后侧微创入路结合三角固定原则治疗肩胛体及肩胛颈骨折
2017-08-01李仁斌林焱斌熊圣仁庄研熊国胜张怡元
李仁斌 林焱斌 熊圣仁 庄研 熊国胜 张怡元
·论著·
后侧微创入路结合三角固定原则治疗肩胛体及肩胛颈骨折
李仁斌 林焱斌 熊圣仁 庄研 熊国胜 张怡元
目的探讨后侧微创入路结合三角固定原则治疗肩胛体及肩胛颈骨折的临床疗效。方法自2012年6月至2014年12月,厦门大学附属福州第二医院采用后侧微创入路钢板内固定治疗肩胛体及肩胛颈骨折患者23例,其中男16例,女7例,平均年龄37.58岁(19~62岁)。合并损伤主要包括:多发肋骨骨折9例,血气胸和(或)肺挫伤6例,颅脑损伤5例,颈椎损伤2例,同侧锁骨骨折4例,骨盆骨折4例。采用臂、肩、手功能障碍(disabilities of the arm,shoulder and hand,DASH)评分对患者肩关节功能进行评估。结果所有患者均获得完整随访,平均随访时间17.7个月(9~36个月)。手术时间78.6min(58~121min),出血量68.3ml(50~100ml)。所有骨折均愈合,无感染、无肩关节创伤性关节炎、无异位骨化、无神经损伤等并发症。DASH评分平均为7.8分(4~21分)。结论后侧微创入路结合三角固定原则治疗肩胛体及肩胛颈骨折具有切口小、出血少、对软组织干扰小、手术时间短、手术效果好等优点。
微创;三角固定;肩胛骨;骨折;内固定
临床上肩胛骨骨折比较少见,约占全身骨折的0.5%~1.0%,98%的肩胛骨骨折可累及肩胛体及肩胛颈。一般认为,盂极角小于22°,肩胛体骨折横向移位和短缩移位超过3cm,骨折成角大于40°的肩胛体及肩胛颈骨折需要手术,78.1%的肩胛骨骨折可通过后侧入路进行手术治疗[1]。最经典的后侧入路是Judet切口,通过这个切口显露肩胛骨,需要很大的皮肤切口,需要切断冈下肌、小圆肌和三角肌后束;另一种是改良Judet入路,这一入路的皮肤切口和传统的Judet切口一样,只是显露皮瓣后,经过冈下肌和小圆肌间隙显露肩胛骨。Judet入路可广泛显露,完全显露肩胛骨后侧部分,但是需要一个大的皮肤切口和广泛的肌肉剥离。而且,大的肌瓣阻碍了对后侧肩胛盂的显露,可能对肩胛上神经的牵拉而导致损伤。改良Judet入路最大的一个缺点就是很大的皮瓣术后产生血肿,它最大的优点是相对于Judet入路有更小的肌肉剥离、更好的显露和固定后侧肩胛盂骨折避免了对肩胛上神经的牵拉[2]。2011年美国学者Gauger等[3]利用后侧微创入路治疗7例肩胛体及肩胛颈骨折患者,并取得了良好的疗效,但是并没有对内固定的原则进行阐述。肩胛骨是一个类似三角形的扁骨,3个边分别为肩胛冈与肩胛体连接部、内侧缘及外侧缘;3个角分别是内上角、下角及关节盂颈部。按肩胛体及肩胛颈骨折的手术适应证,骨折往往累及了2个边甚至3个边。为了重建一个稳定的三角形,提出了三角固定原则,即骨折所累及的每一个边都需固定,肩胛骨上附着18块肌肉。作者认为,一个稳定的肩胛骨有利于术后的早期功能锻炼。按这样的固定原则治疗了一组病例,取得了良好的临床疗效。
资料与方法
一、一般资料
自2012年6月至2014年12月,本院采用后侧微创入路钢板内固定治疗肩胛体及肩胛颈骨折患者23例,其中男16例,女7例,平均年龄37.58岁(19~62岁)。合并损伤主要包括:多发肋骨骨折9例,血气胸和(或)肺挫伤6例,颅脑损伤5例,颈椎损伤2例,同侧锁骨骨折4例,骨盆骨折4例。根据Hardegger的骨折分型标准[4],本组患者肩胛体骨折18例;肩胛颈骨折5例,其中外科颈骨折3例,经肩胛冈骨折2例。受伤至手术的时间平均为7.8d(5~16d)。所有患者术前均接受肩关节创伤系列片投照及肩关节CT扫描三维重建。本组患者骨折的类型均适合通过后侧入路及有切开复位钢板内固定的指征;均在伤后4周内接受手术治疗;均无前侧肩胛盂骨折、喙突骨折、肩峰骨折;外侧柱、肩胛冈、内侧缘均不存在多个骨折块。
二、手术方法
全身麻醉,采取俯卧位,根据骨折类型选择切口,见图1。选择切口的原则是:累及外侧缘的骨折选择A或B切口,累及内侧缘的骨折选择C或D切口,累及上缘的骨折选择E切口。选择A或B切口切开皮肤后可沿冈下肌、小圆肌间隙显露骨折端,选择C或D切口时于肩胛骨内侧缘行纵形皮肤切口,于肩胛骨内侧缘显露骨折端,对于上缘骨折可选择E切口。切口大小在3~5cm,因此内固定钢板不宜选择重建板,因为太长的钢板不可能通过这么小的切口放置。本组患者均选用2.7mm动力加压钢板或重建板钢板,内缘可选择2.4mm的锁定钢板。选择A切口,可不需要切断三角肌后束,在牵拉冈下肌时应特别注意,不要损伤肩胛上神经,还应注意对旋肩胛动脉升支的处理,旋肩胛动脉位于肩胛骨外侧缘与肩胛盂下缘5~6cm处[5]。在肩胛骨内侧角,大多数骨折端位于内侧角,分离筋膜和骨膜沿着肩胛骨脊柱缘。骨膜下剥离游离冈下肌,直到可看见骨折端及复位和固定。首先固定外侧缘,因为外侧钢板不要预弯,内侧钢板往往需要预弯。此外,外侧缘的固定方便内侧缘骨折复位和固定。上缘的骨折可沿着肩胛冈做切口,对冈下肌做钝性分离,在肩胛切迹处要小心保护肩胛上神经及动静脉(图2~7)。
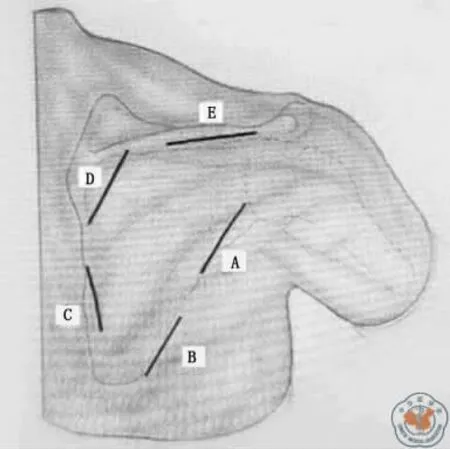
图1 根据骨折位置的不同,可分别选取切口

图2 患者男性,43岁,术前三维CT提示肩胛体骨折,肩胛骨正位上提示骨折移位>25mm,盂极角20°

图3 术前三维CT肩胛骨侧位片提示骨折端成角超过40°

图4 术中外侧缘切口5cm

图5 术中内侧缘切口3cm
三、术后处理
术后均不放置引流片,术后第2天开始钟摆样运动以及被动前屈、外旋锻炼。此后可逐渐增加被动内旋、内收及外展练习。随访期间依患者影像学检查骨折愈合情况逐渐过度为主动活动锻炼。12周后开始力量锻炼并加强各方向的练习。

图6 术后三维CT肩胛骨正位片提示钢板位置正确,盂极角正常骨折复位良好
结 果
所有患者均获完整随访,平均随访时间17.7个月(9~36 个月)。手术 时 间平均78.6min(58~121min),出血量平均68.3ml(50~100ml)。所有患者术中未发生并发症,未见伤口感染、愈合不良,均达Ⅰ/甲愈合。骨折复位良好,术后未出现骨折再移位、骨折畸形愈合或不愈合,平均愈合时间为2.5个月(2~3个月)。所有病例随访期间均未见螺钉松动、退出及断裂情况。术后患者上肢前举平均162°(150~180°),外展平均110°(90~120°),体侧外旋平均54°(45~60°),DASH 评分平均为7.8分(4~21分)。
讨 论

图7 术后三维CT肩胛骨侧位片提示钢板位置正确,骨折复位良好,成角纠正
四、术后随访及评价指标
所有患者术后半年内每个月门诊复查1次,半年后每3个月门诊复查1次,1年后每6个月门诊复查1次。术后X线检查包括前后位肩关节正位片、Y位片。所有患者都进行问卷调查。2名医师独立评估所有术后放射片,决定是否发生骨不连或畸形愈合。骨折畸形愈合的标准是:正位片上、Y位片上移位超过0.5cm,Y位片上成角超过10°和对侧相比盂极角相差10°以上。将每位患者末次随访的臂、肩、手功能障碍(disabilities of the arm,shoulder and hand,DASH)评分作为最后功能评价指标。
一、微创入路的适应证及其禁忌证
肩胛骨骨折通过影像学可精确判断肩胛骨骨折类型,文献报道62%~98%的肩胛骨骨折都累及到肩胛体或肩胛颈,后侧入路是最常用的入路[6]。临床常用的后侧入路有Judet入路和改良Judet入路。这两种入路均存在各自的优缺点。Judet入路的优点是可广泛的显露后侧结构,对于复杂的肩胛骨骨折仍然是必选入路,但存在出血多、肩胛上神经牵拉伤的风险。改良Judet入路利用Judet入路的皮肤切口,通过小圆肌、冈下肌间隙进行外侧骨折复位和固定,通过内侧分离冈下肌对内侧骨折端的复位和固定。改良Judet入路存在切口大、对于复杂的肩胛骨骨折显露不充分等缺点,优点是出血少、对肌肉的干扰小。但对于相对简单的肩胛体及肩胛颈骨折,根据本研究结果,可通过微创入路来治疗,且得到了良好的临床效果。作者认为后侧的微创入路只适用于相对简单的肩胛体及肩胛颈骨折,且不需要很长的钢板就能固定骨折端,因为太长的钢板不可能通过小切口放置。如果同时伴有喙突骨折或前方、上方关节盂骨折就不适应用该切口,如果外侧柱、肩胛冈、内侧缘存在多个骨折块也不适合该切口。骨折超过4周由于骨折端复位困难,可能需要广泛显露骨折端来复位,因此也不适合应用该切口。
二、微创入路治疗肩胛体及肩胛颈骨折的优点及注意事项
微创入路有以下几个优点:第一,这些有限的切口减少了皮瓣和后侧肩胛骨肌肉的剥离,术中有效结扎旋肩胛动脉后,有效保护肩胛上动静脉,可明显减少术中的出血量,有利于术后的康复;第二,微创入路允许充分的直视下复位骨折端,不需要显露位于肩胛体的多数骨折线,多个微创入路的组合使用,可重建肩胛骨的3个边,使肩胛骨达到稳定,有利于术后早期功能锻炼,不需要广泛显露肩胛体的其他骨折线;第三,切口小,更加美观。但是使用该入路时必需严格遵循适应证,在术中应充分了解旋肩胛动脉的走行及肩胛上动静脉的解剖特点,以免术中损伤这些组织。Wijdicks等[7]通过解剖学的研究提出了4-7-8三角的危险区,即肩胛切迹到旋肩胛动脉的距离约为7cm,到肩胛上神经最内分支的距离约为4cm,其围成的一个三角区域为损伤上述组织的危险区域。一个简单实用判断旋肩胛动脉的方法是,术中明确三角肌后束与冈下肌外缘相交处,旋肩胛动脉往往就在此处贴着肩胛骨走行。术中显露旋肩胛动脉后,可对其进行结扎,结扎后并不会破坏肩胛骨的血供。在骨膜下分离肩胛骨,连同冈下肌一起拉向内侧,一般可以很好的显露肩胛盂的后侧而不会损伤肩胛上神经及动静脉,如果只是处理外侧缘的骨折,三角肌后束是没必要切断的。术中对难复性外侧缘骨折的复位可通过单钩来协助完成。一般来说对外侧缘及上缘骨折的固定不需要预弯钢板,因此往往先固定外侧缘,然后是上缘,最后再固定内侧缘,因为内侧缘骨折大多位于内上角,需要预弯钢板,外侧缘或上缘固定好后有利于对内侧缘的固定。由于肋骨的阻挡,术中透视并不能看清肩胛骨的全貌,往往只能看清肩胛骨的外侧部分,因此术中评判骨折复位情况可通过盂极角,在肩胛骨正位片上,正常成人的盂极角正常值为30~40°[8]。通过摆放球管拍摄Y位片,可判断骨折端成角情况。
三、三角固定原则的理论依据与临床结果
肩胛骨是薄片状,呈不规则的三角状,主要作用是提供肌肉的附着区。肩胛骨的上角、下角和外缘增厚,给更有力的肌肉提供附着区。有斜方肌止于肩胛冈和肩峰,其可用于外侧角的抬升。大小菱形肌止于肩胛骨的内侧缘,主要作用为内收肩胛骨。肩胛提肌止于肩胛骨上角,主要作用为上提上角;前锯肌止于肩胛骨胸廓面的内侧缘从上角一直到下角,肩胛提肌和前锯肌一起使肩胛骨产生向上旋转力,冈上窝是冈上肌的起点,冈下窝是冈下肌的起点,肩胛骨前侧窝是肩胛下肌的起点,小圆肌起至肩胛骨外侧缘中下部,大圆肌起自于肩胛骨后表面肩胛骨下部分的外侧边缘,喙突是肱二头肌短头和喙肱肌的起点,也是胸小肌的止点。肩胛冈、肩峰是三角肌的起点,肩胛盂上下极各有一个骨性结节,盂上结节是肱二头肌长头腱的起点,盂下结节是肱三头肌长头腱的起点。由此看出,除了肩胛下肌、冈上肌、冈下肌起点占据肩胛骨的大部分位置,其他肌肉的止点均位于边或角上。这些肌肉组织相互配合,既有协同肌,又有拮抗肌,共同完成肩胛骨的旋转运动、前后倾运动。肩胛骨的运动并非是直线运动,而是旋转运动,因此当骨的连续性中断,必然会导致肌肉群的作用发生紊乱,从而导致骨折的畸形愈合,严重畸形愈合必然导致功能上的缺失[9]。根据三角形力学稳定的原理,至少固定其中的两边,才能恢复和维持该三角形结构的稳定性[10],因此提出三角固定原则来治疗肩胛体或肩胛颈骨折,就是重建三角形的稳定性,恢复肌肉群相互协同、相互拮抗,从而避免骨折的畸形愈合或内固定无失败。从本组病例的临床结果来看,无畸形愈合、无内固定失败,且功能恢复满意。因此作者认为,后侧微创入路结合三角固定原则治疗肩胛体及肩胛颈骨折具有切口小、出血少、对软组织干扰小、手术时间短、手术效果好等临床优点,值得临床推广。
[1]Cole PA,Dubin JR,Freeman G.Operative techniques in the management of scapular fractures [J].Orthop Clin North Am,2013,44(3):331-343.
[2]Cole PA,Gauger EM,Schroder LK.Management of scapular fractures[J].J Am Acad Orthop Surg,2012,20(3):130-141.
[3]Gauger EM,Cole PA.Surgical technique:a minimally invasive approach to scapula neck and body fractures[J].Clin Orthop Relat Res,2011,469(12):3390-3399.
[4]Hardegger H,Simpson A, Weber G.The operative treatment of scapular fractures[J].J Bone Joint Surg Br,1984,66(5):725-731.
[5]Pizanis A,Tosounidis G,Braun C,et al.The posterior twoportal approach for reconstruction of scapula fractures:results of 39patients[J].Injury,2013,44(11):1630-1635.
[6]Cole PA,Freeman G,Dubin JR.Scapula fractures[J].Curr Rev Musculoskelet Med,2013,6(1):79-87.
[7]Wijdicks CA,Armitage BM,Anavian J,et al.Vulnerableneurovasculature with a posterior approach to the scapula[J].Clin Orthop Relat Res,2009,467(8):2011-2017.
[8]Wijdicks A,Anavian J,Hill W,et al.The assessment of scapular radiographs:analysis of anteroposterior radiographs of the shoulder and the effect of rotational offset on the glenopolar angle[J].Bone Joint J,2013,95(8):1114-1120.
[9]Cole PA,Talbot M,Schroder LK,et al.Extra-articular malunions of the scapula:a comparison of functional outcome before and after reconstruction[J].J Orthop Trauma,2011,25(11):649-656.
[10]崔立群,杨志成,陈金钢.移位肩胛颈和体部骨折的手术治疗[J].中华创伤杂志,2010,26(7):614-616.
Clinical results of using minimally invasive approach in combination with triangle principle for internal fixation of displaced scapula neck and body fractures
Li Renbin,Lin Yanbin,Xiong Shengren,Zhuang Yan,Xiong Guosheng,Zhang Yiyuan.Department of Orthopaedic,Xiamen University Affiliated Fuzhou Second Hospital,Fuzhou 350007,China
Li Renbin,Email:lirenbin1009@medmail.com.cn
BackgroundThe scapular fracture is rarein clinic,accounting for about 0.5%-1%of fractures in the whole body.The scapular body and neck can be involved in 98%of scapular fractures.Generally,thesurgical treatment is required forscapular body fractures with glenopolar angle of less than 22°,lateral and shortening displacement of more than 3cm and angulation displacement of more than 40°.78.1%of the scapular fractures can be treated through posterior approach.The scapula is a triangle-like flat bone:the 3sides include the connection between mesoscapula and scapular body,the medial margin and the lateral margin;the 3corners include the inner upper corner,the lower angle corner and the glenoid neck.According to the surgical indications of scapular neck and body fractures,two or three margins are often involved.To build a stable triangle,the author came up with the triangle theory of fixing every margin affected by fractures.In this study,agroup of patients with scapular body and neck fractures was treated with minimally invasive approachin combination with triangle principle to evaluate the corresponding clinical efficacy.Methods(1)General data.From June 2012to December 2014,23patients(16males and 7females)with an average age of 37.58years(19-62years)were treated for the scapular body and neck fractures with plate fixation via posterior minimally invasive approach in our hospital.The associated injuries included 9cases of multiple rib fractures,6cases of hemopneumothorax and (or)pulmonary contusion,5cases of craniocerebralinjury,2cases of cervical spine injury,4cases of ipsilateral clavicle fractures and 4cases of pelvic fractures.According to the Hardegger classification,18cases of scapular body fractures and 5cases of scapular neck fractures were in this group,including 3cases of surgical neck fractures and 2cases of fractures of spina scapulae.The average time from injury to operation was 7.8days(5-16days).All patients
preoperative shoulder fluoroscopic examinations of traumatic series and CT scan with 3Dreconstruction.The types of fractures for all patients in the group fitted for the indications of limited open reduction and the plate internal fixation through posterior minimally invasive approach.Moreover,all patients received surgical procedures within 4weeks of the injury.There were no anterior glenoid fractures,coracoid fracturesand acromial fractures.Also,multiple fracture fragments were not found in lateral column,mesoscapula and medial margin.(2)Surgical methods.The patient was put with the prone positionafter successful general anesthesia,and the incisions were made based on the type of fractures.The principles of choosing incisions:the incision A or B for the fractures involving lateral margin;the incision C or D for the fractures involving medial margin;the incision E for the fractures involving superior margin.The fracture ends could be exposed along the intermuscular space between infraspinatus muscle and teres minor muscle via the incision A or B.If the incision C or D was chosen,the skin above the medial margin of scapula wascut open longitudinally to expose the fracture ends.The incision E could be used for the upper margin fractures of scapula.During the operation,the reconstruction plate was not used dueto difficult placement of long plates into the 3-5cm incision being made.The 2.7mm dynamic compression plates or reconstruction plates were used for allpatients of this group,and the 2.4mm locking plates could be used for the medial margin.The incision A does not require the cutof the posterior deltoid muscle.During the traction of infraspinatus muscle,special attention should be paid to avoid the damage of the nervi suprascapularis and to deal with the ascending branch of circumflex scapular artery which locates 5-6cm below the lateral margin of scapula and the lower margin of glenoid.Most of the fracture ends locate in the inner corner of scapula.After fascia and periosteum were separated along the margo vertebralis scapulae,the infraspinatus muscle was disassociated until the fracture ends were detected,restored and fixed.First of all,the lateral margin was fixed because the medial plate instead of the lateral plate often requires pre-bending.Besides,the fixation of lateral margin facilitated the restoration and the fixation of themedial margin fracture.The upper margin fracturewas treated by the incision made along the mesoscapula and the blunt dissociation of infraspinatus muscle.The nervi suprascapularis and superior scapular artery and vein should be carefully protected at the site of scapular notch.(3)Postoperative management.The drainage was not placed postoperatively,and the pendulumlike movement,passive flexion and external rotation exercise began on the second day after the surgery.Afterward,the passive internal rotation,adduction and abduction exercises couldbe gradually introduced.According to the fracture healing shown by fluoroscopy,agradual transition to active exercises was conducted during the follow-up period.Strength training was initiated 12weeks later,and activities in all directions were reinforced at the same time.(4)Postoperative follow-ups and evaluation indexes.All patients were followed up postoperatively once per month within half a year,once per 3months half a year later and once per 6months one year later.The postoperative X-ray examinations of shoulder joint included anterior view,posterior view and Y view.All patients were investigated by questionnaire,and all of the postoperative fluoroscopies were evaluated by 2physicians independently to decidethe presence of nonunion or malunion.The diagnostic standards of malunion:more than 0.5cm of separate displacement in anterior view,posterior view and Y view;more than 10°of angular displacement in Y view.During the lastfollow-up,the disabilities of the arm,shoulder and hand(DASH)score of each patient was used as the final functional evaluation index.Results The mean operation time was 78.6 min(58-121min),and the average amount of bleeding was 68.3ml(50-100ml).No complications occurred in patients.The mean follow-up time was 17.7months(9-36months).None of the patients had wound infection or poor healing,and allwounds reached level I healing.All fractures were well restored,and there was no fracture displacement,malunion or nonunion.The average healing time was2.5months(2-3months).During the follow up of all cases,no case was found with screw loosening,withdraw or breakage.The postoperative index of shoulder joint functions for patients:the mean range of forward elevation was 162°(150-180°);the mean range of abduction was 110°(90-120°);the mean range of lateral rotation was 54°(45-60°).The average DASH score was 7.8points (4-21points).Conclusions Minimally invasive posterior approach combined with triangle fixation principle for treating scapular body and neck fractures reduces the stripping of flaps and posterior scapular muscles through limited incision.Intraoperative ligation of the circumflex scapular artery effectively protects suprascapular artery and vein,which significantly reduces the amount of bleeding.This method allows fracture reduction under direct vision without exposure of multiple fracture lineson the scapular body.Through multiple minimally invasive approaches,three edges of the scapula are reconstructed to achieve stability with less operation time and good outcomes,which is beneficial for early functional rehabilitation.Having the advantages of small incision and better-looking appearance,this surgical strategy is worth of promotion.
Minimally invasive;Triangular fixation;Scapula;Fracture;Internal fixation
2016-9-27)
(本文编辑:胡桂英;英文编辑:陈建海、张晓萌、张立佳)
10.3877/cma.j.issn.2095-5790.2017.01.006
福州市科技局社会发展项目(2016-S-123-16)
350007 厦门大学附属福州第二医院骨科
李仁斌,Email:lirenbin1009@medmail.com.cn
李仁斌,林焱斌,熊圣仁,等.后侧微创入路结合三角固定原则治疗肩胛体及肩胛颈骨折[J/CD].中华肩肘外科电子杂志,2017,5(1):29-35.
