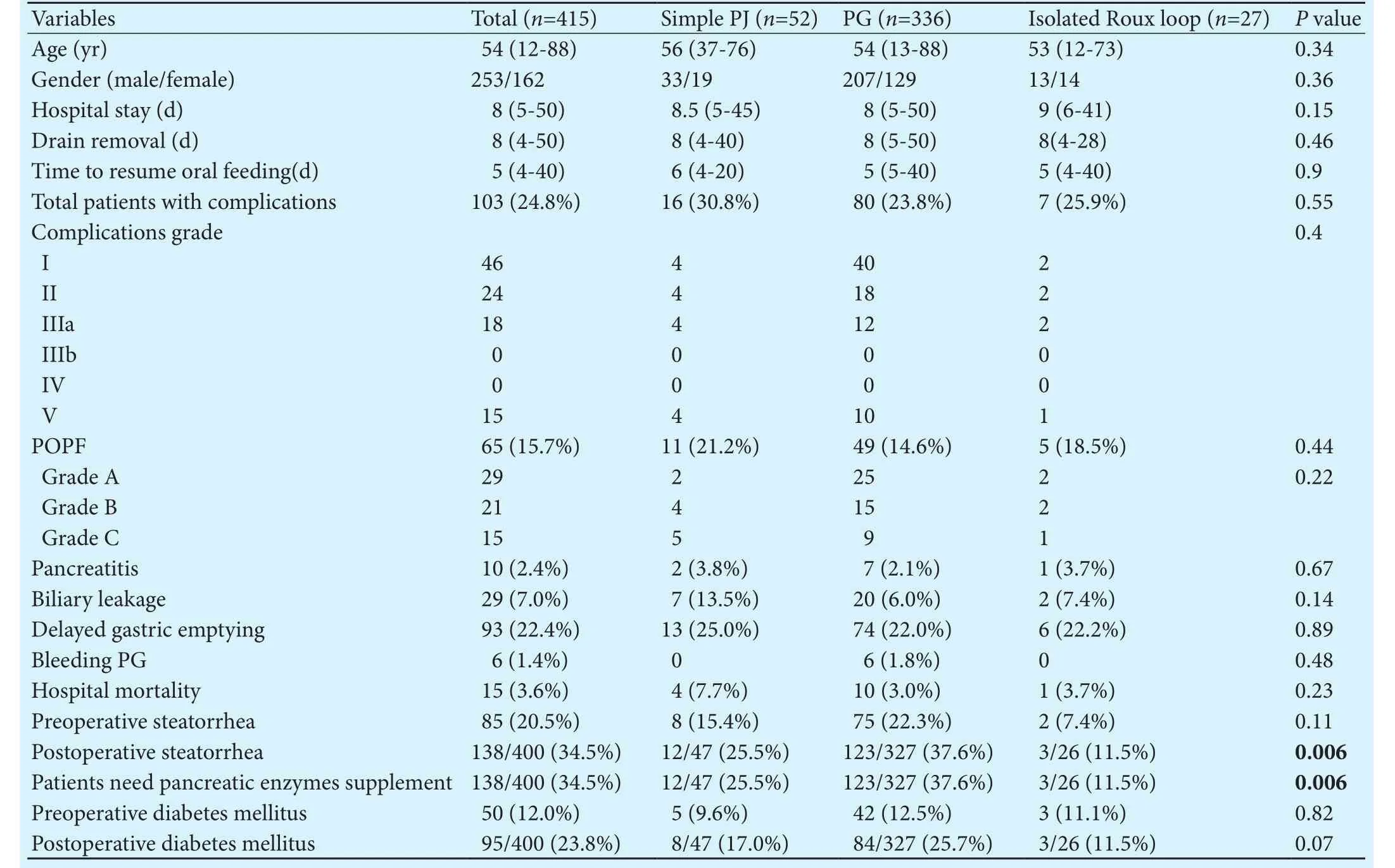
Table 4.Surgical outcomes for moderate-risk patients
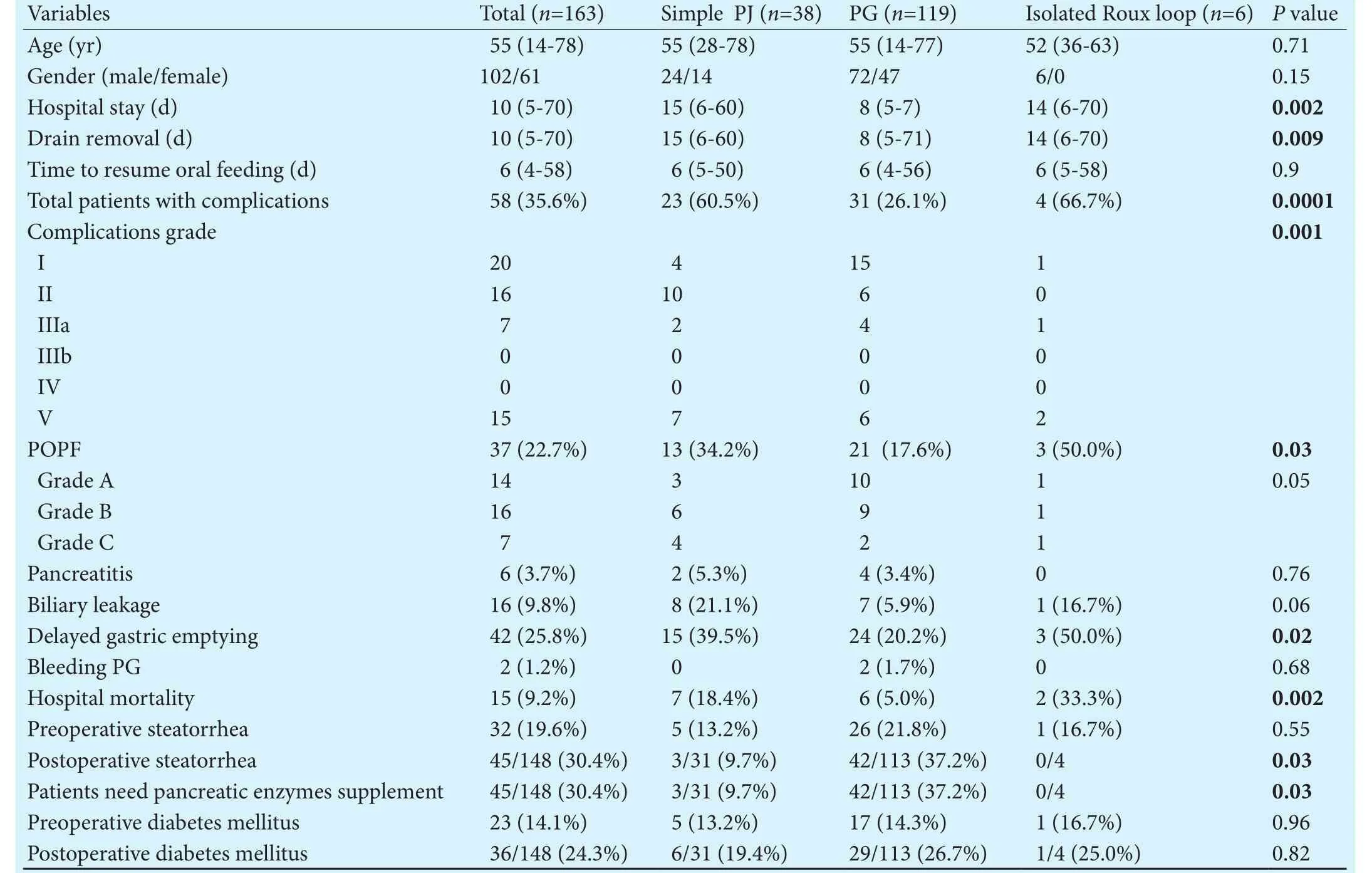
Table 5. Surgical outcomes for high-risk patients
Discussion
POPffollowing PD remains a problem even at specialized pancreatic centers.[4-8]Ideally, the pancreatic reconstruction should reduce the development of POPF and decrease its severity if it developed and should preserve exocrine and endocrine pancreatic functions.[8-12,23]However, the pancreatic reconstruction remains a personal choice depending on the experience and belief of the surgeons. Every pancreatic surgeon has a preferable method of reconstruction aer PD. High-volume hospital may have better outcomes due to expert skills attributed to frequent repetition.[22]e three most common techniques including are duct to mucosa PJ, invaginating PJ,and PG. Randomized prospective studies providing evidence for best way to perform a pancreatic reconstruction are few.[8-12]
Some meta-analyses comparing PG and PJ failed to conclude the optimal pancreatic reconstruction following PD as regards postoperative morbidity and mortality.[17-21]Other meta-analyses demonstrated that PG is associated with significantly fewer POPF than PJ following PD.[29-35]e PG anastomosis is easy to do, stomach is thick wall holds sutures well, has excellent blood supply, close to pancreatic stump, its acidity inhibit the proteolytic enzymes of pancreatic juice, lack of enterokinase in gastric juice and continuous suction by nasogastric tube facilitate sound anastomosis. PG can be assessed by endoscopy postoperatively and allow to remove internal pancreatic stent if it was inserted.[18-21,29-34]
One of the problems in PJ may be increasing possibility of leakage with its subsequent morbidity, pancreatic trypsinogin entering the small intestine becomes activated by enterokinase and this proteolytic enzyme act on the anastomotic site. Obstruction or distension of the intestine can lead to positive backpressure on the anastomosis, and edema of jejunal mucosa may increase the incidence of leakage. PJ is located near the major blood vessels which are dissected during PD. If POPF occurs,the major vessels are liable to be eroded by activated proteolytic pancreatic enzymes.[30-35]
In simple PJ, if POPF developed it is usually complex and severe due to leakage of biliary and pancreatic secretion and nearby major blood vessels may be affected.[30-35]Isolated Roux loop PJ reduces the incidence and severityof POPF as a result of separation of bile and pancreatic juices so reducing the activation of pancreatic enzymes by biliary secretion. It also, decreases the incidence of postoperative steatorrhea. A possible disadvantage of isolated Roux loop PJ is the additional enteroenterostomy which increases the operative time.[23,30-35]
As regards long-term follow-up, PJ is a favorable pancreatic reconstruction aer PD because it maintains exocrine and endocrine pancreatic functions rather than PG reconstruction.[23,36-42]PG may lead to more structural and functional disruption because the gastric juice suppresses pancreatic enzymes causing pancreatic insufficiency, and impairment of pancreatic juice flow due to anastomotic stricture or swelling of the gastric mucosa.[36-38]
Pancreatic reconstruction is difficult in certain situations as small pancreatic duct, pancreatic duct close to posterior border and a sofragile pancreas even in experienced hands.[3-8]Small pancreatic duct makes duct to mucosa PJ complex and easily obstructed due to edema of jejunal mucosa and incorrect suture position.[20-24]Reconstruction of sopancreatic stump is strongly associated with POPF. Sopancreas is more liable to injury either directly or due to ischemia by stitches during reconstruction. Also, sopancreas is more healthy than hard one and so it secrets more pancreatic juice rich in proteolytic enzymes than hard one.[37,42-47]
In our center, in last years, many randomized studies were performed to decrease the incidence of POPF and its severity and to maintain postoperative endocrine and exocrine pancreatic function.[23,24]Duct to mucosa pancreatic reconstruction is considered to be a procedure of choice for hard pancreas with large pancreatic duct.[24]Some studies found that the duct to mucosa pancreatic reconstruction was associated with a lower incidence of POPF in patients with hard pancreas or dilated pancreatic duct, whereas the invagination pancreatic reconstruction was safer in patients with sopancreas or small pancreatic duct.[20,21,24]
Many studies[47-49]tried to develop fistula risk scoring system aer PD.ey used many factors including pancreatic duct diameter, texture of pancreas, BMI >25 kg/m2and absence of pancreatic fibrosis. A score depends on the number of risk variables divided the patients into four categories carrying a risk of POPF that ranged from 7% (no risk factor) to 78% (three risk factors).[48]Presence of these predictive scores based on presence of risk factors may allow surgeons to tailor preventive methods to decrease the incidence of POPF and its severity aer PD which include type of pancreatic reconstruction, use of duct-invagination pancreatic reconstruction, use of pancreatic stent, use of surgical loupe in small pancreatic duct, use offibrin glue, use of somatostatine.[24,43]
Using the present categorization of risk factors may enable surgeons to select the type of pancreatic reconstruction and tailor it for each patient according to the presence of risk factors as PG can be performed more safer than PJ in high-risk patients, it also may allow early removal of drain in low-risk patients, and junior surgeons can perform PD and pancreatic reconstruction in low-risk patients. Invagination pancreatic reconstruction is better than duct to mucosa in high-risk patients.e choice of pancreatic reconstruction should not only be based on individual experience but also on anatomical and structural factors of pancreatic stump.[47-51]Pancreatic surgeons should perform all main types of pancreatic reconstruction perfectly and the choice of the type of reconstruction according to pancreatic stump consistency,pancreatic duct diameter, its relation to posterior border of pancreatic stump and liver status.
In conclusion, risk factors responsible for development of morbidities aer PD are BMI >25 kg/m2, cirrhotic liver, sopancreas, pancreatic duct diameter <3 mm,and pancreatic duct location from posterior edge <3 mm.PG is superior to PJ as regards short-term outcomes but PJ provides better long-term outcomes including pancreatic function. Selection of proper pancreatic reconstruction according to the risk of patients may reduce POPF and postoperative complications and mortality. PG is superior to PJ as regards short-term outcomes in high-risk group but PJ provides better pancreatic function in all groups. PJ is superior in low- and moderate-risk groups.
Contributors:ENA proposed the study and wrote the first dra.ENA and SA collected and analyzed the data. All authors contributed to the design and interpretation of the study and to further dras. ENA is the guarantor.
Funding:None.
Ethical approval:is study was approved by Institutional Review Board of Mansoura University (Egypt).
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Figueras J, Sabater L, Planellas P, Muñoz-Forner E, Lopez-Ben S, Falgueras L, et al. Randomized clinical trial of pancreaticogastrostomy versus pancreaticojejunostomy on the rate and severity of pancreatic fistula aer pancreaticoduodenectomy.Br J Surg 2013;100:1597-1605.
2 Tani M, Kawai M, Hirono S, Okada KI, Miyazawa M, Shimizu A, et al. Randomized clinical trial of isolated Roux-en-Y versus conventional reconstruction aer pancreaticoduodenectomy.Br J Surg 2014;101:1084-1091.
3 Topal B, Fieuws S, Aerts R, Weerts J, Feryn T, Roeyen G, et al. Pancreaticojejunostomy versus pancreaticogastrostomy reconstruction aer pancreaticoduodenectomy for pancreatic or periampullary tumours: a multicentre randomised trial. Lancet Oncol 2013;14:655-662.
4 El Nakeeb A, Salah T, Sultan A, El Hemaly M, Askr W, Ezzat H, et al. Pancreatic anastomotic leakage aer pancreaticoduodenectomy. Risk factors, clinical predictors, and management(single center experience). World J Surg 2013;37:1405-1418.
5 Reid-Lombardo KM, Farnell MB, Crippa S, Barnett M,Maupin G, Bassi C, et al. Pancreatic anastomotic leakage aer pancreaticoduodenectomy in 1507 patients: a report from the Pancreatic Anastomotic Leak Study Group. J Gastrointest Surg 2007;11:1451-1459.
6 Kawai M, Kondo S, Yamaue H, Wada K, Sano K, Motoi F, et al.Predictive risk factors for clinically relevant pancreatic fistula analyzed in 1239 patients with pancreaticoduodenectomy:multicenter data collection as a project study of pancreatic surgery by the Japanese Society of Hepato-Biliary-Pancreatic Surgery. J Hepatobiliary Pancreat Sci 2011;18:601-608.
7 El Nakeeb A, Askr W, Mahdy Y, Elgawalby A, El Sorogy M,Abu Zeied M, et al. Delayed gastric emptying aer pancreaticoduodenectomy. Risk factors, predictors of severity and outcome. A single center experience of 588 cases. J Gastrointest Surg 2015;19:1093-1100.
8 Yeo CJ, Cameron JL, Maher MM, Sauter PK, Zahurak ML,Talamini MA, et al. A prospective randomized trial of pancreaticogastrostomy versus pancreaticojejunostomy aer pancreaticoduodenectomy. Ann Surg 1995;222:580-592.
9 Bassi C, Falconi M, Molinari E, Salvia R, Butturini G, Sartori N, et al. Reconstruction by pancreaticojejunostomy versus pancreaticogastrostomy following pancreatectomy: results of a comparative study. Ann Surg 2005;242:767-773.
10 Fernández-Cruz L, Cosa R, Blanco L, López-Boado MA, Astudillo E. Pancreatogastrostomy with gastric partition aer pylorus-preserving pancreatoduodenectomy versus conventional pancreatojejunostomy: a prospective randomized study. Ann Surg 2008;248:930-938.
11 El Nakeeb A, Atef E, El Hanafy E, Salem A, Askar W, Ezzat H,et al. Outcomes of pancreaticoduodenectomy in elderly patients. Hepatobiliary Pancreat Dis Int 2016;15:419-427.
12 Tajima Y, Kuroki T, Tsuneoka N, Adachi T, Kosaka T, Okamoto T, et al. Anatomy-specific pancreatic stump management to reduce the risk of pancreatic fistula aer pancreatic head resection. World J Surg 2009;33:2166-2176.
13 Que W, Fang H, Yan B, Li J, Guo W, Zhai W, et al. Pancreaticogastrostomy versus pancreaticojejunostomy aer pancreaticoduodenectomy: a meta-analysis of randomized controlled trials. Am J Surg 2015;209:1074-1082.
14 Hashimoto D, Chikamoto A, Ohmuraya M, Hirota M, Baba H. Pancreaticodigestive anastomosis and the postoperative management strategies to prevent postoperative pancreatic fistula formation aer pancreaticoduodenectomy. Surg Today 2014;44:1207-1213.
15 Fernández-Cruz L, Belli A, Acosta M, Chavarria EJ, Adelsdorfer W, López-Boado MA, et al. Which is the best technique for pancreaticoenteric reconstruction aer pancreaticoduodenectomy? A critical analysis. Surg Today 2011;41:761-766.
16 Klaiber U, Probst P, Knebel P, Contin P, Diener MK, Büchler MW, et al. Meta-analysis of complication rates for single-loop versus dual-loop (Roux-en-Y) with isolated pancreaticojejunostomy reconstruction aer pancreaticoduodenectomy. Br J Surg 2015;102:331-340.
17 He T, Zhao Y, Chen Q, Wang X, Lin H, Han W. Pancreaticojejunostomy versus pancreaticogastrostomy aer pancreaticoduodenectomy: a systematic review and meta-analysis. Dig Surg 2013;30:56-69.
18 Zhang X, Ma L, Gao X, Bao H, Liu P, Aziz A, et al. Pancreaticogastrostomy versus pancreaticojejunostomy reconstruction aer pancreaticoduodenectomy: a meta-analysis of randomized controlled trials. Surg Today 2015;45:585-594.
19 Clerveus M, Morandeira-Rivas A, Picazo-Yeste J, Moreno-Sanz C. Pancreaticogastrostomy versus pancreaticojejunostomy aer pancreaticoduodenectomy: a systematic review and meta-analysis of randomized controlled trials. J Gastrointest Surg 2014;18:1693-1704.
20 Lei P, Fang J, Huang Y, Zheng Z, Wei B, Wei H. Pancreaticogastrostomy or pancreaticojejunostomy? Methods of digestive continuity reconstruction aer pancreaticodudenectomy:a meta-analysis of randomized controlled trials. Int J Surg 2014;12:1444-1449.
21 Hua J, He Z, Qian D, Meng H, Zhou B, Song Z. Duct-to-mucosa versus invagination pancreaticojejunostomy following pancreaticoduodenectomy: a systematic review and meta-analysis.J Gastrointest Surg 2015;19:1900-1909.
22 Shrikhande SV, Barreto G, Shukla PJ. Pancreatic fistula aer pancreaticoduodenectomy: the impact of a standardized technique of pancreaticojejunostomy. Langenbecks Arch Surg 2008;393:87-91.
23 El Nakeeb A, Hamdy E, Sultan AM, Salah T, Askr W, Ezzat H, et al. Isolated Roux loop pancreaticojejunostomy versus pancreaticogastrostomy aer pancreaticoduodenectomy: a prospective randomized study. HPB (Oxford) 2014;16:713-722.
24 El Nakeeb A, El Hemaly M, Askr W, Abd Ellatif M, Hamed H,Elghawalby A, et al. Comparative study between duct to mucosa and invagination pancreaticojejunostomy aer pancreaticoduodenectomy: a prospective randomized study. Int J Surg 2015;16:1-6.
25 Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 2005;138:8-13.
26 DeOliveira ML, Winter JM, Schafer M, Cunningham SC,Cameron JL, Yeo CJ, et al. Assessment of complications aerpancreatic surgery: a novel grading system applied to 633 patients undergoing pancreaticoduodenectomy. Ann Surg 2006;244:931-939.
27 Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-213.
28 Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery 1992;111:518-526.
29 Hallet J, Zih FS, Deobald RG, Scheer AS, Law CH, Coburn NG, et al.e impact of pancreaticojejunostomy versus pancreaticogastrostomy reconstruction on pancreatic fistula aer pancreaticoduodenectomy: meta-analysis of randomized controlled trials. HPB (Oxford) 2015;17:113-122.
30 Liu FB, Chen JM, Geng W, Xie SX, Zhao YJ, Yu LQ, et al.Pancreaticogastrostomy is associated with significantly less pancreatic fistula than pancreaticojejunostomy reconstruction aer pancreaticoduodenectomy: a meta-analysis of seven randomized controlled trials. HPB (Oxford) 2015;17:123-130.
31 Menahem B, Guittet L, Mulliri A, Alves A, Lubrano J. Pancreaticogastrostomy is superior to pancreaticojejunostomy for prevention of pancreatic fistula aer pancreaticoduodenectomy: an updated meta-analysis of randomized controlled trials.Ann Surg 2015;261:882-887.
32 Chen Z, Song X, Yang D, Li Y, Xu K, He Y. Pancreaticogastrostomy versus pancreaticojejunostomy aer pancreaticoduodenectomy: a meta-analysis of randomized control trials. Eur J Surg Oncol 2014;40:1177-1185.
33 Xiong JJ, Tan CL, Szatmary P, Huang W, Ke NW, Hu WM, et al. Meta-analysis of pancreaticogastrostomy versus pancreaticojejunostomy aer pancreaticoduodenectomy. Br J Surg 2014;101:1196-1208.
34 Lai EC, Lau SH, Lau WY. Measures to prevent pancreatic fistula aer pancreatoduodenectomy: a comprehensive review.Arch Surg 2009;144:1074-1080.
35 Guerrini GP, Soliani P, D'Amico G, Di Benedetto F, Negri M,Piccoli M, et al. Pancreaticojejunostomy versus pancreaticogastrostomy aer pancreaticoduodenectomy: an up-to-date meta-analysis. J Invest Surg 2016;29:175-184.
36 Fang WL, Su CH, Shyr YM, Chen TH, Lee RC, Tai LC, et al.Functional and morphological changes in pancreatic remnant aer pancreaticoduodenectomy. Pancreas 2007;35:361-365.
37 Rault A, SaCunha A, Klopfenstein D, Larroudé D, Epoy FN,Collet D, et al. Pancreaticojejunal anastomosis is preferable to pancreaticogastrostomy aer pancreaticoduodenectomy for longterm outcomes of pancreatic exocrine function. J Am Coll Surg 2005;201:239-244.
38 Lemaire E, O'Toole D, Sauvanet A, Hammel P, Belghiti J,Ruszniewski P. Functional and morphological changes in the pancreatic remnant following pancreaticoduodenectomy with pancreaticogastric anastomosis. Br J Surg 2000;87:434-438.
39 Nakamura H, Murakami Y, Uemura K, Hayashidani Y, Sudo T, Ohge H, et al. Predictive factors for exocrine pancreatic insufficiency aer pancreatoduodenectomy with pancreaticogastrostomy. J Gastrointest Surg 2009;13:1321-1327.
40 Tran TC, van ‘t Hof G, Kazemier G, Hop WC, Pek C, van Toorenenbergen AW, et al. Pancreatic fibrosis correlates with exocrine pancreatic insufficiency aer pancreatoduodenectomy.Dig Surg 2008;25:311-318.
41 Hirono S, Murakami Y, Tani M, Kawai M, Okada K, Uemura K, et al. Identification of risk factors for pancreatic exocrine insufficiency aer pancreaticoduodenectomy using a 13C-labeled mixed triglyceride breath test. World J Surg 2015;39:516-525.
42 Suzuki Y, Fujino Y, Tanioka Y, Hiraoka K, Takada M, Ajiki T, et al. Selection of pancreaticojejunostomy techniques according to pancreatic texture and duct size. Arch Surg 2002;137:1044-1048.
43 Zovak M, Mužina Mžić D, Glavčić G. Pancreatic surgery: evolution and current tailored approach. Hepatobiliary Surg Nutr 2014;3:247-258.
44 Tomimaru Y, Takeda Y, Kobayashi S, Marubashi S, Lee CM,Tanemura M, et al. Comparison of postoperative morphological changes in remnant pancreas between pancreaticojejunostomy and pancreaticogastrostomy aer pancreaticoduodenectomy. Pancreas 2009;38:203-207.
45 Ishikawa O, Ohigashi H, Eguchi H, Yokoyama S, Yamada T,Takachi K, et al. Long-term follow-up of glucose tolerance function aer pancreaticoduodenectomy: comparison between pancreaticogastrostomy and pancreaticojejunostomy. Surgery 2004;136:617-623.
46 Lygidakis NJ, Jain S, Sacchi M, Vrachnos P. Reappraisal of a method of reconstruction aer pancreatoduodenectomy.Hepatogastroenterology 2005;52:1077-1082.
47 Yamamoto Y, Sakamoto Y, Nara S, Esaki M, Shimada K, Kosuge T. A preoperative predictive scoring system for postoperative pancreatic fistula aer pancreaticoduodenectomy. World J Surg 2011;35:2747-2755.
48 Gaujoux S, Cortes A, Couvelard A, Noullet S, Clavel L, Rebours V, et al. Fatty pancreas and increased body mass index are risk factors of pancreatic fistula aer pancreaticoduodenectomy. Surgery 2010;148:15-23.
49 Chen JY, Feng J, Wang XQ, Cai SW, Dong JH, Chen YL. Risk scoring system and predictor for clinically relevant pancreatic fistula aer pancreaticoduodenectomy. World J Gastroenterol 2015;21:5926-5933.
50 Roberts KJ, Sutcliffe RP, Marudanayagam R, Hodson J, Isaac J, Muiesan P, et al. Scoring system to predict pancreatic fistula aer pancreaticoduodenectomy: a UK multicenter study. Ann Surg 2015;261:1191-1197.
51 Vallance AE, Young AL, Macutkiewicz C, Roberts KJ, Smith AM. Calculating the risk of a pancreatic fistula aer a pancreaticoduodenectomy: a systematic review. HPB (Oxford)2015;17:1040-1048.
October 8, 2016
Accepted after revision June 15, 2017
Author Affiliations: Gastroenterology Surgical Center, Mansoura University, Mansoura 35516, Egypt (El Nakeeb A, Sultan AM, Atef E, Salem A, Abu Zeid M, Abu El Eneen A, El Ebidy G and Abdel Wahab M)
Ayman El Nakeeb, MD, Professor of General Surgery, Gastroenterology Surgical Center, Mansoura University, Mansoura 35516, Egypt (Tel: +20-10-6752021; Email: elnakeebayman@yahoo.com)© 2017, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(17)60051-1
Published online August 8, 2017.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Letters to the Editor
- The “Colonial Wig” pancreaticojejunostomy:zero leaks with a novel technique for reconstruction after pancreaticoduodenectomy
- Risk factors and managements of hemorrhage associated with pancreatic fistula after pancreaticoduodenectomy
- Helicobacter pyloriand 17β-estradiol induce human intrahepatic biliary epithelial cell abnormal proliferation and oxidative DNA damage
- Prospective comparison of prophylactic antibiotic use between intravenous moxifloxacin and ceftriaxone for high-risk patients with post-ERCP cholangitis
- Comparative study of the effects of terlipressin versus splenectomy on liver regeneration after partial hepatectomy in rats