替罗非班给药途径及时机对急性心肌梗死患者术中无复流的影响
2017-07-01刘继文汤曾耀王新旺刘玉连曾紫微朱保成乔凌维
刘继文,汤曾耀,王新旺,刘玉连,曾紫微,朱保成,乔凌维
• 论著 •
替罗非班给药途径及时机对急性心肌梗死患者术中无复流的影响
刘继文1,汤曾耀1,王新旺1,刘玉连1,曾紫微1,朱保成1,乔凌维1
目的 探讨替罗非班给药途径及时机对急性心肌梗死(AMI)患者术中无复流的影响。方法 选择2015年7月~2016年7月间就诊于九江市第一人民医院诊断为AMI并接受急诊经皮冠状动脉介入治疗(PCI)患者110例,根据替罗非班给药方式不同分为A、B1和B2三组。A组(32例)患者于急诊室静脉注射替罗非班,B组患者冠状动脉内注射替罗非班,其中B1(38例)组患者于血管开通前经指引导管注入,B2组(40例)患者于球囊扩张后或PCI后出现无复流时经微导管给药。其中A组及B1组患者如球囊扩张或PCI术后仍有无复流者可经指引导管再次注入替罗非班,其统计组不变。比较各组靶血管开通前后及支架植入后即刻TIMI血流分级和矫正TIMI血流帧(CTFC)计数、替罗非班给药剂量和术后出血情况。结果 A组和B1组靶血管开通前TIMI血流分级和CTFC均优于B2组,差异有统计学意义(P<0.05),A组与B1组间比较差异无统计学意义(P>0.05);A组和B1组靶血管开通后TIMI血流分级优于B2组,差异有统计学意义(P<0.05),且B1组优于A组,差异有统计学意义(P<0.05);支架植入后即刻B2组靶血管TIMI血流分级和CTFC优于A组和B1组,差异有统计学意义(P<0.05),而A组和B1组两组间比较差异无统计学意义(P>0.05)。B2组术中替罗非班用量少于A组及B1组(P<0.05),但A组和B1组两组间比较差异无统计学意义(P>0.05)。B2组替罗非班给药剂量显著少于A组和B1组,B1组少于A组,差异有统计学意义(P<0.05);B2组术后出血发生率最低,且显著低于A组(P<0.05),与B1组比较差异无统计学意义(P>0.05)。结论 替罗非班给药途径及时机不同对行PCI术治疗的AMI患者血流灌注影响不同,其中急诊室静脉注射能更早改善血流状态,而PCI术中冠状动脉内注射尤其是闭塞开通后给药对血流灌注的改善作用更强,替罗非班用量更小,术后出血更少。
替罗非班;无复流;急性心肌梗死;经皮冠状动脉介入
急性心肌梗死是常见的心血管内科疾病,其主要发病机制为冠状动脉斑块破裂造成的冠状动脉闭塞和急性血栓形成,对患者的生命健康造成严重威胁[1,2]。梗死相关动脉(IRA)的再通和心肌细胞水平的有效灌注是治疗的关键,急诊经皮冠状动脉介入治疗(PCI)是尽早开通IRA的最有效方法之一,已成为AMI再灌注治疗的首选。在PCI术中或术后常发生冠状动脉慢血流及无复流等并发症,严重影响患者生存率及预后[3,4]。血小板过度激活引起的冠状动脉内血栓碎片形成是PCI术中心肌灌注不良和无复流的重要原因。替罗非班是强效、速效、短效的血小板抑制剂,目前的使用方法有在急诊室静脉注射和PCI术中冠状动脉内注射两种方法,而冠状动脉内给药的时机方法亦有不同[5-7]。目前在以上方面研究较少,临床证据相对不足,基于此我们设计实验,评价不同时间窗和不同的给药方法对术中无复流的防治效果。
1 资料与方法
1.1 临床资料 选择2015年7月~2016年8月连续于九江市第一人民医院血管中心(胸痛中心)确诊为AMI并接受急诊PCI患者110例。AMI诊断标准:典型的缺血性胸痛持续时间>30 min;心电图两个或两个以上相邻导联ST-T段动态改变,新发生或怀疑发生的左束支传导阻滞;心肌酶谱肌酸激酶同工酶(CK-MB)超过正常值上限2倍,肌钙蛋白阳性。入选标准:①年龄40~80岁;②符合急诊PCI适应证的AMI患者;③同意接受急诊PCI治疗患者。排除标准:①合并活动性出血及凝血功能障碍患者;②急性心力衰竭及严重肝肾功能不全患者;③近期有大手术、恶性肿瘤患者;④造影剂过敏者。根据替罗非班给药方法不同分A、B1和B2三组。三组一般资料见表1。
1.2 给药方法 所有患者PCI术前即刻给予肠溶阿司匹林300 mg嚼服、氯吡格雷600 mg及阿托伐他汀40 mg口服。术中所有患者给予普通肝素100 μg/kg,时间每超过1 h追加1000 U。术后全部患者均应用依诺肝素4000 U,1/12 h,连续5~7 d。同时口服氯吡格雷75 mg/d、阿司匹林100 mg/d。A组:急诊室静脉注射替罗非班(山东新时代药业有限公司生产,规格12.5 mg),入院后急诊室早期静脉推注10 μg/kg的替罗非班;B组:冠状动脉内注射替罗非班,其中B1组:血管开通前经指引导管注入,冠状动脉造影后于冠状动脉口推注10 μg/kg的替罗非班;B2组:球囊扩张后或PCI后出现无复流时经微导管注入10 μg/kg的替罗非班,再行支架置入。替罗非班负荷剂量给药后如果还有无复流,继续以每次5 μg/kg剂量推注,最大剂量不超过20 μg/kg。
表1 三组一般资料比较[(±s),(n,%)]
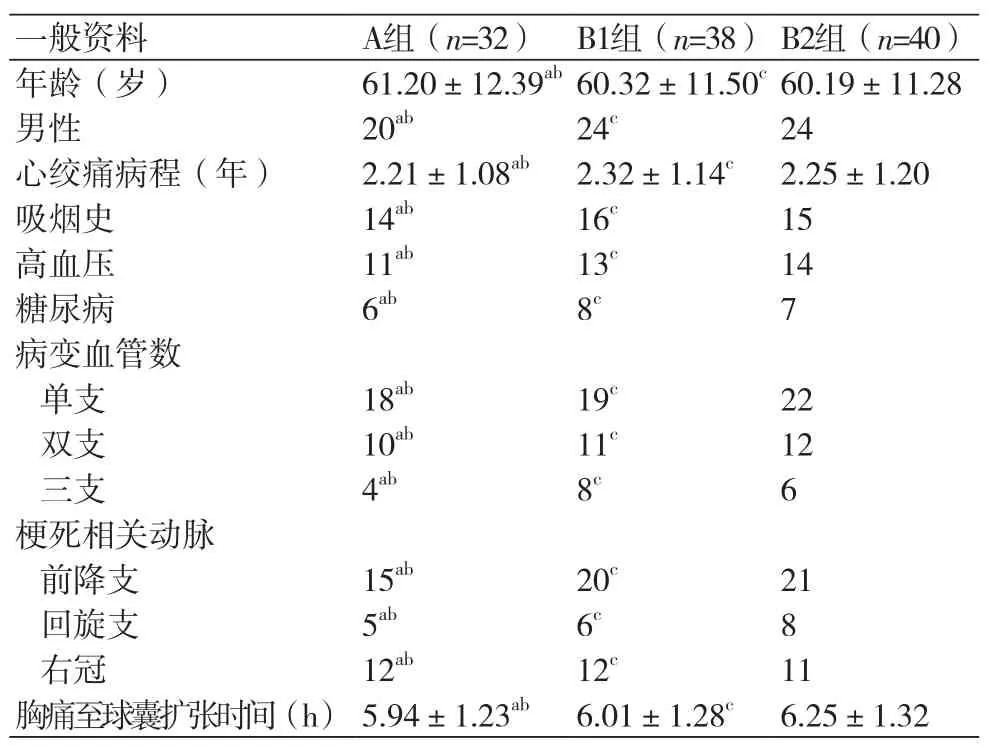
表1 三组一般资料比较[(±s),(n,%)]
注:A与B2组比较,aP>0.05;A与B1组比较,bP>0.05;B1组与B2组比较 ,cP>0.05
一般资料 A组(n=32) B1组(n=38)B2组(n=40)年龄(岁) 61.20±12.39ab60.32±11.50c60.19±11.28男性 20ab24c24心绞痛病程(年) 2.21±1.08ab2.32±1.14c2.25±1.20吸烟史 14ab16c15高血压 11ab13c14糖尿病 6ab8c7病变血管数单支 18ab19c22双支 10ab11c12三支 4ab8c6梗死相关动脉前降支 15ab20c21回旋支 5ab6c8右冠 12ab12c11胸痛至球囊扩张时间(h) 5.94±1.23ab6.01±1.28c6.25±1.32
1.3 观察指标
1.3.1 血流情况采用TIMI血流分级和矫正 TIMI血流帧(CTFC)计数评价各组血流情况,分别于靶血管开通前后及支架植入后即刻各评价一次。TIMI血流分级包括0级:无血流灌注;1级部分造影剂通过;2级狭窄远端可完全充盈;3级血流灌注正常。其中TIMI血流0~1级为无复流。
1.3.2 替罗非班给药剂量和术后出血情况 记录替罗非班给药剂量,观察术后出血情况,包括主要出血:颅内出血或临床可见出血(包括影像学)伴血红蛋白浓度下降≥5 g/dL;小出血:临床可见出血伴血红蛋白浓度下降3~5 g/dL;轻微出血:临床可见出血伴血红蛋白浓度下降<3 g/dL。
1.4 统计学分析 所有资料采用SPSS 17.0统计软件进行处理,计数资料用百分比(%)表示,采用卡方检验和非参数检验;计量资料用均数±标准差(±s)表示,采用方差分析和t检验;P <0.05为差异有统计学意义。
2 结果
2.1 各组靶血管开通前后及支架植入后即刻血流情况比较 A组和B1组靶血管开通前TIMI血流分级和CTFC优于B2组(P<0.05),但A组和B1组两组间比较差异无统计学意义(P>0.05);A组和B1组靶血管开通后TIMI血流分级和CTFC优于B2组(P<0.05),且B1组优于A组,差异有统计学意义(P<0.05);支架植入后即刻B2组靶血管开通前TIMI血流分级和CTFC优于A组和B1组(P <0.05),而两组间比较差异无统计学意义(P >0.05),见表2。
2.2 各组替罗非班给药剂量和术后出血情况比较B2组替罗非班给药剂量显著少于A组和B1组,B1组少于A组,差异有统计学意义(P<0.05)。各组术后出血情况比较结果显示,B2组出血发生率最低,且显著低于A组(P<0.05),与B1组比较差异无统计学意义(P>0.05),见表3。
表2 各组靶血管开通前后及支架植入后即刻TIMI血流分级和CTFC比较[(±s),(n,%)]
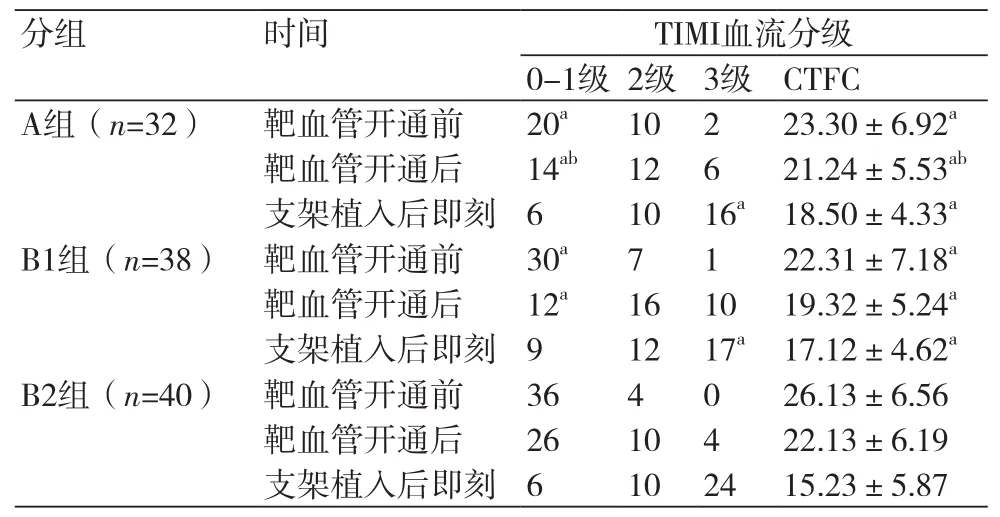
表2 各组靶血管开通前后及支架植入后即刻TIMI血流分级和CTFC比较[(±s),(n,%)]
注:与B2组比较,aP<0.05;与B1组比较,bP<0.05
分组 时间 TIMI血流分级0-1级 2级 3级 CTFC A组(n=32) 靶血管开通前 20a10 2 23.30±6.92a靶血管开通后 14ab12 6 21.24±5.53ab支架植入后即刻 6 10 16a18.50±4.33aB1组(n=38) 靶血管开通前 30a7 1 22.31±7.18a靶血管开通后 12a16 10 19.32±5.24a支架植入后即刻 9 12 17a17.12±4.62aB2组(n=40) 靶血管开通前 36 4 0 26.13±6.56靶血管开通后 26 10 4 22.13±6.19支架植入后即刻 6 10 24 15.23±5.87
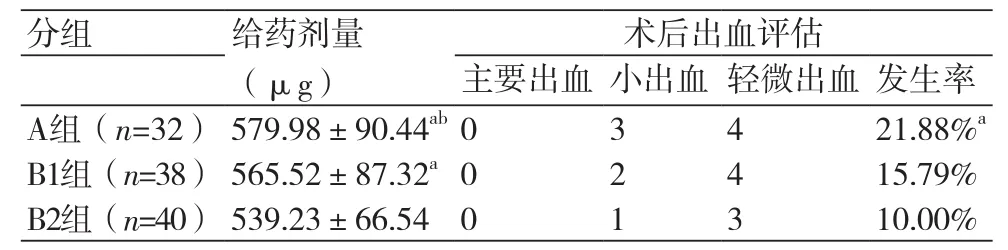
表3 各组术后出血情况比较(n,%)
3 讨论
AMI形成的主要原因是冠状动脉粥样的斑块破裂和继发性血栓形成,早期、迅速恢复梗死相关动脉的前向血流,可挽救濒死心肌,保护和恢复受损的左心室功能,减少左室重构,改善患者的预后[8]。但急性ST段抬高型心肌梗死患者冠状动脉内血栓负荷往往较重,常规的球囊扩张及支架置入时,新鲜血栓或斑块被压碎而脱落,易致术中或术后慢血流及无复流等并发症,将抵消血管再通所带来的获益[3,4]。与心肌充分复流的患者相比,无复流患者恶性心律失常、左心室功能不全的发生率和病死率增加5~10倍,严重影响患者预后[9,10]。目前研究表明无复流现象是由多种因素共同作用而导致微循环障碍所致,其机制包括:血栓栓塞、内皮细胞肿胀、血管痉挛、炎症因子分泌、内膜损伤、支架贴壁不良等[11],而血小板的过度激活及聚集是其主要原因,在AMI围手术期,不充分的抗血小板治疗将明显增加慢血流及心血管不良事件发生[12],因此围手术期的抗血小板治疗至关重要。
治疗无复流的策略可分为器械和药物两方面。直接支架植入、血栓抽吸以及远端保护装置的应用减少了无复流的发生,但仍然不能抑制持续、过度激活的血小板,此时血小板过度激活及其活性物质释放是产生慢血流、无复流的主要原因[13]。血小板膜蛋白Ⅱb/Ⅲa受体拮抗剂(GPI)替罗非班阻断血小板聚集的最后共同通路,是强效、速效、短效的血小板抑制剂,有良好的抗无复流作用。
替罗非班目前的使用方法有在急诊室静脉注射和PCI术中冠状动脉内注射两种方法,而冠状动脉内给药的时机方法亦有不同。研究表明不同时间窗及不同前向血流条件下使用替罗非班可让患者临床获益有所差异[5-7],因此如何在AMI患者中应用替罗非班对患者预后至关重要。
本研究对比了急诊室静脉注射、血管开通前冠状动脉内注射和血管开通后冠状动脉内注射三种给药方式和给药时机下对患者的影响,采用靶血管开通前后和TIMI血流分级、CTFC,替罗非班给药剂量和出血情况评价效果。结果发现,急诊室静脉注射能更早改善血流状态,而PCI术中冠状动脉内注射尤其是闭塞开通后给药对血流灌注的改善效果更强,目前多数观点认为,替罗非班不同途径和时机给药对PCI术治疗的AMI患者血流灌注影响不同,心脏功能和预后多无明显差异,安全性均较好[14,15]。急诊室静脉给药时间早,可更早发挥抗血小板作用,血流灌注早期血管开通前就能发挥一定的效果;但由于是全身用药,药物不能直达靶点,其转运过程中还经肝脏首过效应、自身代谢及血液稀释,到达冠状动脉的浓度降低使其效果削弱。冠状动脉内给药将药物直接注入血栓部位,局部药物浓度高,给药后可以快速、强效改善血流状况。与血管开通前比较,血管开通给药作用于闭塞远端,可以更好的发挥溶栓治疗效果,并在PCI术后发挥更强的血流灌注改善效果[4]。此外,血管开通后给药,替罗非班给药剂量、术后出血风险均大大降低,安全性显著提高。
[1] 王丽,何艺,冉华,等. 术前小剂量替罗非班改善急性冠脉综合征患者PCI治疗预后情况的临床研究[J]. 海南医学院学报,2016,22(11):1058-61.
[2] Vlaar PJ,SvilaasT,van der Horst I C,et al. Cardiac death and reinfarction after 1 year in the thrombus aspiration during percutaneous coronary intervention in acute myocardial infarction study(TAPAS):a1-year follow-up study[J]. Lancet,2008,371(9628): 1915-20.
[3] Buyukkaya E,Poyraz F,Karakas MF,et al. Usefulness of monocyte chemoattractant protein-1 to predict no-reflow and three-year mortality in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention[J].Am J Cardiol,2013,112(2):187-93.
[4] Ergelen M,Uyarel H,Gül M,et al. Efficacy and outcome of primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction due to saphenous vein graft occlusion[J]. Turk Kardiyol Dern Ars,2010,38(8):531-6.
[5] Akpek M,Sahin O,Sarli B,et al. Acute Effects of Intracoronary Tirofiban on No-Reflow Phenomena in Patients With ST-Segment Elevated Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention[J]. Angiology,2015,66(6):560-7.
[6] 李超,程自平,陈刚,等. 不同时间窗应用替罗非班对PCI术中无复流的疗效观察[J]. 安徽医科大学学报,2015,50(1):119-21.
[7] Yang TY,Chang ST,Chung CM,et al. Restoration of normal coronary flow with tirofiban by intracoronary administration for no-reflow phenomenon after stent deployment[J]. Int Heart J,2005,46(1):139-45.
[8] Akpek M,Elcik D,Kalay N,et al. The prognostic value of serum gamma glutamyl transferase activity on admission in patients with STEMI undergoing primary PCI[J]. Angiology,2012,63(8):579-85.
[9] Stone GW,PetersonMA,Lansky A2,et al. Impact of normalized myocardial perfusion after successful angioplasty in acute myocardial infarction[J]. J Am Coll Cardio,2002,39(4):591-7.
[10] Zhao HJ,Yan HB,Wang J,et al. Comparison of Diver CE and ZEEK manual aspiration catheters for thrombectomy in STsegment elevation myocardial infarction[J]. Chin Med J(Engl),2009,122(6):648-54.
[11] Yun KH,ShinIS,ShinSN,et al. Effect of previous statin therapy in patients with acute coronary syndrome and percutaneous coronary intervention[J]. Korean Cire J,2011,41(8):458-63.
[12] Thiele H,Schindler K,Friedenberger J,et al. Intracoronary compared with intravenous bolus abciximab application in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention: the randomized Leipzig immediate percutaneous coronary intervention abciximab IV versus IC in ST-elevation myocardial infarction trial[J]. Circulation,2008,118(1):49-57.
[13] Jagroop IA,Mikhailidis DP. The effect of tirofiban on fibrinogen/ agonist-induced platelet shape change and aggregation[J]. ClinApplThromb Hemost,2008,14(3):295-302.
[14] SayuriFriedland,BSca,Mark J. Eisenberg,et al. Meta-Analysis of Randomized Controlled Trials of Intracoronary Versus Intravenous Administration of Glycoprotein IIb/IIIa Inhibitors During Percutaneous Coronary Intervention for Acute Coronary Syndrome[J]. Am J Cardiol 2011,108(9):1244-51.
[15] 孙宇珺,周雯,丁嵩,等. 经靶向灌注导管在冠状动脉靶病变远段给予替罗非班对急性冠状动脉综合征患者心肌灌注的影响[J].中国介入心脏病学杂志,2015,23(1):5-10.
本文编辑:陈亚磊,田国祥
Effect of tirofiban route and timing on intraoperative no - reflow in patients with acute myocardial infarction
LIU Ji-wen*, TANG Zeng-yao, WANG Xin-wang, LIU Yu-lian, ZENG Zi-wei, ZHU Bao-cheng, QIAO Ling-wei.*Department of Cardiology, the First People 's Hospital of Jiujiang City, Jiangxi Province, Jiujiang 332000, China.
LIU Ji-wen, E-mail: liujiwen519@163.com
Objective To explore the effects of tirofiban administrated at different routes and timing on noreflow in patients with acute myocardial infarction. Method 110 AMI patients were divided into group A and group B (including B1 and B2) according to the different ways of administration. Group A (n=32)
intravenous tirofiban in the emergency department, group B was treated with tirofiban by intracoronary administration. Among them, group B1 (n=38) was injected via guide catheter before the vessel was opened. Patients in group B2 (n=40) were given tirofiban via microcatheterization after balloon dilatation or PCI when no reflow occurred. Among the group A and B1, tirofiban could be re-injected when there was no flow after balloon expansion or PCI. TIMI flow grade and corrected TIMI blood flow count (CTFC), intraoperative tirofiban dosage, hospital adverse cardiac events (MACE), and postoperative bleeding were compared before and after target vessel stenting and stent implantation. Results TIMI blood flow grade and CTFC were superior to group B2 (P<0.05) in group A and group B1 before the target vessel is opened, and there was no statistically significant difference between A and B1 groups (P>0.05). The blood flow of TIMI in group A and group B1 was better than that in group B2 after the target vessel is opened (P<0.05), and B1 group was better to group A (P<0.05). TIMI blood flow grade and CTFC of target vessel in group B2 were better than that of group A and group B1 after Immediately stent implantation (P<0.05), and there was no significant difference between A and B1 groups (P>0.05). In group B2, the dosage of tirofiban was significantly less than that of group A and group B1 (P<0.05), and B1 group was less than that of group A (P<0.05). The incidence of postoperative bleeding in group B2 was the lowest, which was significantly lower than that in group A (P<0.05), and there was no significant difference compared with group B1 (P>0.05). Conclusion There have different effects on the blood perfusion of patients with AMI when treated with tirofiban on different routes and timing. In the emergency room intravenous tirofiban can improve coronary blood flow status earlier. Intracoronary injection of tirofiban duringthe PCI operation, especially after the opening of the occluded blood vessels, can more improved the blood perfusion with lower doses and less postoperative bleeding.
Tirofiban; No-reflow; Acute myocardial infarction; Percutaneous coronary intervention
R541.4
A
1674-4055(2017)05-0556-03
江西省卫生计生委科技计划项目(20167106)
1332000 九江,江西九江市第一人民医院总院心内科
刘继文,E-mail:liujiwen519@163.com
10.3969/j.issn.1674-4055.2017.05.11
