MRI诊断孟氏骨折骨间膜损伤范围的研究
2017-08-01连鸿凯谢攀攀马长生朱智肖新广夏玉礼张景义张濛
连鸿凯谢攀攀马长生朱智肖新广夏玉礼张景义张濛
·论著·
MRI诊断孟氏骨折骨间膜损伤范围的研究
连鸿凯1谢攀攀1马长生2朱智1肖新广1夏玉礼2张景义3张濛4
目的探讨新鲜儿童孟氏骨折骨间膜损伤的MRI表现及损伤的范围。方法2014年4月至2016年6月郑州大学附属郑州中心医院和深圳平乐骨伤科医院急诊收治新鲜孟氏骨折患儿36例,术前给予MRI检查,其中男23例,女13例;年龄3~11岁,平均年龄为6.9岁;左侧12例,右侧24例。合并同侧桡骨远端骨骺骨折1例,合并桡神经损伤6例,尺神经损伤1例。BadoⅠ型17例,BadoⅡ型1例,BadoⅢ型18例,BadoⅣ型0例。采用肘关节表面柔顺线圈,患者仰卧、上肢伸直前臂旋后位。分别扫描横轴位、矢状位、冠状位、横轴位获得T1WI、T2WI、T2脂肪抑制图像,扫描层厚为3~5mm,间距为1mm,扫描范围为肘关节至腕关节前臂全长。对比正常儿童前臂骨间膜MRI图像,观察孟氏骨折患儿骨间膜损伤的MRI表现,记录不同程度损伤的距离。结果4例患儿因不能配合MRI检查而未能获得MRI图像,最终获得32例患儿的影像学资料。前臂骨间膜在轴位T1WI、T2WI均可显示,T2脂肪抑制图像显示较为理想,矢状位、冠状位无法分辨骨间膜。以桡骨头环状软骨面为起点,轴位骨间膜距环状软骨面以远30~45mm开始显示。32例患儿均伴有前臂骨间膜损伤,其中25例损伤且伴有断裂,7例骨间膜损伤但无断裂(BadoⅠ型1例,BadoⅢ型6例)。病理改变距离(损伤未断裂+断裂)12~80mm,平均(46.03±18.78)mm;损伤未断裂距离12~56mm,平均(33.09±11.60)mm,断裂距离4~35mm,平均(13.25±9.96)mm。结论MRI可以显示前臂骨间膜损伤,判断损伤程度(损伤未断裂、断裂);孟氏骨折均伴有骨间膜损伤,损伤的程度与上尺桡关节分离的程度具有一定的联系,损伤由上尺桡关节向远端延伸,远端骨间膜可保持完整。
孟氏骨折;核磁共振成像;前臂骨间膜;损伤;上尺桡关节
孟氏骨折是一种特殊类型的骨折,即尺骨骨折或尺桡骨双骨折合并桡骨头脱位[1],临床治疗极具挑战性。前臂作为一个整体功能单位,尺桡骨、上下尺桡关节、肌肉、韧带、骨间膜共同维系着前臂复杂运动,治疗上提倡重视前臂解剖结构特点,强调个体化治疗,并依据骨折类型,软组织损伤情况为治疗方式选择提供线索。前臂或肘关节损伤常伴随骨间膜损伤,骨间膜损伤能够一定程度上影响前臂纵向、横向稳定性[2],因此研究骨间膜损伤情况,能够为前臂损伤诊疗提供新的思路。然而以往对孟氏骨折伴随的骨间膜损伤重视不够,认识不足,相关文献报道较少。为研究前臂骨间膜解剖和孟氏骨折骨间膜损伤情况,本院收治的符合纳入及排除标准的36例新鲜孟氏骨折患儿术前行前臂MRI检查,观察骨间膜病理改变,探讨孟氏骨折前臂骨间膜损伤程度,现总结分析如下。
资料与方法
一、一般资料
本研究共纳入患者36例,其中男23例,女13例;年龄3~11岁,平均年龄为6.9岁;左侧12例,右侧24例。合并同侧桡骨远端骨骺骨折1例,合并桡神经损伤6例,尺神经损伤1例。BadoⅠ型17例,BadoⅡ型1例,BadoⅢ型18例,BadoⅣ型0例。所有患儿均为闭合性损伤,均为1周内的新鲜损伤,受伤至入院治疗的时间为1~168h,平均时间为23.6h。患者一般情况见表1。
二、纳入及排除标准
纳入标准:①符合孟氏骨折诊断标准的患者;②年龄﹤14岁;③受伤时间﹤3周;④首诊患者,未在其他医院接受治疗。
排除标准:①开放性骨折患者;②前臂骨筋膜室综合征需急诊手术者;③有MRI检查禁忌证者;④合并有心脑血管、肝、肾和造血系统等严重原发疾病及精神病患者。
三、MRI设备和检查方法
术前给予前臂MRI检查,与患者家属沟通并签署MRI检查安全知情同意书。采用1.5T超导型MRI扫描机,肘关节表面柔顺线圈,检查体位为患者仰卧、上肢伸直前臂旋后位。主要采取横轴面扫描,获得T1WI、T2WI、T2脂肪抑制像,扫描层厚为3~5mm,层间距为1mm,扫描范围为肘关节至腕关节前臂全长。
四、观察指标
依据正常骨间膜与不同损伤程度骨间膜MRI轴位图像表现,将骨间膜定义如下[3]:①骨间膜完整:连接尺桡骨间均匀、连续不间断低信号带,周围不伴有水肿或出血高信号表现(图1~2);②骨间膜损伤:尺桡骨间低信号带连续性尚存,但迂曲且周围伴有水肿、出血高信号表现(图3~4);③骨间膜断裂:尺桡骨间连续性低信号带被水肿、出血高信号截断,组织完整性丧失(图5~6)。依据骨间膜损伤程度评价标准,记录骨间膜损伤未断裂和断裂的范围(轴位骨间膜病理改变层数)。图像分析由经验丰富的影像学中级职称以上的2位医师进行,有争议的病灶由二人协商解决。
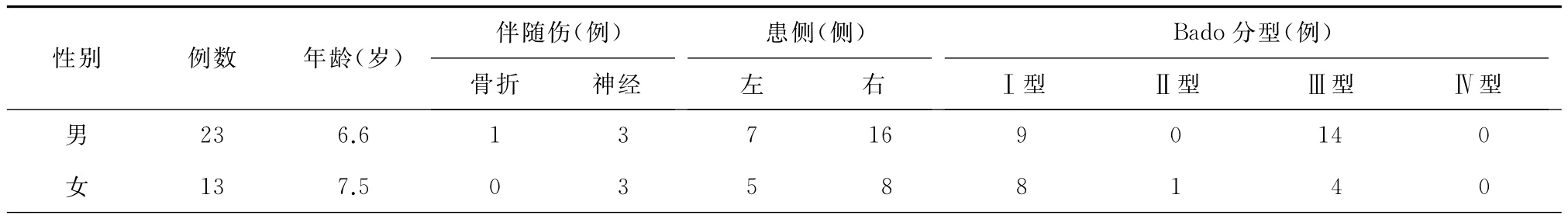
表1 36例患者的一般资料
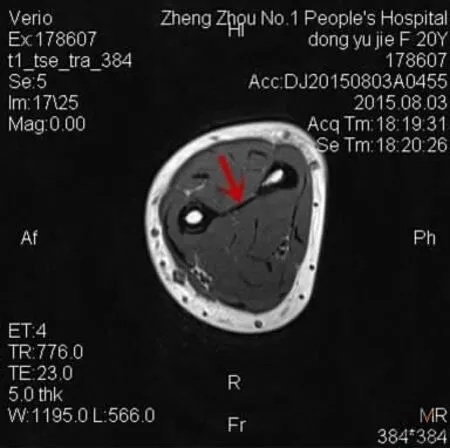
图1 骨间膜完整(T1WI图像,为轴位扫描第17层),尺桡骨间连续不间断低信号带,周围不伴有水肿或出血高信号表现(如箭头所指)

图2 骨间膜完整(T2脂肪抑制图像,为轴位扫描第20层),尺桡骨间连续不间断低信号带,周围不伴有水肿或出血高信号表现(如箭头所指)
结 果
4例患者因不能配合MRI检查而未能获得MRI图像,其中BadoⅠ型1例,BadoⅢ型3例,共获得32例患者的影像学资料。MRI矢状位、冠状位无法分辨骨间膜,轴位能够显示骨间膜。正常骨间膜图像,距离环状软骨面以远30~45mm开始显示,为尺桡骨间连续线状低密度影,周围不伴出血、水肿高信号,脂肪抑制序列可消除脂肪信号干扰更为清晰显示。给予健康人前臂MRI检查,观察正常骨间膜轴位MRI图像(扫描体位:上肢伸直前臂旋后位,扫描层厚为5mm,扫描层数25层)。如图1所示为T1WI图像,为轴位扫描第17层。如图2所示为T2脂肪抑制图像,为轴位扫描第20层。均为完整骨间膜,表现为连接尺桡骨间均匀、连续不间断低信号带,周围不伴有水肿或出血高信号表现。32例患儿均伴有前臂骨间膜损伤,骨间膜损伤表现为尺桡骨间线状低密度带迂曲但连续性尚存,骨间膜周围伴有出血、水肿高信号,此为外力载荷引起骨间膜部分纤维撕裂但尚未断裂,完整性尚存,损伤距离12~56mm,平均(33.09±11.60)mm。给予1例伤后24h内入院的患儿X线检查(图7~8),诊断为孟氏骨折(BadoⅠ型),同时行前臂MRI检查(扫描体位:上肢伸直前臂旋后位,轴位扫描层厚为5mm,扫描层数24层)。32例患者中25例损伤且伴有断裂,骨间膜断裂表现为尺桡骨间连续性低信号带被高信号截断,连续性中断,骨间膜弹弹性回缩,断裂距离4~35mm,平均(13.25±9.96)mm,32例患者中7例骨间膜有损伤但无断裂(BadoⅠ型1例,BadoⅢ型6例)。病理改变距离(损伤+断裂)12~80mm,平均(46.03±18.78)mm。骨间膜损伤或断裂是由于上尺桡关节分离和尺骨力线改变超过了骨间膜力学强度。

图3 骨间膜损伤(患儿轴位扫描第13层),尺桡骨间低信号带连续性尚存,但迂曲且周围伴有水肿、出血高信号(如箭头所指)

图4 骨间膜损伤(患儿轴位扫描第14层),尺桡骨间低信号带连续性尚存,但迂曲且周围伴有水肿、出血高信号(如箭头所指)

图5 骨间膜断裂(患儿轴位扫描第17层),尺桡骨间连续性低信号带被高信号截断,连续性中断,骨间膜弹性回缩(如箭头所指)
讨 论
基于儿童骨骼生理特点和孟氏骨折损伤特点,目前临床上孟氏骨折诊疗重点放在以下两个方面:一是恢复尺骨生物力线,尺骨力线的恢复有助于桡骨小头的回纳,同时减少桡骨小头再脱位的可能;二是理解孟氏骨折环状韧带和肘关节周围韧带损伤情况及其在桡骨小头复位时的影响。作者认为在重视以上两个方面的同时,应该考虑到骨间膜在整个前臂运动中的功能,理解骨间膜在保持前臂稳定中的作用,把握骨间膜损伤在影响治疗方式选择中的作用。只有对孟氏骨折伴随的骨间膜损伤情况有所了解,才能对不同损伤类型有深入认识,治疗中有的放矢,制定出个体化治疗方案。本次研究在国内外首次利用MRI影像学技术,观察了新鲜儿童孟氏骨折伴随的骨间膜损伤情况,揭示了新鲜儿童孟氏骨折骨间膜病理改变。
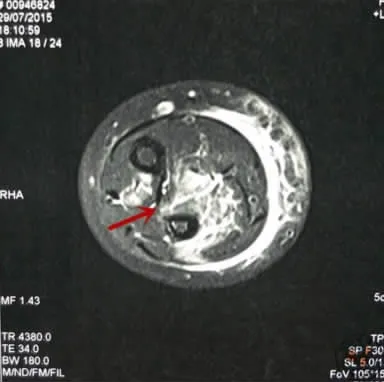
图6 骨间膜断裂(患儿轴位扫描第18层),尺桡骨间连续性低信号带被高信号截断,连续性中断,骨间膜弹性回缩(如箭头所指)

图7 患儿伤后X线正位片,右孟氏骨折(BadoⅠ型)

图8 患儿伤后X线侧位片,右孟氏骨折(BadoⅠ型)
一、骨间膜解剖和生物力学特性
骨间膜为尺桡骨之间斜向走行的膜性结构,一般认为由3部分组成:中央腱性部分、两端的膜性部分以及背侧斜索。膜性部分薄且柔软,腱性部分及背侧斜索厚且坚韧,可以称之为骨间韧带。骨间膜随前臂旋转而形态变化,紧张或松驰程度不同,中立位时伸展紧张,旋前时向背侧弯曲,旋后时向掌侧弯曲[4],更好地使前臂应力均匀地分布在尺桡骨之间,减少肱桡关节应力,保护肱桡关节[5]。研究表明正常情况下,桡骨头在维持前臂稳定和承担轴向载荷中起到基础作用,骨间膜和三角纤维软骨起到次要作用,当桡骨头脱位或切除后,骨间膜和三角纤维软骨则起到主要作用[6]。Anderson等[7]研究发现,在横向位移载荷下,骨间膜中央腱部、两端膜部、环状韧带对稳定桡骨同样重要,但是在前臂旋转过程中,中央腱部能够更好保持桡骨小头的稳定。Trousdale等[8]认为骨间膜损伤的情况一定程度上可反应上尺桡关节损伤的情况。作者认为前臂有大体相互平行的尺桡骨组成基本构架,两端有相互约束的上下尺桡关节,中间有骨间膜维系,这是一个相对稳定的功能体系,前臂旋转功能的正常,需要尺桡骨与肘腕关节维持正常解剖对位,维持力线,也需要骨间膜、上下尺桡关节周围韧带维持。
二、骨间膜损伤MRI表现
前臂骨间膜损伤常伴随前臂骨折而出现,以往对前臂骨间膜的解剖和生物力学功能,损伤后的诊断和治疗认识不足,后期患者多出现腕关节疼痛、前臂旋转受限及肘关节活动障碍等并发症。近年来随着对前臂骨间膜生理、病理解剖研究的深入,超声、MRI技术的应用,提高了对骨间膜的认识。目前评估和诊断前臂骨间膜损伤的方法主要有桡骨拉伸试验[9],超声检查以及MRI检查。相较于桡骨拉伸试验局限于术中,超声检查受困于医师的经验,MRI技术是观察骨间膜结构最有效的非创伤性方法,对骨间膜损伤的阳性预测值为100%,阴性预测值为89%,敏 感 性 为 87.5%,特 异 性 为 100%[10]。Rodriguez-Martin等[11]研究发现轴向 T1和 T2加权图像能够清晰显示健康志愿者的前臂骨间膜,脂肪抑制技术更清楚地确定水肿和出血区域。骨间膜由于其线性附着和平面结构,矢状位、冠状位无法显示骨间膜结构,轴位可以较好显示。骨间膜轴位MRI图像以桡骨头环状软骨面为起点,距离环状软骨面以远30~45mm开始显示,骨间膜很薄且周围有肌间脂肪、血管信号的干扰,因此一般脂肪抑制图像能够更好的显示骨间膜结构和病理改变,但要注意肌肉软组织损伤信号改变给骨间膜损伤信号改变带来的干扰。通过研究前臂骨间膜病理改变有两种形式:损伤和断裂。损伤为骨间膜部分纤维断裂,但仍具有连续性断裂为低信号线状影被高信号影截断,连续性中断。孟氏骨折一般均伴有骨间膜损伤,但不都伴有断裂,有时损伤和断裂并存。与本研究结果是一致的,32例患儿均伴有前臂骨间膜损伤,其中25例损伤且伴有断裂,7例骨间膜损伤但无断裂(BadoⅠ型1例,BadoⅢ型6例)。病理改变距离(损伤未断裂+断裂)12~80mm,平均(46.03±18.78)mm;损伤未断裂距离12~56mm,平均(33.09±11.60)mm,断裂距离4~35mm,平均(13.25±9.96)mm。
三、骨间膜与上尺桡关节分离程度的关系
上尺桡关节为车轴关节,由肘关节囊、环状韧带和骨间膜3个因素共同维持[12]。骨间膜一定程度上能够限制桡骨外移,防止肱桡关节脱位。通过MRI检查发现骨间膜损伤层面由上尺桡关节向远端延伸,远端骨间膜可保持完整,同时有这样一种趋势:上尺桡关节分离距离较小者,前臂骨间膜多为小范围病理改变,损伤未断裂或断裂层面较少。随着上尺桡关节分离距离的增加,前臂骨间膜多出现大范围病理改变,损伤或断裂层数增多,但由于上尺桡关节分离尚缺乏明确的测量标准,两者是否存在线性相关,尚未明确。作者认为基于前臂骨间膜解剖应力特点,在前臂稳定和维持前臂旋转功能中的重要作用,上尺桡关节分离程度与骨间膜损伤程度反映了暴力大小,都是由外来暴力大小决定的,作为损伤的结果并存。结构决定功能,功能强化结构,上尺桡关节分离程度一定程度上反映了骨间膜损伤的程度,若两者存在的线性关系,是否考虑借鉴上尺桡关节分离程度对骨间膜损伤程度做出诊断,进而指导临床治疗值得思考。
孟氏骨折均伴有前臂骨间膜损伤,MRI检查能够很好的观察骨间膜结构,显示骨间膜损伤造成的出血、水肿,判断骨间膜病理改变的类型:损伤或断裂,是诊断骨间膜损伤非常有效的非创伤性方法。明确骨间膜损伤及损伤程度的诊断,能够更好的了解前臂损伤的机制,为治疗和预后提供理论依据,但不同类型的骨间膜损伤及其损伤程度在影响治疗方式选择中起到何种作用,仍需要继续深入的研究。
[1]Rehim SA,Maynard MA,Sebastin SJ,et al.Monteggia fracture dislocations:a historical review [J].J Hand Surg Am,2014,39(7):1384-1394.
[2]Green JB,Zelouf DS.Forearm instability [J].J Hand Surg Am,2009,34(5):953-961.
[3]杨胜松,王满宜.MRI诊断Maisonneuve骨折骨间膜断裂范围的研究 [J].中华放射学杂志,2000,34(6):389-392.
[4]McGinley JC,Kozin SH.Interosseous membrane anatomy and functional mechanics[J].Clin Orthop Relat Res,2001,(383):108-122.
[5]Shepard MF,Markolf KL,Dunbar AM.Effects of radial head excision and distal radial shortening on load-sharing in cadaver forearms[J].J Bone Joint Surg Am,2001,83(1):92-100.
[6]Skahen JR 3rd,Palmer AK,Werner FW,et al.Reconstruction of the interosseous membrane of the forearm in cadavers[J].J Hand Surg Am,1997,22(6):986-994.
[7]Anderson A,Werner FW,Tucci ER,et al.Role of the interosseous membrane and annular ligament in stabilizing the proximal radial head[J].J Shoulder Elbow Surg,2015,24(12):1926-1933.
[8]Trousdale RT,Amadio PC,Cooney WP,et al.Radio-ulnar dissociation.A review of twenty cases[J].J Bone Joint Surg Am,1992,74(10):1486-1497.
[9]Smith AM,Urbanosky LR,Castle JA,et al.Radius pull test:predictor of longitudinal forearm instability[J].J Bone Joint Surg Am,2002,84(11):1970-1976.
[10]Mcginley JC,Roach N, Hopgood BC,et al.Forearm interosseous membrane trauma:MRI diagnostic criteria and injury patterns[J].Skeletal Radiol,2006,35(5):275-281.
[11]Rodriguez-Martin J,Pretell-Mazzini J.The role of ultrasound and magnetic resonance imaging in the evaluation of the forearm interosseous membrane.A review [J].Skeletal Radiol,2011,40(12):1515-1522.
[12]Abdelgawad AA,Hussain A,Ebraheim NA.Screw fixation of the radial head:radiological assessment of the proximal radio-ulnar joint and average radial head diameter-an anatomic study[J].Arch Orthop Trauma Surg,2010,130(4):465-467.
Study on MRI diagnosis of interosseous membrane damage range of Monteggia fractures
Lian Hongkai1,Xie Panpan1,Ma Changsheng2,Zhu Zhi1,Xiao Xinguang1,Xia Yuli2,Zhang Jingyi3,Zhang Meng4.1Department of Orthopedics,Zhengzhou Central Hospital Affliated to Zhengzhou University,Zhengzhou 450007,China;2Department of Pediatric Orthopaedic,Shenzheng Pingle Orthopedics Hospital,Shenzheng 518010,China;3Department of Orthopedics,Zhengzhou Orthopedics Hospital,Zhengzhou 450052,China;4Department of Orthopedics,the Medical Group of Zhengzhou First People′s Hospital,Zhengzhou 450004,China
Xie Panpan,Email:shangqiuxiepan@126.com
BackgroundMonteggia fracture is a special type of fractures,namely,the ulnar fracture or the radial and ulnar fractures associated with radial head dislocation,and the treatment is extremely challenging in the clinical practice.As a whole functional unit,the complex movement of forearm is maintained by radius and ulna,proximal and distal radioulnar joints,muscles,tendons and interosseous membrane(IOM).Therapeutically,the anatomic characteristics of forearm were valued and the individual treatment of was emphasized.The treatment options were based on the fracture classification and the soft tissue damage degree.IOM damage is often combined in forearm or elbow joint injuries,which can affect the vertical and transverse instability to some extent.Therefore,theresearch of IOM damage provides new ideas for the diagnosis and treatment of forearm injuries.Formerly,with few reported literatures we did not attach importance to the damage and lack the recognition.To study the anatomy of forearm IOM and its damage after Monteggia fracture,36 children of Monteggia fractures were hospitalized to undergo the MRI examinations according to the inclusive and exclusive criteria,observe the pathologic changes and explore the MRI appearance and damage degrees.Methods(1)General information:This study was made up of 36children,including 23males and 13females.The ages ranged from 3to 11years with 6.9years on average.12cases were left side and 24cases were right side.1case was combined with ipsilateral distal radial epiphyseal fracture,6cases were combined with radial nerve injuries and 1case was combined with ulnar nerve injuries.17cases were type BadoⅠ,1case was type BadoⅡ,18cases were type BadoⅢand no cases were type BadoⅣ.All the children had fresh closed injuries within one week and the time from injury to hospitalization ranged from 1to 168hours with 23.6hours on average.(2)Inclusive and exclusive criteria.Inclusive criteria:①Children who fitted for the diagnostic criteria of Monteggia fracture;②Age <14years;③Time after injury <3weeks;④First-visit outpatients without receiving treatment in other hospitals.Exclusive criteria:①Open fracture;②Patients who had forearm osteofascial compartment syndrome and needed emergency surgery;③Contraindications of MRI examination;④Children combined with cardiovascular,cerebrovascular, hepatic,renal or hematopoietic system primary diseases or psychotic patients.(3)MRI equipment and examination method.After communication with the children′s family members,the informed consents were signed to permit the conduction of preoperative MRI examinations.The superconduct magnetic resonance imaging system of 1.5Twas applied with soft coil on the surface of elbow joint.The children were in supine position with upper extremities extension and forearms supination.The axial scans were applied to obtain the images of T1WI,T2WI and T2WI/SPIR.The slice thickness of scanning was 3-5mm with 1mm of interlayer spacing,and the scanning range was forearm of full length from elbow to wrist.(4)Observed indicators.According to the MRI axial images of normal IOM and IOM of different damage degrees,the definitions were as follows:①IOM integrity:The homogeneous and continuous hypointense bands connected radius and ulna without;②IOM damage:The continuous hypointense bands between radius and ulna still exited but had high signals of edema and hemorrhage;③IOM rupture:The hypointense bands were ruptured by high signals of edema or hemorrhage with tissue integrity loss.According to the evaluation standards of IOM damage degree,the range of non-ruptured and ruptured IOM (axial layers of IOM pathological changes).The image analysis was conducted by two radiologists of intermediate grade or above,and the controversial focuses were negotiated and settled cooperatively between them.ResultsFour patients could not cooperate with MRI examinations and thus failed to get the MRI images,including 1case of type BadoⅠ,3cases of type BadoⅢ,and the imaging data of 32cases were obtained in total.The IOM could be distinguished in the axil images instead of sagittal or coronal images.In the images of normal IOM,the continuous linear hypointense signals between radius and ulna started 30-45mm distal to cricoidcartilage surface without hyperintense signals hemorrhage or edema around.The lipoma signal interference was eliminated by STIR for clearer display.Healthy people were taken as control and conducted forearm MRI to observe the normal MRI axial images of IOM (scanning position:upper extremity extension with forearm supination;5mm of scanning slice thickness and 25scanning layers).32children were combined with forearm IOM damage and the manifestations were presented as circuitous but continuous linear hypointense signals between radius and ulna with hyperintense signals of hemorrhage and edema around.This was partial IOM fiber laceration instead of rupture with remaining integrity,which resulted from external force loads.The damage distance was 12-56mm with (33.09±11.60)mm on average.25children were combined with IOM ruptures and the manifestations were presented as hypointense signals interception by hyperintense signals between radius and ulna,continuity interruption and IOM elastic retraction.The rupture distance was 4-35mm with (13.25±9.96)mm on average.7cases had damaged but not ruptured IOM (1case of type BadoⅠand 6cases of type BadoⅢ).The distance of pathologic change(damage and rupture)was 12-80mm with(46.03±18.78)mm on average.The strength produced by the separation of proximal radioulnar joint and the change of force lines was larger than the mechanical strength of IOM,which led to damages or ruptures.Conclusions The forearm IOM injuries are combined in all the Monteggia fractures.MRI are applied to well observe the structures of IOM,reveal hemorrhage and edema caused by the injury and determine whether the type of pathological changes is damage or rupture,which is a very effective noninvasive method in the treatment of IOM injuries.To clarify diagnosis and damage degree is to better understand the mechanism of forearm injury and provide theoretical basis for treatment and prognosis.However,the role of different injuries and damage degrees in the treatment options of IOM requires further research.
Monteggia fracture;Magnetic resonance imaging;Interosseous membrane of forearm;Injury;Upper ulnar joint
2016-09-28)
(本文编辑:胡桂英;英文编辑:陈建海、张晓萌、张立佳)
10.3877/cma.j.issn.2095-5790.2017.01.004
河南省科技攻关计划项目(102102310430)
450007 郑州大学附属郑州中心医院骨科1;518010 深圳平乐骨伤科医院小儿骨科2;450052 郑州市骨科医院骨病科3;450004 郑州市第一人民医院骨科4
谢攀攀,Email:shangqiuxiepan@126.com
连鸿凯,谢攀攀,马长生,等.MRI诊断孟氏骨折骨间膜损伤范围的研究 [J/CD].中华肩肘外科电子杂志,2017,5(1):15-21.
