Ficat III 期股骨头坏死并滑膜软骨瘤病一例报告
2017-06-01王亚康秦四清江仁奇张育民
王亚康 秦四清 江仁奇 张育民
·病例报告 Case report·
Ficat III 期股骨头坏死并滑膜软骨瘤病一例报告
王亚康 秦四清 江仁奇 张育民
骨坏死;股骨头坏死;软骨瘤,滑膜;关节成形术,置换,髋;髋关节
滑膜软骨瘤病是一种关节骨膜自限性增殖性的良性疾病,由滑膜内层结缔组织增生并化生成多数软骨结节,钙化、骨化而脱离滑膜,进入关节腔,形成大量游离小体。该病好发年龄为 30~50 岁,男性多于女性,绝大多数发生在单关节[1]。
患者,男,34 岁,右髋疼痛,活动受限渐进性加重2 年入院,2 年前患者无明显诱因感觉右髋疼痛,活动时加重,休息后减轻,其后疼痛逐渐加重。拍片提示:右股骨头坏死,患者既往有饮酒史 10 年,约 50 g / 天,吸烟史18 年,约 15 支 / 天;入院查体:右髋部皮肤无发红,右腹股沟中点压痛阳性,大粗隆叩击痛及下肢叩击痛阳性,右髋 4 字试验阳性,右髋关节内收及外展活动受限,右髋屈伸活动度 80°~0°~10°,右下肢皮肤感觉及末梢血运良好,足趾活动正常。辅助检查:X 线片 ( 双髋正位,双髋侧位 ) 显示:双髋关节间隙狭窄,关节软骨下骨质硬化,右关节面欠光滑,双侧股骨头负重区出现囊样变 ( 图 1 );CT:见双侧股骨头内骨小梁消失,出现大小不等的囊样骨质侵蚀,周围出现骨硬化环 ( 图 2 );MRI:在 T1WI 双关节表现为广泛的高信号,关节囊内局灶性高信号,关节囊样变表现;在 T2WI 中可以看到明显的双边征表现关节周围水肿,局灶性低信号 ( 图 3 )。C-反应蛋白:26.60 mg / L,血沉:32 mm / h,类风湿因子及抗“O”均正常。初步诊断:双侧股骨头坏死。

图 1 髋关节 X 线片:双髋关节间隙狭窄,关节软骨下骨质硬化,右髋关节面不平整,双侧股骨头负重区出现囊样变 a:双髋正位;b:双髋侧位Fig.1 Hip X-rays: Both spaces of the hip joints were narrowed, subchondral bony tissue was sclerotic and right articular surface was not fl at, bilateral loading area of femoral head appeared to have cystic degeneration a: Anteroposterior fi lms of the hips; b: Lateral position fi lms of the hips
在全麻醉下行双侧股骨头坏死右人工全髋关节置换术,术中见关节囊内有满视野黄豆大小、乳白色实性增生物,骨股头变形,关节软骨缺失 ( 图 4 )。病理诊断:滑膜软骨瘤 ( 图 5 )。出院诊断:( 1 ) 双侧股骨头坏死;( 2 ) 右髋滑膜软骨瘤病。
讨 论
本病的主要临床表现为关节疼痛、肿胀、活动受限。患者感觉关节内有异物感及摩擦感有时会出现关节弹响及交锁现象。
滑膜软骨瘤病的病因较为复杂,根据病因可分为原发性滑膜软骨瘤病和继发性滑膜软骨病。原发性滑膜软骨瘤病的病因尚不明确,而继发性滑膜软骨瘤病可继发于骨关节炎,缺血性骨坏死,剥脱性骨软骨炎,色素沉着绒毛结节性滑膜炎及类风湿性骨关节炎等病因[2-3]。其主要的发病机制为:关节囊内滑膜结缔组织的增生和化生。依据发病机制又分为四种学说:( 1 ) 外伤学说,受伤后滑膜软骨异常增生出现滑膜软骨瘤;( 2 ) 滑膜化生学说,正常关节滑膜反折可以使滑膜软骨细胞化生为软骨或软骨小岛;( 3 ) 畸形学说,滑膜因为有胚胎性细胞,成年分化为软骨;( 4 ) 肿瘤学说,滑膜软骨瘤属于良性肿瘤,具有自限性[4]。
依据本病的病程进展,Milgram[5]将本病分为 3 期:I 期:活动性滑膜内病变;II 期:过渡性滑膜病变合并滑膜软骨瘤及游离体;III 期:滑膜病变静止,形成数枚游离体,在 I 期和 II 期中,X 线片中看不到游离体,只有在MRI 状况下可以观察到游离体病变,而在 III 期 X 线中可以看到滑膜组织中出现游离体。滑膜软骨瘤治疗方案主要为手术治疗。主要是通过关节镜清除关节腔内游离体及依据病变情况进行病变滑膜的切除[6],个别病例需切开手术,髋关节由于关节间隙狭窄,需手术治疗,关节囊切开脱位髋关节清理髋关节手术也是常用的治疗手段,然而脱位手术治疗后,随访中发现术后并发症也较多[7-8]。如合并股骨头坏死需关节置换术可行切开治疗[9]。如本例患者则须行开放性手术治疗。
依据患者辅助检查可以判定,本例患者的 X 线片及CT 中未看到软骨瘤游离体的形成,但是术中见到大量的软骨结节,所以该病情属于 Milgram 分期的 II 期,X 线片和 CT 片,显示股骨头囊样改变,在术切开股骨头可以看到空腔囊样改变,所以为股骨头坏死 Ficat 分期 II 期[5,10]。

图 2 髋关节 CT:可见双侧股骨头内骨小梁消失,出现大小不等的囊样骨质侵蚀,周围出现骨硬化环Fig.2 The CT showed that bilateral femoral trabecular bone disappeared, there was showed large cystic bone erosion and sclerotic bone ring

图 3 在 T1WI 双关节表现为广泛的高信号,关节囊内局灶性高信号,关节囊样变表现;在 T2WI 中可以看到明显的双边征表现关节周围水肿,局灶性低信号 a:T1WI;b:T2WIFig.3 T1WI double joint for a wide range of high performance signal focal signal within the joint capsule, capsule-like performance; On T2WI, we could see clear signs of bilateral edema around the joint, focal low signal a: T1WI; b: T2WI

图 4 关节囊内有满视野黄豆大小、乳白色实性增生物,骨股头变形,关节软骨缺失 a:股骨头内病变;b:髋臼内病变Fig.4 Loose bodies in acetabular with full view; Deformation of femoral head with loss of articular cartilage a: Femoral head lesion; b: Acetabular lesion
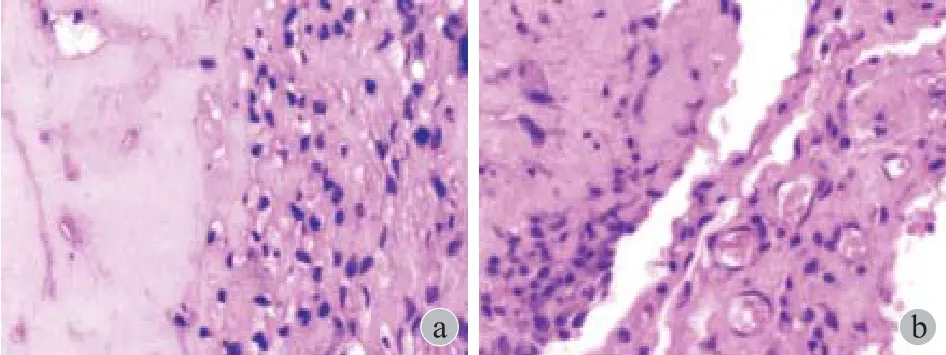
图 5 病理诊断 a:可见分叶状、多发性、透明软骨形成;b:外层可见滑膜细胞包绕,病变内有多核像、核聚积及核深染( HE × 100 )Fig.5 Pathological diagnosis a: Lobulated, multiple myelomalike, hyaline cartilage formation; b: Synovial cells wrapped the outer, lesions in the nuclei, nuclear accumulation and hyperchromatic nuclei ( HE × 100 )
本例术前 X 线,CT 未看到关节腔内存在游离体,MRI 在 T2加权中见到滑膜组织的明显水肿增厚,和髋臼内出现游离体及股骨头骨质的破坏溶解。而患者的 X 线表现为关节间隙狭窄和关节下骨质硬化,与 Kim 等[11]的研究相似,而患者在坏死的早期即表现股骨头负重区囊样变的表现不同,并且术前血沉、C-反应蛋白均增高,首先考虑患者由于滑膜水肿,无菌性炎症刺激引用,逐渐出现关节腔内纤维组织增生形成关节腔内游离体,进而引起关节腔内压力增高和引起股骨头坏死[12-13]。但是患者股骨头明显出现囊样变性,并且患者股骨头出现部分塌陷,属于股骨头坏死的中后期,而滑膜软骨瘤病却属于发病的早期,所以不得不考虑另外一种坏死机制,即由于其它原因导致股骨头坏死而进一步引起滑膜水肿,进而出现滑膜软骨瘤病,即早在 1979 年 Milgram 报告 1 例随访 27 年的患者即先出现股骨头坏死,而后出现滑膜软骨瘤病,作者认为滑膜软骨瘤既可以为关节坏死的继发性疾病,也可以为独立的原发性滑膜软骨瘤病的独立病存在[13]。纪泉等[14]学者认为误将滑膜软骨瘤病诊断为股骨头缺血性坏死。也有学者报道滑膜软骨瘤病和股骨头坏死并存[12,15]。到底是股骨头坏死引起滑膜软骨瘤病,或者是前者继发后者,又或者二者独立并存的两种疾病。然而本病的具体发病机制及分子信号通路仍然有待于更为深入的研究,来明确二者的关系。
[1] Giancane G, de Horatio LT, Buonuomo PS, et al. Swollen knee due to primary synovial chondromatosis in pediatrics: a rare and possibly misdiagnosed condition[J]. Rheumatol Int, 2013, 33(8):2183-2185.
[2] Peh WC, Shek TW, Davies AM, et al. Osteochondroma and secondary synovial osteochondromatosis[J]. Skeletal Radiol, 1999, 28(3):169-174.
[3] Duif C, Von SPC, Ali A, et al. Primary synovial chondromatosis of the hip - is arthroscopy suff i cient? A review of the literature and a case report[J]. Technol Health Care, 2014, 22(5):667-675.
[4] 杨先甲, 汪亚玲, 蔡秀华, 等. 滑膜软骨瘤病研究进展[J]. 骨科, 2015, (6):332-336.
[5] Milgram JW. Synovial osteochondromatosis: a histopathological study of thirty cases[J]. J Bone Joint Surg Am, 1977, 59(6): 792-801.
[6] Kim HG, Park KH, Huh JK, et al. Magnetic resonance imaging characteristics of synovial chondromatosis of the temporomandibular joint[J]. J Orofac Pain, 2002,16(2): 148-153.
[7] Nakamura Y, Echigoya N, Toh S. Synovial osteochondromatosis of the hip treated through a surgical dislocation[J]. J Arthroplasty, 2009, 24(7):1143.e15-19.
[8] Lim SJ, Park YS. Operative treatment of primary synovial osteochondromatosis of the hip. Surgical technique[J]. J Bone Joint Surg Am, 2007, 89(Suppl 2)Pt.2:232-245.
[9] 许杰, 马若凡, 李亮平, 等. 髋关节滑膜软骨瘤病临床病例诊治分析[J]. 中华关节外科杂志 (电子版), 2012, 6(5):14-17.
[10] Ficat RP. Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment[J]. J Bone Joint Surg Br, 1985, 67(1):3-9.
[11] Kim SH, Hong SJ, Park JS, et al. Idiopathic synovial osteochondromatosis of the hip: radiographic and MR appearances in 15 patients[J]. Korean J Radiol, 2002, 3(4): 254-259.
[12] 王信胜, 张喜善, 阮汝清, 等. 髋关节 256 颗滑膜软骨瘤并股骨头缺血坏死 1 例报告[J]. 中国矫形外科杂志, 1994, (2):118.
[13] Milgram JW. Synovial osteochondromatosis in association with Legg-Calve-Perthes disease[J]. Clin Orthop Relat Res, 1979, (145):179-182.
[14] 纪泉, 郭志斌. 髋关节滑膜软骨瘤病误诊 1 例[J]. 中国骨伤, 2003, 16(7):62.
[15] 康强军, 钱宇航. 髋关节滑膜软骨瘤并股骨头坏死一例报告[J]. 解放军医药杂志, 2004, 16(3):200.
( 本文编辑:李贵存 )
Femoral head necrosis Ficat stage III complicated with synovial chondromatosis: 1 case report
WANG Yakang, QIN Si-qing, JIANG Ren-qi, ZHANG Yu-min. Department of Joint Surgery, Hong-Hui Hospital, Xi’an Jiaotong University College of Medicine, Xi’an, Shaanxi, 710054, China
Objective To investigate the clinical, imaging, pathological features and diagnosis and treatment of the femoral head necrosis combined with synovial chondromatosis.MethodsA patient with femoral head necrosis complicated with synovial chondromatosis was reported. We reviewed the relevant literatures and conducted an analysis.ResultsAccording to the X-rays, CT, MRI fi ndings and clinical manifestations, the patient was diagnosed as femoral head necrosis and was treated with total hip arthroplasty; We found the loose bodies in acetabula with full view. The loose bodies were pathologically diagnosed as synovial chondromatosis. Eventually this patient was diagnosed as femoral head necrosis complicated with synovial chondromatosis.ConclusionsFemoral head necrosis can coexist with synovial chondromatosis. Either of these diseases can also exist independently or appear one after another. Clinical diagnosis should be made based on clinical manifestations, imaging and pathological examinations, so that the correct fi nal diagnosis, and appropriate treatment option can be obtained.
Osteonecrosis; Femur head necrosis; Chondromatosis, synovial; Arthroplasty, replacement, hip; Hip joint
10.3969/j.issn.2095-252X.2017.05.015
R684
陕西省科学技术研究发展计划项目 ( S2014SF4009 )
710054 西安交通大学医学院附属红会医院
张育民,Email: zym2666@163.com
2016-10-09 )
