阿托伐他汀片对2型糖尿病肾病患者血清chemerin水平的影响
2017-09-12陈小盼陈竑陈韩李大伟韩倩菲云川孙胜花
陈小盼,陈竑,陈韩,李大伟,韩倩菲,云川,孙胜花
(海南医学院第一附属医院内分泌科1、检验科2,海南海口570102)
阿托伐他汀片对2型糖尿病肾病患者血清chemerin水平的影响
陈小盼1,陈竑1,陈韩2,李大伟1,韩倩菲1,云川1,孙胜花1
(海南医学院第一附属医院内分泌科1、检验科2,海南海口570102)
目的观察长期口服HMG-CoA还原酶抑制剂阿托伐他汀片后2型糖尿病肾病(DN)患者尿白蛋白肌酐比值(ACR)和血清chemerin水平的变化,探讨HMG-CoA还原酶抑制剂改善DN尿蛋白的效果及机制。方法收集海南医学院第一附属医院2015年1月至2016年12月门诊和住院诊断的60例DN患者,采用随机数表法将患者分为对照组和观察组,每组30例。两组患者均予以注射24周的胰岛素控制血糖,观察组同时给予阿托伐他汀片口服24周(20 mg/d)。实验室检测两组患者治疗前后的空腹血糖(FPG)、糖化血红蛋白(HbA1c)、甘油三酯(TG)、总胆固醇(TC)、低密度脂蛋白(LDL)、血肌酐(Cr)、尿素氮(BUN)、ACR以及血清chemerin、肿瘤坏死因子-α (TNF-α)浓度。结果治疗24周后,两组患者的BUN、Cr均无明显变化,而FBG、HbA1c均较治疗前明显下降,且差异均有统计学意义(P<0.05),但两组间下降程度比较差异均无统计学意义(P>0.05);对照组患者治疗后TG、TC、LDL无明显改变,但观察组则均明显下降,差异均有统计学意义(P<0.05);对照组和观察组治疗前的ACR分别为(173.32±71.23)µg/mg和(168.08±66.29)µg/mg,治疗后分别为(102.09±65.35)µg/mg和(72.08±41.33)µg/mg,两组患者治疗后的ACR均明显下降,但观察组下降较对照组更明显,差异均有统计学意义(P<0.05);治疗前对照组患者的血清chemerin和TNF-α分别为(48.17±11.25)ng/mL、(123.48±31.56)ng/mL,观察组分别为(45.08±11.36)ng/mL和(118.75±34.02)ng/mL,两组间比较差异均无统计学意义(P>0.05);治疗24周后,对照组患者的chemerin和TNF-α下降至(34.60±9.18)ng/mL和(94.66±30.33)ng/mL,观察组下降至(25.23±8.87)ng/mL和(69.20±25.12)ng/mL,治疗前后比较差异均有统计学意义(P<0.05),但是观察组chemerin和TNF-α下降更为明显(P<0.05)。结论长期口服阿托伐他汀片能显著降低DN患者血清的chemerin水平,改善尿蛋白滤过。
糖尿病肾病;阿托伐他汀;chemerin;尿蛋白
糖尿病发病率逐年增加,是危害身体健康的常见病、多发病。随着病情的发展,糖尿病可以造成一系列严重并发症,最终导致肾小球滤过率显著降低,尿中的蛋白含量增高,演变成糖尿病肾病,甚至发展成尿毒症。所以,对于糖尿病肾病的发生发展机制进行研究,探讨其预防和治疗手段具有重要的临床价值。Chemerin是最近发现的一种表达于成熟的脂肪细胞的脂肪因子,已被证实参与炎症反应和各种心血管疾病的发生发展[1]。此外,近年来大量的临床研究证实,HMG-CoA还原酶抑制剂除了已知的改善血脂水平,缓解动脉硬化外还可以延缓2型糖尿病对肾脏的损害[2-3],但其机制仍不清楚。本文通过研究口服阿托伐他汀对2型糖尿病肾病(DN)患者尿白蛋白肌酐比值(ACR)和血清chemerin水平的影响,探讨阿托伐他汀改善糖尿病肾病的可能机理。
1 资料与方法
1.1 一般资料选取海南医学院第一附属医院2015年1月至2016年12月门诊和住院诊断且符合以下入选和排除标准的60例DN患者。入选标准:门诊初诊,符合1999年WHO 2型糖尿病诊断标准及Mogenson糖尿病肾病诊断分期标准[4],确诊2型糖尿病和尿白蛋白肌酐比值(ACR)≥30µg/mg的患者,且未接受过包括饮食、运动和药物的任何治疗。排除标准:合并原发性高血压、肝肾损害、感染、创伤和血清肌酐<150 μmol/L,以及不能服用阿托伐他汀片的患者。60例患者中男性34例,女性26例;年龄42~75岁。采用随机数表法将患者分为对照组和观察组,每组30例。
1.2 治疗方法所有患者人院后均对其饮食以及运动进行控制,限制其糖类与蛋白质的摄取量。两组患者均给予胰岛素控制血糖,依据血糖值调整胰岛素剂量直至血糖达标,胰岛素每日用量40~60 U,治疗24周。观察组同时给予阿托伐他汀片(商品名:立普妥,生产厂家:辉瑞制药有限公司,规格:20 mg/片)连续口服24周,20 mg/d。
1.3 观察指标与检测方法两组患者治疗前均保持稳定的饮食和戒烟戒酒1周,测量及计算身高、体质量、体质量指数(BMI)和收缩压(SBP)、舒张压(DBP)等临床指标。分别在治疗前后空腹抽血送检验科采用自动生化分析仪检测空腹血糖(FPG)、糖化血红蛋白(HbA1c)、总胆固醇(TC)、甘油三酯(TG)、低密度脂蛋白(LDL)、血肌酐(Cr)、尿素氮(BUN)。治疗前后所有患者均留清晨尿标本测即时ACR。采用ELISA法血清检测血清chemerin和肿瘤坏死因子-α(TNF-α)浓度。试剂配制和操作步骤严格按说明书进行,所有标本的检测全部在同一批次完成。
1.4 统计学方法应用SPSS16.0统计软件进行数据分析,计量资料以均数±标准差()表示,组间比较采用t检验,计数资料比较采用χ2检验,均以P<0.05为差异具有统计学意义。
2 结果
2.1 两组患者治疗前的一般资料比较治疗前两组患者的性别、年龄、BMI、SBP、DBP比较差异均无统计学意义(P>0.05),见表1。
2.2 两组患者治疗前后的生化和实验室指标比较治疗前两组患者的血清FBG、HbA1c、TG、TC、LDL、BUN、Cr和ACR比较差异均无统计学意义(P>0.05)。治疗24周后,虽然两组患者的BUN、Cr仍无明显改变,但FBG、HbA1c数值显著下降,且两组间下降的程度差异无统计学意义(P>0.05)。治疗前后对照组血脂指标比较,TG、TC、LDL均无明显改变,但治疗组则有显著的下降(P<0.05)。两组患者治疗后的ACR均明显下降,但观察组下降较对照组更明显,差异均有统计学意义(P<0.05)。治疗前两组患者的chemerin及TNF-α水平比较差异均无统计学意义(P>0.05),治疗24周后,两组患者的chemerin及TNF-α水平均下降,但观察组chemerin和TNF-α下降更明显,差异均有统计学意义(P<0.05),见表2。
表1 两组患者治疗前的一般资料比较()
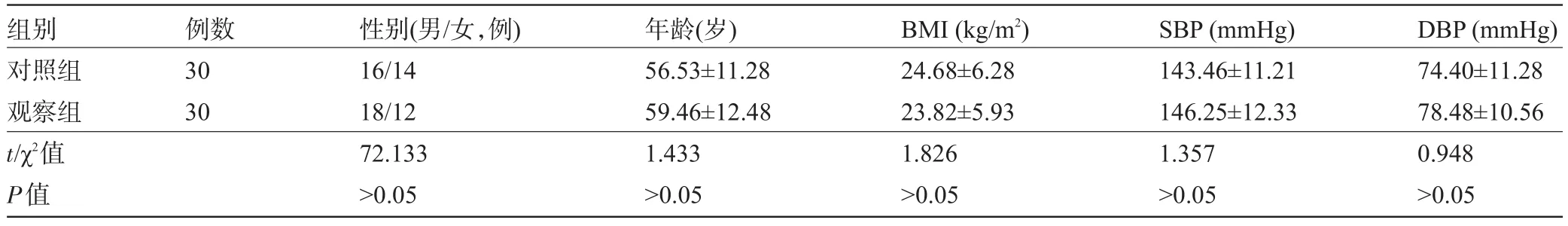
表1 两组患者治疗前的一般资料比较()
注:1 mmHg=0.133 kPa。
组别对照组观察组t/χ2值P值例数30 30性别(男/女,例) 16/14 18/12 72.133>0.05年龄(岁) 56.53±11.28 59.46±12.48 1.433>0.05 BMI(kg/m2) 24.68±6.28 23.82±5.93 1.826>0.05 SBP(mmHg) 143.46±11.21 146.25±12.33 1.357>0.05 DBP(mmHg) 74.40±11.28 78.48±10.56 0.948>0.05
表2 两组患者治疗前后的生化和实验室指标比较()

表2 两组患者治疗前后的生化和实验室指标比较()
注:与对照组治疗后比较,aP<0.05。
组别指标对照组观察组治疗前治疗后t值P值治疗前治疗后t值P值FBG (mmol/L) 9.08±2.77 5.83±1.67 2.148<0.05 9.34±2.81 5.93±2.00 2.365<0.05 HbA1c (%) 7.62±2.01 5.48±2.08 2.365<0.05 8.05±2.46 5.82±2.36 2.511<0.05 TG (µmol/L) 2.09±0.83 2.11±1.01 1.832>0.05 1.86±0.72 1.46±0.80 2.135<0.05 TC (µmol/L) 5.73±1.57 5.47±1.68 1.176>0.05 5.61±1.36 4.30±1.16 2.447<0.05 LDL (µmol/L) 3.46±0.78 3.28±0.83 1.408>0.05 3.61±0.95 2.05±0.47 2.166<0.05 BUN (µmol/L) 7.62±3.43 7.89±3.01 1.674>0.05 8.01±3.88 7.74±3.70 1.802>0.05 Cr (µmol/L) 98.63±16.77 101.86±20.42 1.359>0.05 100.25±22.40 105.28±30.01 1.289>0.05 ACR (µg/mg) 173.32±71.23 102.09±65.35 2.225<0.05 168.08±66.29 72.08±41.33a2.872<0.01 TNF-α (ng/mL) 123.48±31.56 94.66±30.33 2.503<0.05 118.75±34.02 69.20±25.12a2.714<0.01 chemerin (ng/mL) 48.17±11.25 34.60±9.18 2.33<0.05 45.08±11.36 25.23±8.87a2.692<0.01
3 讨论
HMG-CoA还原酶抑制剂是临床常用的调脂药,在动脉硬化性疾病如冠心病、脑梗死的预防和治疗中起重要作用。近年来的临床研究还发现其多种代表药物能改善糖尿病肾病[2-3],但机制仍不清楚,探讨其机制对临床推广使用HMG-CoA还原酶抑制剂改善DN预后有重要的参考价值。在本研究中,观察组与对照组比较,治疗后的ACR明显下降,但两组血糖的下降程度未见明显差异。由此可见,患者ACR的改善不是血糖下降的直接结果,其机理值得进一步探讨。
众所周知,DN的发病机制并不完全清楚,先前的研究已经显示,DN患者血清中的炎症因子如C反应蛋白和IL-6水平与ACR呈正相关,提示炎症过度激活所造成的肾脏损伤是DN形成和加重的重要原因[5-6]。而chemerin是近年来新发现的一种脂肪因子,在组织中广泛分布,在人体炎症反应、调节脂肪细胞分化和代谢等方面发挥着重要作用。有研究报道循环中chemerin水平的增加与炎症因子C反应蛋白、IL-6和TNF-α相关[7]。人肠上皮细胞、小鼠脂肪细胞在富含TNF-α的培养液中培养一段时间后,chemerin的分泌也会明显增多[8]。近年还有研究表明,炎症应答反应可能是chemerin通过调控炎症介质的表达和分泌引起,chemerin对持久的慢性炎症产生潜在的积极作用[9]。此外,炎症部位的chemerin水平升高可能是机体通过调节免疫细胞的聚集而发挥直接促炎症作用的。因此,可以推测chemerin可能通过调控炎症反应而参与糖尿病肾病的发生发展。
本研究中,观察组患者的TNF-α和chemerin水平较对照组明显下降,且血清TNF-α与chemerin水平成明显正相关,因此长期口服HMG-CoA还原酶抑制剂代表药物阿托伐他汀片可能通过降低chemerin水平,调控机体和组织的炎症反应而改善糖尿病肾病。但是,HMG-CoA还原酶抑制剂降低chemerin而改善DN的具体分子机制有待进一步研究。
[1]Sawicka M,Janowska J,Chudek J.Potential beneficial effect of some adipokines positively correlated with the adipose tissue content on the cardiovascular system[J].Int J Cardiol,2016,222:581-589.
[2]Abe M,Maruyama N,Okada K,et al.Effects of lipid-lowering therapy with rosuvastatin on kidney function and oxidative stress in patients with diabetic nephropathy[J].J Atheroscler Thromb,2011,18 (11):1018-1028.
[3]Götz AK,Böger CA,Hirschmann C,et al.Effect of HMG-CoA-reductase inhibitors on survival in type 2 diabetes patients with end stage diabetic nephropathy[J].Eur J Med Res,2005,10(4):155-160.
[4]Mogenson CE.The stages in diabetic renal disease with emphasis on the stage of incipient diabetic nephropathy[J].Diabetes,1993,32 (Suppl2):S64-S78.
[5]Liu F,Guo J,Zhang Q,et al.The expression of tristetraprolin and Its relationship with urinary proteins in patients with diabetic nephropathy[J].PLoS One,2015,10(10):e0141471.
[6]Shelbaya S,Amer H,Seddik S,et al.Study of the role of interleukin-6 and highly sensitive C-reactive protein in diabetic nephropathy in type 1 diabetic patients[J].Eur Rev Med Pharmacol Sci,2012,16 (2):176-182.
[7]Zhang O,Ji Q,Lin Y,et al.Circulating chemerin levels elevated in dilated cardiomyopathy patients with overt heart failure[J].Clin Chim Acta,2015,448:27-32.
[8]Maheshwari A,Kurundkar AR,Shaik SS,et al.Epithelial cells in fetal intestine produce chemerin to recruit macrophages[J].Am J Physiol Gastrointest Liver Physiol,2009,297(1):G1-G10.
[9]Herová M,Schmid M,Gemperle C,et al.Low dose aspirin is associated with plasma chemerin levels and may reduce adipose tissue inflammation[J].Atherosclerosis,2014,235(2):256-262.
Effects of atorvastatin on the levels of serum chemerin in patients with type 2 diabetic nephropathy.
CHEN Xiao-pan1,CHEN Hong1,CHEN Han2,LI Da-wei1,HAN Qian-fei1,YUN Chuan1,SUN Sheng-hua1.Department of Endocrinology1,Department of Clinical Laboratory2,the First Affiliated Hospital of Hainan Medical College,Haikou 570102,Hainan,CHINA
ObjectiveTo observe the changes of urine albumin creatinine ratio(ACR)and serum chemerin levels in type 2 diabetic nephropathy(DN)after taking the 3-hydroxy-3-methylglutaryl-coenzyme A(HMG-CoA)reductase inhibitor atorvastatin for long time,to investigate the effect and mechanism of HMG-CoA reductase inhibitor in improving DN protein.MethodsA total of 60 patients with DN,who admitted to the First Affiliated Hospital of Hainan Medical College from January 2015 to December 2016,were selected and divided randomly into the control group(n= 30)and the observation group(n=30).The patients in both groups were given human insulin injection to control the blood glucose for 24 weeks.In addition,atorvastatin tablet was given in the observation group for 24 weeks(20 mg/d). The fasting plasma glucose(FPG),glycosylated hemoglobin(HbA1c),triglycerides(TG),total cholesterol(TC),low density lipoprotein(LDL),serum creatinine(Cr),urea nitrogen(BUN),ACR and serum chemerin,tumor necrosis factor-α(TNF-α)concentration in both groups before and after treatment were tested.ResultsAlthough BUN and Cr after treatment for 24 weeks in both groups had no obvious change,FBG and HbA1c significantly decreased and the differences were statistically significant(P<0.05).The TG,TC and LDL were not significantly changed after treatment in the control group,but they were significantly reduced in the observation group(P<0.05).The values of ACR of the observation group and the control group were respectively(173.32±71.23)μg/mg and(168.08±66.29)μg/mg before treatment, which were significantly higher than(102.09±65.35)μg/mg and(72.08±41.33)μg/mg after the treatment,and the decreasing in the observation group was more obvious than that in the control group(P<0.05).The serum chemerin and TNF-α in the control group before treatment were(48.17±11.25)ng/mL and(123.48±31.56)ng/mL,respectively,which were higher than(45.08±11.36)ng/mL and(118.75±34.02)ng/mL in the observation group,and the differences between the two groups were not statistically significant(P>0.05).After treatment for 24 weeks,serum chemerin and TNF-α inthe control group dropped to(34.60±9.18)ng/mL and(94.66±30.33)ng/mL,while those dropped to(25.23±8.87)ng/mL and(69.20±25.12)ng/mL in the observation group,and the differences before and after the treatment in both groups were statistically significant(P<0.05),but the decreasing in the observation group was more significantly than those in the control group(P<0.05).ConclusionTaking atorvastatin tablets for a long time could significantly reduce the serum levels of chemerin and improve the filtration of urine protein in patients with DN.
Diabetic nephropathy;Atorvastatin;Chemerin;Urine albumin
R587.2
A
1003—6350(2017)16—2596—03
10.3969/j.issn.1003-6350.2017.16.005
2017-05-27)
海南省教育厅科研基金(编号:Hnky2015-39)
陈小盼。E-mail:xiaopanchen115@sina.com