63例特应性皮炎患者过敏原检测结果分析
2017-09-03潘珂
潘珂
(四川省绵阳市妇幼保健院检验科,四川绵阳 621000)
63例特应性皮炎患者过敏原检测结果分析
潘珂
(四川省绵阳市妇幼保健院检验科,四川绵阳 621000)
目的:分析本地区特应性皮炎(Atopic dermatitis,AD)患者过敏原检测结果,为本地区AD的预防提供参考依据。方法:使用ELISA方法检测我院2016年1月至2017年1月收治AD患者血清总免疫球蛋白E(IgE)及特异性IgE抗体(sIgE),并分析其过敏原表达情况。结果:63例患者中,36例<6岁,占57.14%,纳入学龄前组,其余27例年龄6~15岁,占42.86%,纳入学龄期组。学龄前组、学龄期组血清总IgE阳性率分别为55.56%、59.26%,其sIgE阳性率分别为58.33%、55.56%,组间比较差异均无统计学意义(P>0.05)。患者过敏原以点青霉/烟曲霉/交链胞霉、艾蒿、狗毛等吸入性过敏原以及芒果/菠萝/苹果/桃/草莓等食入性过敏原为主;学龄期组霉菌过敏原构成比高于学龄前组,其芒果/菠萝/苹果/桃/草莓过敏原构成比低于后者,差异有统计学意义(P<0.05)。结论:AD患者血清总IgE及sIgE阳性率均较高且无年龄差异,学龄前患者过敏原以食入性为主,学龄期儿童以吸入性为主,据此实施食物回避与防护措施有望降低人群AD发生率。
特应性皮炎;过敏原;免疫球蛋白E
特应性皮炎(Atopic dermatitis,AD)好发于儿童并可持续至成年期,患者临床症状以瘙痒、多形性皮损及渗出倾向为主,部分可出现哮喘或过敏性鼻炎[1]。AD的发病机制十分复杂,遗传、皮肤屏障功能障碍、免疫、环境等因素均可能参与AD的发生发展,但目前尚未明确AD发病的确切诱因[2]。因此,当前临床对于AD尚无理想的治疗方法,而了解患者过敏原分布,对于避免接触过敏原、改善患者临床症状具有重要意义[3]。本研究对我院2016年1月至2017年1月收治的64例AD患者过敏原检测结果进行汇总分析,旨在了解其过敏原分布,为临床防治提供参考。
1 对象与方法
1.1 对象
入组患者既往无寄生虫感染史,排除入组前2周内有糖皮质激素或免疫抑制剂使用史及入组前3 d内有抗组胺药物使用史者[4]。64例患者中,男34例,女30例,年龄3~15岁,平均(7.12±1.64)岁,病程2~31个月,平均(17.26±3.95)个月;AD病情严重度Scorad评分[5]26~85分,平均(56.24±15.33)岁。
1.2 检测方法
使用ELISA方法,以敏筛定量过敏原检测系统(苏州浩欧博生物医药有限公司),对患者血清总免疫球蛋白E(IgE)及特异性IgE抗体(sIgE)进行检测,选用过敏原包括吸入性过敏原与食入性过敏原,总IgE<100 IU/mL为正常,总IgE≥100 IU/mL为异常,sIgE≥0.35 IU/mL为阳性[6]。其中,吸入性过敏原包括屋尘螨/粉尘螨、蟑螂、点青霉/烟曲霉/交链胞霉、梧桐、榆树、葎草、艾蒿、豚草、猫毛、狗毛共10种,食入性过敏原包括蛋清/蛋黄、牛奶、鳕鱼/鲑鱼/鲈鱼、虾/蟹/扇贝、牛肉/羊肉、芒果/菠萝/苹果/桃/草莓、花生/开心果/腰果/榛子共7种。
1.3 统计学分析方法
对本临床研究的所有数据采用SPSS18.0进行分析,按照患者年龄分布,将其分别纳入学龄前组(<6岁)及学龄期组(≥6岁),比较两组患者IgE、sIgE阳性率以及过敏原分布,采用χ2检验,以P<0.05为差异有统计学意义。并总结63例患者的过敏原分布特点。
2 结果
63例患者中,36例<6岁,占57.14%,纳入学龄前组,其余27例年龄6~15岁,占42.86%,纳入学龄期组。
学龄前组、学龄期组血清总IgE阳性率分别为55.56%(20/36)、59.26%(16/27),其sIgE阳性率分别为58.33%(21/36)、55.56%(15/27),组间比较差异均无统计学意义(P>0.05)。
患者过敏原以点青霉/烟曲霉/交链胞霉、艾蒿、狗毛等吸入性过敏原,以及芒果/菠萝/苹果/桃/草莓等食入性过敏原为主;学龄期组霉菌构成比高于学龄前组,其芒果/菠萝/苹果/桃/草莓构成比低于后者,差异有统计学意义(P<0.05),见表1、图1。
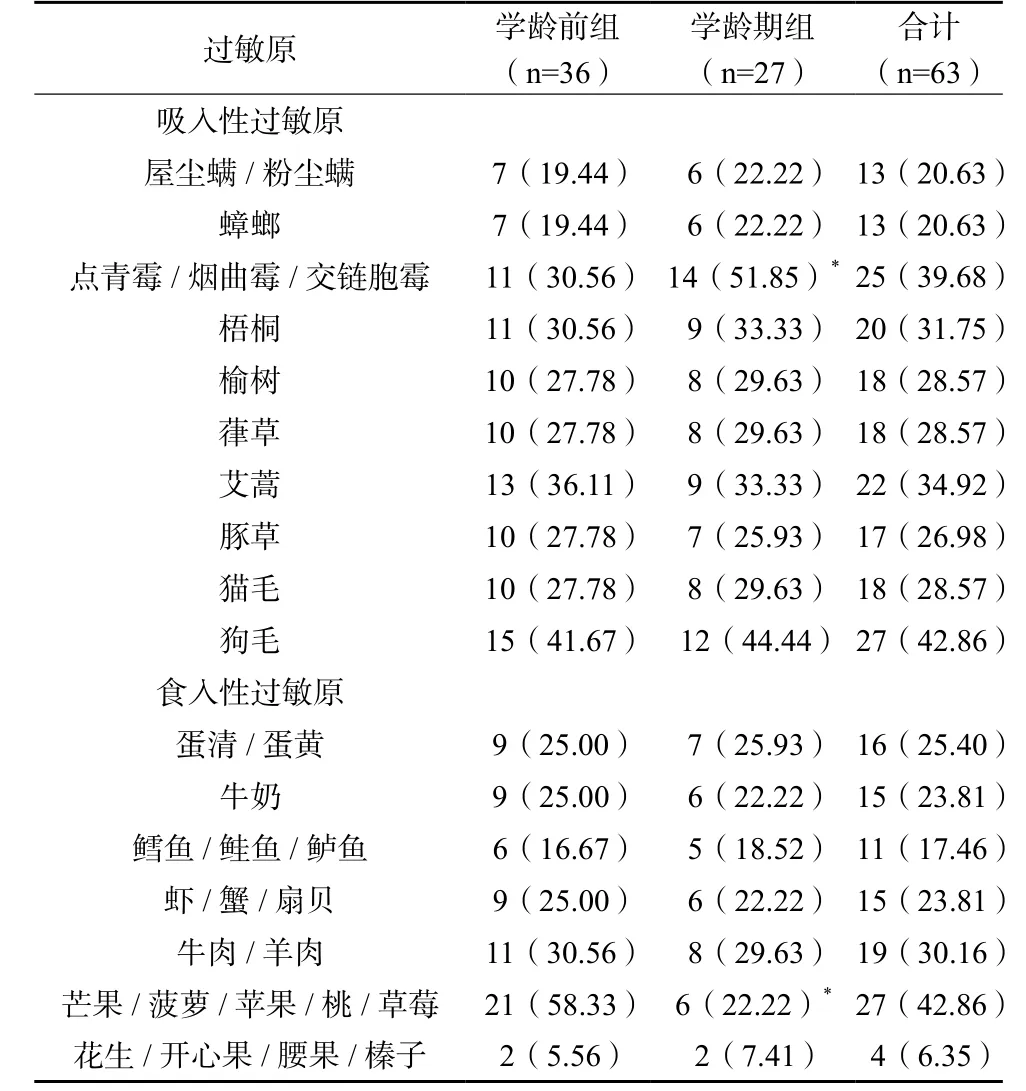
表1 学龄前与学龄期患者过敏原分布比较(n/%)

图1 63例AD患者过敏原检测结果分布
3 讨论
AD发病机制主要为IgE介导的Ⅰ型变态反应,过敏原进入机体所致浆细胞大量分泌sIgE是引发机体致敏状态及相关临床症状的主要原因[7-8]。由于过敏原分布与环境、地理位置、生活习惯存在一定关联,因此,了解当地患者过敏原分布,对于指导AD防治具有价值。我院过敏原检测采用血清总IgE、sIgE表达方法,规避激发试验风险较高、不易被接受的缺陷。结果表明,无论是学龄前还是学龄期患者,其血清总IgE、sIgE阳性率均超过50%,且组间比较差异无统计学意义,说明本地区AD患者中过敏现象占主导,即多数AD患者均有过敏体质,因此,检测血清sIgE亦有助于相关过敏原的明确[9-11]。
在本次研究中,狗毛是AD患者最常见的吸入性过敏原,芒果/菠萝/苹果/桃/草莓是最常见的食入性过敏原,与大量临床研究结果一致[12-15],说明吸入性、食入性过敏原均可诱发AD发生,而空气干燥、越来越多的家庭饲养宠物与监护人盲目给予儿童水果,均是造成儿童AD发生的重要诱因。与此同时,不同年龄段患者过敏原分布存在一定差异,学龄期组吸入性过敏原中霉菌占比较高,考虑与该年龄段人群户外活动增多有关,霉菌大量漂浮于户外空气中,可随呼吸进入人体,诱发特异性变态反应[16],相较于成人而言,儿童对外界环境中的各类抗原因素有着更高的敏感性,故其不仅更易因过敏原引发AD,且临床症状也易因外界感染、季节及气候变化、刺激性物质等原因进一步加重。学龄前组经典性食入性过敏原占比较高,可能与这一阶段,人体在胸腺发育成熟的过程中对体内外抗原的识别逐渐建立导致学龄期儿童对过敏原反应性较高有关[17]。
由于目前AD的治疗尚无特别有效的药物,而长期激素治疗的不良反应较为明显,可能对患者生长发育造成明显影响。因此,在今后的临床实践中,应根据AD患者的年龄特点及所处环境提出针对性临床建议,做到个体化诊治,如对过敏体质学龄前儿童,应谨慎给予水果等副食品,并做到逐个给予,以早期发现可能诱发过敏反应的变应原,并避免AD的诱发与加重[18],而学龄期儿童户外活动前应做好保护措施,日常生活环境中需注重尘螨的清除,并避免皮肤的过度清洗与不洁衣物的长期皮肤接触,从而完善发病因素环节的预防,从根本上降低AD发生率。
总体而言,AD患者普遍存在过敏体质,且其过敏原分布与年龄相关,学龄前患者更易因食物刺激发生AD,而学龄期患者户外活动的增加使其霉菌致敏风险显著提高,应针对患者年龄特点予以综合防治。
[1] BROUGH H A, LIU A H, SICHERER S, et al. Atopic dermatitis increases the effect of exposure to peanut antigen in dust onpeanut sensitization and likely peanut allergy[J]. J Allergy Clin Immunol, 2015, 135(1): 164-170.
[2] 孙婧, 弓娟琴, 姚煦. 特应性皮炎自身免疫发病机制的研究进展[J]. 国际皮肤性病学杂志, 2015, 41(3): 181-183.
[3] MURARO A, LEMANSKE R F, HELLINGS P W, et al. Precision medicine in patients with allergic diseases: airway diseases and atopic dermatitis—PRACTALL document of the European Academy of Allergy and Clinical Immunology and the American Academy of Allergy, Asthma & Immunology[J]. J Allergy Clin Immunol, 2016, 137(5): 1347-1358.
[4] 李慧, 冯海瑕, 俞先水, 等. 2036例过敏相关疾病体外过敏原特异性IgE检测与分析[J]. 国际皮肤性病学杂志, 2014, 40(4): 212-214.
[5] NERMES M, ENDO A, AARNIO J, et al. Furry pets modulate gut microbiota composition in infants at risk for allergic disease[J]. J Allergy Clin Immunol, 2015, 136(6): 1688.
[6] 常曼丽. 过敏性疾病患者过敏原及血清特异性IgE的研究[D].哈尔滨:哈尔滨医科大学, 2013.
[7] HENRIKSEN L, SIMONSEN J, HAERSKJOLD A, et al. Incidence rates of atopic dermatitis, asthma, and allergic rhinoconjunctivitis in Danish and Swedish children[J]. J Allergy Clin Immunol, 2015, 136(2): 360-366.
[8] DA ROSA J C, MALAJIAN D, SHEMER A, et al. Patients with atopic dermatitis have attenuated and distinct contact hypersensitivity responses to common allergens in skin[J]. J Allergy Clin Immunol, 2015, 135(3): 712-720.
[9] 王兰, 李东宁, 孙健, 等. 特应性皮炎常见食物过敏原的特应性斑贴试验结果分析[J]. 中国皮肤性病学杂志, 2014, 28(5): 485-487.
[10] LUCAE S, SCHMID‐GRENDELMEIER P, WÜTHRICH B, et al. IgE responses to exogenous and endogenous allergens in atopic dermatitis patients under long‐term systemic cyclosporine A treatment[J]. Allergy, 2016, 71(1): 115-118.
[11] TSAKOK T, MARRS T, MOHSIN M, et al. Does atopic dermatitis cause food allergy? A systematic review[J]. J Allergy Clin Immunol, 2016, 137(4): 1071-1078.
[12] 姚尧. 延边地区特应性皮炎成人过敏原检测及分析[D]. 延吉:延边大学, 2014.
[13] KELLEHER M, DUNN-GALVIN A, HOURIHANE J O B, et al. Skin barrier dysfunction measured by transepidermal water loss at 2 days and 2 months predates and predicts atopic dermatitis at 1 year[J]. J Allergy Clin Immunol, 2015, 135(4): 930-935.
[14] BANERJEE S, RESCH Y, CHEN K W, et al. Der p 11 is a major allergen for house dust mite-allergic patients suffering from atopic dermatitis[J]. J Invest Dermatol, 2015, 135(1): 102-109.
[15] 折雪. 三种变态反应性皮肤病患者血清过敏原检测分析[D].太原:山西医科大学, 2014.
[16] OLIVRY T, DEBOER D J, FAVROT C, et al. Treatment of canine atopic dermatitis: 2015 updated guidelines from the International Committee on Allergic Diseases of Animals (ICADA)[J]. BMC Vet Res, 2015, 11(1): 210.
[17] WOLLENBERG A, ORANJE A, DELEURAN M, et al. ETFAD/EADV Eczema task force 2015 position paper on diagnosis and treatment of atopic dermatitis in adult and paediatric patients[J]. J Eur Acad Dermatol Venereol, 2016, 30(5): 729-747.
[18] SMITH V M, CLARK S M, WILKINSON M. Allergic contact dermatitis in children: trends in allergens, 10 years on. A retrospective study of 500 children tested between 2005 and 2014 in one UK centre[J]. Contact Dermatitis, 2016, 74(1): 37-43.
The analysis of allergen on 63 cases of atopic dermatitis patients
PAN Ke. (Department of laboratory,Mianyang Maternal and Child Health-Care Hospital,Mianyang 621000 china)
Objective: The objective of this study was to analyze the allergen of AD (atopic dermatitis, AD) patients and provide reference for the prevention of AD of local region. Methods: The igE (immunoglobulin e, igE) and antibiotic of slgE of AD patients treated in our hospital from Jan 2016 to Jan 2017 were tested by means of ELISA (enzyme-linked immuno sorbent assay, ELISA) and their allergen were analyzed. Results: A total of 63 cases were collected, of whom 36 cases were less than 6 years old, accounting for 57.14% and were classif i ed as preschool group and the rest 27 cases aging from 6 to 15, accounting for 42.86% were classif i ed as schooling group. The positive rate of serum igE of two groups were 55.56% and 59.26% respectively and the positive rate of serum igE of them were 58.33% and 55.56%, and the difference was not statistically signif i cant(P>0.05). The most common allergen were allergen of inhalation as penicillium notatum, aspergillus fumigatus, mugwort, dog hair and allergen of edibility as mango, pineapple, apple, peach and strawberry; the constituent ratio of fugous allergen of preschool group was higher than that of schooling group while their constituent ratio of mango, pineapple, apple, peach and strawberry was lower than that of latter group and the difference was statistically signif i cant(P<0.05). Conclusions: The positive rate of both serum igE and slgE of AD patients are high and the age has no difference. The common allergens of preschool patients are edible while the schooling patients are inhaling. It is expected to decrease the AD rate through the avoidance of allergic food and prevention measurements.
atopic dermatitis; allergen; immunoglobulin e
R446
A
2095-5200(2017)04-085-03
10.11876/mimt201704035
潘珂,本科,检验主管技师,研究方向:检验临床,Email:dcq023186@126.com。
