Modif i cations of ALPPS - from complex to more complex or from complex to less complex operations
2017-08-16WanYeeLauandEricCHLai
Wan Yee Lau and Eric CH Lai
Hong Kong, China
Modif i cations of ALPPS - from complex to more complex or from complex to less complex operations
Wan Yee Lau and Eric CH Lai
Hong Kong, China
BACKGROUND:Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) has recently been developed to induce rapid liver hypertrophy to reduce the chance of post-hepatectomy liver failure in patients with borderline or insuff i cient future liver remnant. ALPPS is still in an early developmental stage and its techniques have not been standardized. This study aimed to review the technical modif ications of the conventional ALPPS procedure.
DATA SOURCES:Studies were identif i ed by searching MEDLINE and PubMed for articles published from January 2007 to December 2016 using the keywords “associating liver partition and portal vein ligation for staged hepatectomy” and “ALPPS”. Additional articles were identif i ed by a manual search of references from key articles.
RESULTS:There have been a lot of modif i cations of the conventional ALPPS. These are classif i ed as: (1) modif i cations aiming to improve surgical results; (2) modif i cations aiming to expand surgical indications; (3) salvage ALPPS; (4) ALPPS using the minimally invasive approach. Some of these modifi cations have made the conventional ALPPS procedure to become even more complex, although there have also been other attempts to make the procedure less complex. The results of most of these modi fi cations have been reported in small case series or case reports. We need better well-designed studies to establish the true roles of these modi fi cations. However, it is interesting to see how this conventional ALPPS procedure has evolved since its introduction.
CONCLUSIONS:There is a trend for the use of minimally invasive procedure in the phase 1 or 2 of the conventional ALPPS procedure. Some of these modif i cations have expanded the use of ALPPS in patients who have been considered to have unresectable liver tumors. The long-term oncological outcomes of these modif i cations are still unknown.
(Hepatobiliary Pancreat Dis Int 2017;16:346-352)
associating liver partition and portal vein ligation for staged hepatectomy; hepatocellular carcinoma; hepatectomy; liver metastasis; portal vein embolization
Introduction
Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) is a new strategy which has been developed to induce accelerated hypertrophy of future liver remnant (FLR) in order to increase resectability of liver tumors and reduce the risk of postoperative liver failure. Since its introduction, many surgeons around the world have rapidly adopted ALPPS as it has the advantages of inducing rapid liver hypertrophy of 47% to 100% over a median of 6 to 16 days, and 95% to 100% completion of tumor resection rate for the 2-staged operation.[1-20]Even in patients with chronic liver diseases, severe steatosis, liver fi brosis or cirrhosis, liver hypertrophy rates, although less predictable, have been reported to vary from 18.7% to 100% over a median of 7 days.[21-27]The main criticisms of ALPPS are its high morbidity and mortality rates. The morbidity rates after ALPPS have been reported to be 15.3% to 100% with ≥Clavien-Dindo Grade II being 13.6% to 44%, and the reported mortality rates ranged from 0 to 29%.[1-20]Thus ALPPS is not accepted by some surgeons who believe portal vein embolization or portal vein ligation to be much safer than ALPPS. Because of the longer timeinterval to wait for the FLR to hypertrophy adequately, the risk of drop out from completion of tumor resection is signif i cantly lower in ALPPS, due to either tumor progression or insuff i cient hypertrophy of FLR.[28-32]
Since the introduction of the conventional ALPPS, surgeons have reported on various modif i cations of the procedure, aiming to decrease the perioperative morbidity and mortality rates, to improve postoperative longterm survival and to improve the completion of tumor resection of the ALPPS phase 2 operation. This article aimed to review the technical modif i cations of the conventional ALPPS procedure.
Methods
Studies were identif i ed by searching MEDLINE and PubMed for articles published from January 2007 to December 2016 using the keywords “associating liver partition and portal vein ligation for staged hepatectomy” and“ALPPS”. Additional articles were identif i ed by a manual search of references from key articles. All articles on technical modif i cations of ALPPS were included in this review.
Results
Conventional ALPPS and its initial development
Professor Hans Schlitt from Regensburg, Germany fi rst carried out this operation in 2007. He originally planned to carry out an extended right hepatectomy for a patient with hilar cholangiocarcinoma. During the operation, he found the FLR to be too small for the patient’s survival after surgery. He then decided to carry out a biliary bypass. For optimal exposure and positioning of a jejunal loop for the left hepaticojejunostomy, he carried out anin situsplit of the liver parenchyma on the right side of the falciform ligament. To induce liver hypertrophy of the liver segments 2 and 3, he ligated the right portal vein. Out of curiosity, he performed computed tomography (CT) on postoperative day 9 and found the left lateral section of the liver had adequately hypertrophied. He then carried out the originally planned extended right hepatectomy as a second staged operation. The patient recovered well from the operation. This novel approach was formally presented as a poster presentation on 3 such cases in the 9th European-African Hepato-Pancreato-Biliary Association Congress in Cape Town, South Africa, in 2011 by Dr. Hauke Lang from Mazin, Germany.[33]In the same year, de Santibañes and his colleagues from Argentina adopted this technique and reported their initial experiences on 3 patients.[34]Schlitt and his colleagues reported the technique which they called “right portal vein ligation combined within situsplitting” on 25 patients.[1]Reports started to come from regions around the world with overwhelming enthusiasm. In 2012, de Santibañes and Clavien proposed the acronym for this procedure as associating liver partition and portal vein ligation for staged hepatectomy, or ALPPS in short.[35]Fig. 1 shows the diagrammatic representation of the conventional ALPPS procedure.
Modif i cations of the conventional ALPPS
Although ALPPS is still considered by many surgeons to be in an early developmental phase, and its indications and contraindications have not been well-def i ned, many technical modif i cations of the conventional ALPPS have been successfully carried out and reported. Unfortunately, almost all these reports are case reports or small case series which limit meaningful statistical comparison on treatment outcomes. Validation of success of these techniques are still lacking. Technical standardization of some of these modif i cations is needed before the effectiveness and safety of these modif i cations can be clarif i ed. However, it is interesting to review the gradual changes in the technical modif i cations of the conventional ALPPS and the reasoning behind the modif i cations — a change from complex to more complex, and subsequently from complex to less complex operations using minimally invasive approaches.
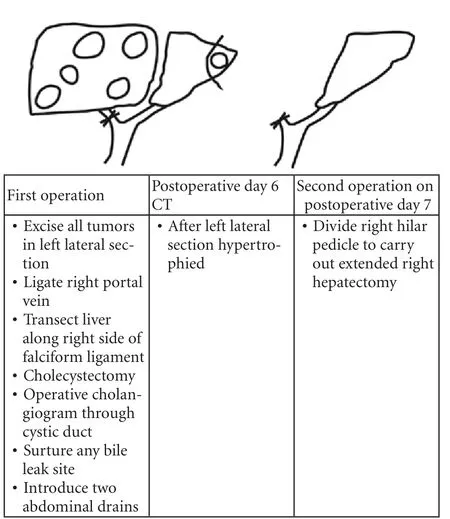
Fig. 1. Conventional ALPPS.
Modif i cations aiming to improve surgical results
The initial aims of introducing modif i cations to the conventional ALPPS were to decrease perioperative morbidity and mortality rates, improve long-term survival, and improve the completion tumor resection rate of the phase II ALPPS. There is still a lack of consensus of adopting the following modif i cations because these modif i cations can result in a more complex operation and some of these modif i cations fail to achieve what they have been designed to achieve. Sometimes, they can even result in worse outcomes. These modif i cations include:
(i) Time interval between the 1st and 2nd phases of ALPPS to extend to be more than 14 days. The main reason is because of inadequate liver hypertrophy of the FLR within the second week after the 1st phase of ALPPS.[36]
(ii) As bile leakage after the 1st phase of ALPPS led to signif i cant morbidity and mortality rates due to sepsis, a plastic bag was introduced to wrap around the liver after liver transection and drains were placed into the plastic bag to drain any body fl uid or bile to outside of the body.[1]However, there are two disadvantages of using a plastic bag. First this is a foreign body which can lead to sepsis. Second, even if a 2nd phase ALPPS cannot be done due to inadequate liver hypertrophy, a second operation still needs to be carried out to remove the plastic bag. As a consequence, the use of bags made of absorbable material or the use of biologic sealant have been proposed.[37,38]
(iii) As the arterial and portal blood supply to liver segment 4 is compromised by liver transection along the right side of the falciform ligament, Andriani and his associates proposed to resect this liver segment in an attempt to decrease any ischemia to liver segment 4 which may become infected.[39]This segment 4 resection is now seldom done as it adds to the complexity without providing any obvious advantage to the surgery.
(iv) Simultaneous ligation of the right hepatic artery, aiming to increase the liver hypertrophy rate.[40]Again this is now seldom carried out as this adds to the complexity without any obvious advantage to the surgery.
(v) To preserve the middle hepatic vein in the left liver aiming to improve venous drainage of the liver segment 4 which may decrease the risk of necrosis and bile leakage.[12]This should be done if technically possible.
(vi) To use the anterior approach with or without the liver hanging technique. The aim is to decrease adhesions formation after the 1st phase of ALPPS. In patients with a large tumor in the right liver, this approach can decrease the chance of tumor rupture during liver mobilization.[17,41]
(vii) The “no touch technique” aiming to improve the long-term results of ALPPS.[42]
Modif i cations aiming to expand surgical indications of the conventional ALPPS by preserving different liver segments
All these modif i cations of the conventional ALPPS increase the technical diff i culty of the operation. However, these modif i cations were designed for patients with liver tumors that were considered to be unresectable even with the conventional ALPPS. There are still not enough data to support whether the long-term results justify the increased risk of these procedures.
(i) To preserve the right liver (liver segments 5, 6, 7, 8)[42](Fig. 2)
(ii) To preserve liver segments 4, 5, 8[36](Fig. 3)
(iii) To preserve the left liver (liver segments 2, 3, 4)[36](Fig. 4)

Fig. 2. Modif i cation to preserve right liver (i.e. segments 5, 6, 7, 8).
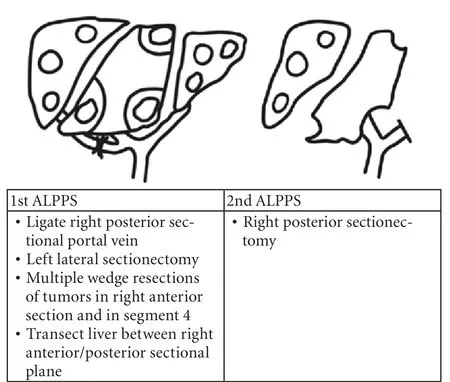
Fig. 3. Modif i cation to preserve liver segments 4, 5, 8.
This is used in patients with a huge liver tumor (>10 cm) in the right liver and the size of the FLR in the left liver is too small. This modif i cation will hopefully resultin adequate liver hypertrophy in the FLR within 1 to 2 weeks. If portal vein embolization or portal vein ligation is to be used, the wait needs to be 4 to 6 weeks before resectional surgery can be carried out. By then the tumor may have progressed to become unresectable.
(iv) Doublein situliver split for staged mesohepatectomy (Fig. 5)
This is used in patients with gallbladder cancer.[43]The operation requires resection of liver segments 1, 4, 5, 8 with preservation of liver segments 2, 3, and 6, 7. Right and left hepaticojejunostomy and regional lymphadenectomy form parts of the operation.
(v) Monosegment ALPPS
The operation includes resection of all liver segments but leaving behind:[44-46]
·Segment 2+1/2 segment 4
·Segment 3+segment 1
·Segment 4+segment 1 or (+) 1/4 segment 2
·Segment 6+segment 1
Salvage ALPPS[47,48]
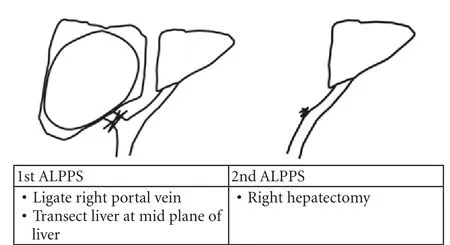
Fig. 4. Modif i cation to preserve left liver (i.e. liver segments 2, 3, 4).

Fig. 5. Doublein situsplit for staged mesohepatectomy. IVC: inferior vena cava.
Sometimes, either a right or left portal vein embolization results in inadequate liver hypertrophy in the FLR. Salvage ALPPS is carried out by parenchymal transection along the mid plane of the liver between the right and the left liver. The 2nd phase ALPPS can be carried out when the FLR has hypertrophied to an adequate size by carrying out a right or a left hepatectomy.
ALPPS using the minimally invasive approach
The main aim of using the minimally invasive approach in ALPPS is to reduce surgical trauma. However, using minimally invasive procedures in ALPPS can become technically more diff i cult. Whether the reduced surgical trauma in the minimally invasive procedures can result in better overall surgical outcomes is still unknown.
ALPPS involves 2 phases of a staged operation. For these two operations the approaches can vary from: open surgery, to hand-assisted laparoscopic, to totally laparoscopic, to robotic, and then to percutaneous interventional procedures.
The fi rst phase of ALPPS involves 2 major components:
[A] Liver partition — this can vary from open liver parenchymal transection, to laparotomy+liver tourniquet, to open radiofrequency/microwave for liver parenchymal partition, to laparoscopic liver transection, to laparoscopic liver tourniquet, to laparoscopic radiofrequency/microwave for liver parenchymal partition, and to percutaneous radiofrequency/microwave for liver parenchymal partition.
[B] For blockage of a portal vein branch, it can vary from open portal vein ligation, to laparoscopic portal vein ligation, to percutaneous portal vein embolization.
The second phase of ALPPS involves liver resection which can vary from open, to laparoscopic, to robotic liver resection.
The development of the modif i cations of ALPPS using the minimally invasive approach, involves the various combinations of the above mentioned procedures.
The development can be divided into 3 stages (Table).
(i) Phase 1 of ALPPS uses minimally invasive surgery Phase 2 of ALPPS uses open liver resection
(ii) Phase 1 of ALPPS uses minimally invasive procedures Phase 2 of ALPPS uses laparoscopic or robotic liver resection
(iii) Phases 1 of ALPPS uses percutaneous procedures Phase 2 of ALPPS uses open liver resection
The study by Hong et al[62]using totally percutaneous procedures in the fi rst phase of ALPPS is interesting. The main merits are (i) the percutaneous procedures decrease harm on patients who otherwise have to undergo two major surgical procedures within a time interval of 1 to 2 weeks; and (ii) this 1st phase of ALPPS can be used as a screening procedure to screen out patients who donot have good degree of liver hypertrophy after the 1st phase of ALPPS. The success of this operation is based on the following two observed facts which have been previously reported:

Table. Modif i cations of ALPPS using minimally invasive procedures
(i) There is no difference between the degree of liver hypertrophy in the FLR in partial and complete partition using radiofrequency ablation/microwave[18,63-66]
(ii) After liver partition, percutaneous portal vein embolization can give a similar degree of liver hypertrophy as intraoperative portal vein ligation.[49,62,67]The major precaution that should be taken is the chance of damaging the blood supply to liver segments 2 and 3 if there is too excessive ablation using radiofrequency ablation or microwave on the right side of the falciform ligament, as the blood supply of the left liver (segments 2, 3, 4) goes along the umbilical fi ssure to supply segment 4 on the right side and segments 2, 3 on the left side.
Conclusions
There have been a lot of modif i cations of the conventional ALPPS. Some of these modif i cations made the conventional ALPPS even more complex, although other attempts to make the procedure less complex.
The results of most of these modif i cations have been reported in small case series or case reports. We need well-designed studies to establish the true roles of these modif i cations.
Contributors: LWY proposed the study. Both authors contributed to the design and interpretation of the study and to further drafts. LWY is the guarantor.
Funding: None.
Ethical approval: Not needed.
Competing interest: No benef i ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA, et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg 2012;255:405-414.
2 Sala S, Ardiles V, Ulla M, Alvarez F, Pekolj J, de Santibañes E. Our initial experience with ALPPS technique: encouraging results. Updates Surg 2012;64:167-172.
3 Torres OJ, Fernandes Ede S, Oliveira CV, Lima CX, Waechter FL, Moraes-Junior JM, et al. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): the Brazilian experience. Arq Bras Cir Dig 2013;26:40-43.
4 Li J, Girotti P, Königsrainer I, Ladurner R, Königsrainer A, Nadalin S. ALPPS in right trisectionectomy: a safe procedure to avoid postoperative liver failure? J Gastrointest Surg 2013;17:956-961.
5 Ielpo B, Caruso R, Ferri V, Quijano Y, Duran H, Diaz E, et al. ALPPS procedure: our experience and state of the art. Hepatogastroenterology 2013;60:2069-2075.
6 Troja A, Khatib-Chahidi K, El-Sourani N, Antolovic D, Raab HR. ALPPS and similar resection procedures in treating ex-tensive hepatic metastases: our own experiences and critical discussion. Int J Surg 2014;12:1020-1022.
7 Oldhafer KJ, Donati M, Jenner RM, Stang A, Stavrou GA. ALPPS for patients with colorectal liver metastases: effective liver hypertrophy, but early tumor recurrence. World J Surg 2014;38:1504-1509.
8 Nadalin S, Capobianco I, Li J, Girotti P, Königsrainer I, Königsrainer A. Indications and limits for associating liver partition and portal vein ligation for staged hepatectomy (ALPPS). Lessons learned from 15 cases at a single centre. Z Gastroenterol 2014;52:35-42.
9 Robles R, Parrilla P, López-Conesa A, Brusadin R, de la Peña J, Fuster M, et al. Tourniquet modif i cation of the associating liver partition and portal ligation for staged hepatectomy procedure. Br J Surg 2014;101:1129-1134.
10 Schadde E, Ardiles V, Robles-Campos R, Malago M, Machado M, Hernandez-Alejandro R, et al. Early survival and safety of ALPPS: fi rst report of the International ALPPS Registry. Ann Surg 2014;260:829-838.
11 Kremer M, Manzini G, Hristov B, Polychronidis G, Mokry T, Sommer CM, et al. Impact of neoadjuvant chemotherapy on hypertrophy of the future liver remnant after associating liver partition and portal vein ligation for staged hepatectomy. J Am Coll Surg 2015;221:717-728.
12 Hernandez-Alejandro R, Bertens KA, Pineda-Solis K, Croome KP. Can we improve the morbidity and mortality associated with the associating liver partition with portal vein ligation for staged hepatectomy (ALPPS) procedure in the management of colorectal liver metastases? Surgery 2015;157:194-201.
13 Truant S, Scatton O, Dokmak S, Regimbeau JM, Lucidi V, Laurent A, et al. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): impact of the inter-stages course on morbi-mortality and implications for management. Eur J Surg Oncol 2015;41:674-682.
14 Alvarez FA, Ardiles V, de Santibañes M, Pekolj J, de Santibañes E. Associating liver partition and portal vein ligation for staged hepatectomy offers high oncological feasibility with adequate patient safety: a prospective study at a single center. Ann Surg 2015;261:723-732.
15 Lang SA, Loss M, Benseler V, Glockzin G, Schlitt HJ. Longterm results after in-situ split (ISS) liver resection. Langenbecks Arch Surg 2015;400:361-369.
16 Vivarelli M, Vincenzi P, Montalti R, Fava G, Tavio M, Coletta M, et al. ALPPS procedure for extended liver resections: A single centre experience and a systematic review. PLoS One 2015;10:e0144019.
17 Chan AC, Poon RT, Chan C, Lo CM. Safety of ALPPS procedure by the anterior approach for hepatocellular carcinoma. Ann Surg 2016;263:e14-16.
18 Røsok BI, Björnsson B, Sparrelid E, Hasselgren K, Pomianowska E, Gasslander T, et al. Scandinavian multicenter study on the safety and feasibility of the associating liver partition and portal vein ligation for staged hepatectomy procedure. Surgery 2016;159:1279-1286.
19 Serenari M, Zanello M, Schadde E, Toschi E, Ratti F, Gringeri E, et al. Importance of primary indication and liver function between stages: results of a multicenter Italian audit of ALPPS 2012-2014. HPB (Oxford) 2016;18:419-427.
20 Björnsson B, Sparrelid E, Hasselgren K, Gasslander T, Isaksson B, Sandström P. Associating liver partition and portal vein ligation for primary hepatobiliary malignancies and noncolorectal liver metastases. Scand J Surg 2016;105:158-162.
21 Cavaness KM, Doyle MB, Lin Y, Maynard E, Chapman WC. Using ALPPS to induce rapid liver hypertrophy in a patient with hepatic fi brosis and portal vein thrombosis. J Gastrointest Surg 2013;17:207-212.
22 Chia NH, Lai EC, Lau WY. Associating liver partition and portal vein ligation for a patient with hepatocellular carcinoma with a background of hepatitis B related fi brotic liver. Int J Surg Case Rep 2014;5:1077-1081.
23 Vennarecci G, Laurenzi A, Santoro R, Colasanti M, Lepiane P, Ettorre GM. The ALPPS procedure: a surgical option for hepatocellular carcinoma with major vascular invasion. World J Surg 2014;38:1498-1503.
24 Vennarecci G, Laurenzi A, Levi Sandri GB, Busi Rizzi E, Cristofaro M, Montalbano M, et al. The ALPPS procedure for hepatocellular carcinoma. Eur J Surg Oncol 2014;40:982-988.
25 Papamichail M, Pizanias M, Yip V, Prassas E, Prachalias A, Quaglia A, et al. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) procedure for hepatocellular carcinoma with chronic liver disease: a case report and review of literature. Korean J Hepatobiliary Pancreat Surg 2016;20:75-80.
26 D’Haese JG, Neumann J, Weniger M, Pratschke S, Björnsson B, Ardiles V, et al. Should ALPPS be used for liver resection in intermediate-stage HCC? Ann Surg Oncol 2016;23:1335-1343.
27 Schadde E, Raptis DA, Schnitzbauer AA, Ardiles V, Tschuor C, Lesurtel M, et al. Prediction of mortality after ALPPS stage-1:an analysis of 320 patients from the International ALPPS Registry. Ann Surg 2015;262:780-786.
28 Knoefel WT, Gabor I, Rehders A, Alexander A, Krausch M, Schulte am Esch J, et al. In situ liver transection with portal vein ligation for rapid growth of the future liver remnant in two-stage liver resection. Br J Surg 2013;100:388-394.
29 Shindoh J, Vauthey JN, Zimmitti G, Curley SA, Huang SY, Mahvash A, et al. Analysis of the eff i cacy of portal vein embolization for patients with extensive liver malignancy and very low future liver remnant volume, including a comparison with the associating liver partition with portal vein ligation for staged hepatectomy approach. J Am Coll Surg 2013;217:126-134.
30 Schadde E, Ardiles V, Slankamenac K, Tschuor C, Sergeant G, Amacker N, et al. ALPPS offers a better chance of complete resection in patients with primarily unresectable liver tumors compared with conventional-staged hepatectomies: results of a multicenter analysis. World J Surg 2014;38:1510-1519.
31 Ratti F, Schadde E, Masetti M, Massani M, Zanello M, Serenari M, et al. Strategies to Increase the resectability of patients with colorectal liver metastases: a multi-center case-match analysis of ALPPS and conventional two-stage hepatectomy. Ann Surg Oncol 2015;22:1933-1942.
32 Tanaka K, Matsuo K, Murakami T, Kawaguchi D, Hiroshima Y, Koda K, et al. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): short-term outcome, functional changes in the future liver remnant, and tumor growth activity. Eur J Surg Oncol 2015;41:506-512.
33 Baumgart J, Lang S, Lang H. A new method for induction of liver hypertrophy prior to right trisectionectomy: a report of three cases. HPB 2011;13:71-72.
34 de Santibañes E, Alvarez FA, Ardiles V. How to avoid postoperative liver failure: a novel method. World J Surg 2012;36:125-128.
35 de Santibañes E, Clavien PA. Playing Play-Doh to prevent postoperative liver failure: the “ALPPS” approach. Ann Surg 2012;255:415-417.
36 Lau WY, Lau SH. Surgical modif i cations on the conventional ALPPS. Chin J Pract Surg 2016;36:93-95.
37 Brustia R, Scatton O, Soubrane O. Variation on a theme: Alternative to plastic bag in ALPPS procedures: feasibility and clinical safety of COVA+™ membrane in ALPPS procedures. World J Surg 2015;39:3023-3027.
38 Brustia R, Scatton O, Perdigao F, El-Mouhadi S, Cauchy F, Soubrane O. Vessel identif i cations tags for open or laparoscopic associating liver partition and portal vein ligation for staged hepatectomy. J Am Coll Surg 2013;217:e51-55.
39 Andriani OC. Long-term results with associating liver partition and portal vein ligation for staged hepatectomy (ALPPS). Ann Surg 2012;256:e5; author reply e16-19.
40 Dokmak S, Belghiti J. Which limits to the “ALPPS” approach? Ann Surg 2012;256:e6; author reply e16-17.
41 Vennarecci G, Levi Sandri GB, Ettorre GM. Performing the ALPPS procedure by anterior approach and liver hanging maneuver. Ann Surg 2016;263:e11.
42 Bertens KA, Hawel J, Lung K, Buac S, Pineda-Solis K, Hernandez-Alejandro R. ALPPS: challenging the concept of unresectability--a systematic review. Int J Surg 2015;13:280-287.
43 Tsui TY, Heumann A, Vashist YK, Izbicki JR. How we do it:double in situ split for staged mesohepatectomy in patients with advanced gall bladder cancer and marginal future liver remnant. Langenbecks Arch Surg 2016;401:565-571.
44 Montalvá Orón EM, Maupoey Ibáñez J, Bañuelos Carrillo R, Boscà Robledo A, Orbis Castellanos JF, Moya Herraiz á, et al. Monosegment ALPPS: A new variant of the techniques for rapid hepatic regeneration. Critical review of the initial results of our series. Cir Esp 2015;93:436-443.
45 Schadde E, Malagó M, Hernandez-Alejandro R, Li J, Abdalla E, Ardiles V, et al. Monosegment ALPPS hepatectomy: extending resectability by rapid hypertrophy. Surgery 2015;157:676-689.
46 de Santibañes M, Alvarez FA, Santos FR, Ardiles V, de Santibañes E. The associating liver partition and portal vein ligation for staged hepatectomy approach using only segments I and IV as future liver remnant. J Am Coll Surg 2014;219:e5-9.
47 Vyas SJ, Davies N, Grant L, Imber CJ, Sharma D, Davidson BR, et al. Failure of portal venous embolization. ALPPS as salvage enabling successful resection of bilobar liver metastases. J Gastrointest Cancer 2014;45:233-236.
48 Tschuor Ch, Croome KP, Sergeant G, Cano V, Schadde E, Ardiles V, et al. Salvage parenchymal liver transection for patients with insuff i cient volume increase after portal vein occlusion --an extension of the ALPPS approach. Eur J Surg Oncol 2013;39:1230-1235.
49 Robles Campos R, Parrilla Paricio P, López Conesa A, Brusadín R, López López V, Jimeno Griñó P, et al. A new surgical technique for extended right hepatectomy: tourniquet in the umbilical fi ssure and right portal vein occlusion (ALTPS). Clinical case. Cir Esp 2013;91:633-637.
50 Gall TM, Sodergren MH, Frampton AE, Fan R, Spalding DR, Habib NA, et al. Radio-frequency-assisted liver partition with portal vein ligation (RALPP) for liver regeneration. Ann Surg 2015;261:e45-46.
51 Chen JX, Ran HQ, Sun CQ. Associating microwave ablation and portal vein ligation for staged hepatectomy for the treatment of huge hepatocellular carcinoma with cirrhosis. Ann Surg Treat Res 2016;90:287-291.
52 Boggi U, Napoli N, Kauffmann EF, Presti GL, Moglia A. Laparoscopic microwave liver ablation and portal vein ligation: an alternative approach to the conventional ALPPS procedure in hilar cholangiocarcinoma. Ann Surg Oncol 2016;23:884.
53 Gringeri E, Boetto R, D’Amico FE, Bassi D, Cillo U. Laparoscopic microwave ablation and portal vein ligation for staged hepatectomy (LAPS): a minimally invasive fi rst-step approach. Ann Surg 2015;261:e42-43.
54 Cillo U, Gringeri E, Feltracco P, Bassi D, D’Amico FE, Polacco M, et al. Totally laparoscopic microwave ablation and portal vein ligation for staged hepatectomy: A new minimally invasive two-stage hepatectomy. Ann Surg Oncol 2015;22:2787-2788.
55 Machado MA, Makdissi FF, Surjan RC. Totally laparoscopic ALPPS is feasible and may be worthwhile. Ann Surg 2012;256:e13; author reply e16-19.
56 Xiao L, Li JW, Zheng SG. Totally laparoscopic ALPPS in the treatment of cirrhotic hepatocellular carcinoma. Surg Endosc 2015;29:2800-2801.
57 Conrad C, Shivathirthan N, Camerlo A, Strauss C, Gayet B. Laparoscopic portal vein ligation with in situ liver split for failed portal vein embolization. Ann Surg 2012;256:e14-15; author reply e16-17.
58 Cai X, Peng S, Duan L, Wang Y, Yu H, Li Z. Completely laparoscopic ALPPS using round-the-liver ligation to replace parenchymal transection for a patient with multiple right liver cancers complicated with liver cirrhosis. J Laparoendosc Adv Surg Tech A 2014;24:883-886.
59 Zhang Y, Yang H, Chen Y, Zhu S, Lu T, Jun X. Totally laparoscopic associating liver tourniquet and portal ligation for staged hepatectomy via anterior approach for cirrhotic hepatocellular Carcinoma. J Am Coll Surg 2015;221:e43-48.
60 Vicente E, Quijano Y, Ielpo B, Fabra I. First ALPPS procedure using a total robotic approach. Surg Oncol 2016;25:457.
61 Robles Campos R, Brusadin R, López Conesa A, Parrilla Paricio P. Staged liver resection for perihilar liver tumors using a tourniquet in the umbilical fi ssure and sequential portal vein embolization on the fourth postoperative day (a modif i ed ALTPS). Cir Esp 2014;92:682-686.
62 Hong de F, Zhang YB, Peng SY, Huang DS. Percutaneous microwave ablation liver partition and portal vein embolization for rapid liver regeneration: A minimally invasive fi rst step of ALPPS for hepatocellular carcinoma. Ann Surg 2016;264:e1-2.
63 de Santibañes E, Alvarez FA, Ardiles V, Pekolj J, de Santibañes M. Inverting the ALPPS paradigm by minimizing fi rst stage impact: the Mini-ALPPS technique. Langenbecks Arch Surg 2016;401:557-563.
64 Petrowsky H, Györi G, de Oliveira M, Lesurtel M, Clavien PA. Is partial-ALPPS safer than ALPPS? A single-center experience. Ann Surg 2015;261:e90-92.
65 Linecker M, Kambakamba P, Reiner CS, Linh Nguyen-Kim TD, Stavrou GA, Jenner RM, et al. How much liver needs to be transected in ALPPS? A translational study investigating the concept of less invasiveness. Surgery 2017;161:453-464.
66 Chan AC, Chok K, Dai JW, Lo CM. Impact of split completeness on future liver remnant hypertrophy in associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) in hepatocellular carcinoma: Complete-ALPPS versus partial-ALPPS. Surgery 2017;161:357-364.
67 Shi H, Yang G, Zheng T, Wang J, Li L, Liang Y, et al. A preliminary study of ALPPS procedure in a rat model. Sci Rep 2015;5:17567.
March 22, 2017
Accepted after revision May 12, 2017
Author Aff i liations: Faculty of Medicine, The Chinese University of Hong Kong, Shatin, New Territories, Hong Kong SAR, China (Lau WY and Lai ECH); Department of Surgery, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China (Lai ECH)
Professor Wan Yee Lau, MD, FRCS, FACS, FRACS (Hon), Professor of Surgery, Faculty of Medicine, The Chinese University of Hong Kong, Prince of Wales Hospital, Shatin, New Territories, Hong Kong SAR, China (Tel: +852-2632-2626; Fax: +852-2632-5459; Email: josephlau@cuhk.edu.hk)
© 2017, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(17)60034-1
Published online June 30, 2017.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Indocyanine green fl uoroscopy and liver transplantation: a new technique for the intraoperative assessment of bile duct vascularization
- Effects of multimodal fast-track surgery on liver transplantation outcomes
- Characteristics of recipients with complete immunosuppressant withdrawal after adult liver transplantation
- Predictive value of C-reactive protein/albumin ratio in acute pancreatitis
- Bilioenteric anastomotic stricture in patients with benign and malignant tumors: prevalence, risk factors and treatment
- Interaction between insulin-like growth factor binding protein-related protein 1 and transforming growth factor beta 1 in primary hepatic stellate cells
