老年2型糖尿病患者室性期前收缩特点研究
2017-04-10何晓丹吕聪敏杜琼颖田晨光胡云霞
何晓丹,吕聪敏,杜琼颖,田晨光,胡云霞
·论著·
老年2型糖尿病患者室性期前收缩特点研究
何晓丹,吕聪敏*,杜琼颖,田晨光,胡云霞
目的 探讨老年2型糖尿病(T2DM)患者室性期前收缩特点,为临床监测和治疗提供依据。方法 选取2014年3月—2015年9月于郑州大学第二附属医院常规心电图检查发现室性期前收缩的T2DM患者138例为病例组,另选取同期在本院常规心电图检查发现室性期前收缩的体检者102例为对照组。受试者采用同步十二导联动态心电图仪进行24 h监测,记录室性期前收缩发生次数、部位,分析是否出现震荡起始(TO)、震荡斜率(TS)、连续心率减速力(DRs)异常。结果 病例组24 h室性期前收缩>100次为109例(79.0%),对照组为68例(66.7%)。病例组24 h室性期前收缩>100次比例高于对照组(χ2=4.597,P<0.05)。病例组0:00~5:59、18:00~23:59室性期前收缩发生次数高于对照组,6:00~11:59室性期前收缩发生次数低于对照组(P<0.05)。病例组0:00~5:59室性期前收缩发生次数均高于其他时间段(P<0.05)。病例组起源于左心室心尖部的室性期前收缩比例高于对照组,起源于右心室流出道的室性期前收缩比例低于对照组(P<0.05)。病例组TO、TS及DRs异常比例均高于对照组(P<0.05)。结论 老年T2DM患者室性期前收缩更加频繁,尤其在凌晨显著,以起源于左心室心尖部为主,窦性心率震荡(HRT)及DRs异常率增高。
室性早搏复合征;糖尿病,2型;老年人;窦性心率震荡;连续心率减速力
室性期前收缩是2型糖尿病(T2DM)患者最常见的心血管并发症,治疗不当可发展为室性心动过速、心室颤动等恶性心律失常,是导致T2DM患者心源性死亡的主要原因。因此,了解T2DM患者室性期前收缩发生特点对改善其预后有重大意义。T2DM患者频发室性期前收缩与血糖波动、自主神经功能紊乱密切相关,多数研究从室性期前收缩的分布趋势、Lown分级等探讨其特点及临床意义,认为病理性室性期前收缩发生的昼夜变异性明显下降,多发生在睡眠中,但并未对具体时间段室性期前收缩的分布特征进一步研究[1-3],同时,关于T2DM患者不同起源部位室性期前收缩特征研究较少。本研究综合室性期前收缩的发生时间、起源部位等,对T2DM患者并发室性期前收缩的特点进行分析,为临床监测和治疗T2DM患者室性期前收缩提供依据。
1 对象与方法

1.2 方法 受试者采用同步十二导联动态心电图仪(美国DMS有限公司)进行24 h监测,并通过人机对话进行核对校正。室性期前收缩起源部位定位标准[5-6]见表1、图1~4。
窦性心率震荡(heart rate turbulence,HRT)采用震荡起始(turbulence onset,TO)和震荡斜率(turbulence slope,TS)作为检测指标,反映单次室性期前收缩后窦性心率先快后慢的现象。TO<0为正常,即室性期前收缩后早期窦性心率增快;TO≥0为异常,即室性期前收缩后早期无窦性心率增快。TS>2.5 ms/RR间期为正常,即室性期前收缩后窦性心率有减慢现象;TS≤2.5 ms/RR间期为异常,即室性期前收缩后窦性心率无减慢现象[7-10]。
表1 室性期前收缩起源部位定位标准
Table 1 Standards for positioning the original sites of ventricular premature beats
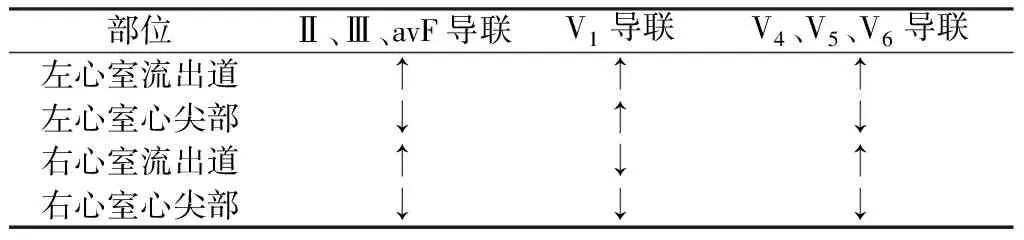
部位Ⅱ、Ⅲ、avF导联V1导联V4、V5、V6导联左心室流出道↑↑↑左心室心尖部↓↑↓右心室流出道↑↓↑右心室心尖部↓↓↓
注:“↑”表示室性期前收缩QRS波主波向上,“↓”表示室性期前收缩QRS波主波向下;起源于左心室的期前收缩V1导联QRS波主波向上,包括qR型、R型、rsR′型、rsr′型、Rs型,若呈rS型,则r波时间应大于S波的50%,振幅大于S波的30%,V2导联呈Rs型;起源于右心室的期前收缩V1导联QRS波主波向下

图1 起源于左心室流出道的室性期前收缩心电图表现
Figure 1 ECG manifestations of ventricular premature beats originating from left ventricular outflow tract

图2 起源于左心室心尖部的室性期前收缩心电图表现
Figure 2 ECG manifestations of ventricular premature beats originating from left ventricular apex

图3 起源于右心室流出道的室性期前收缩心电图表现
Figure 3 ECG manifestations of ventricular premature beats originating from right ventricular outflow tract
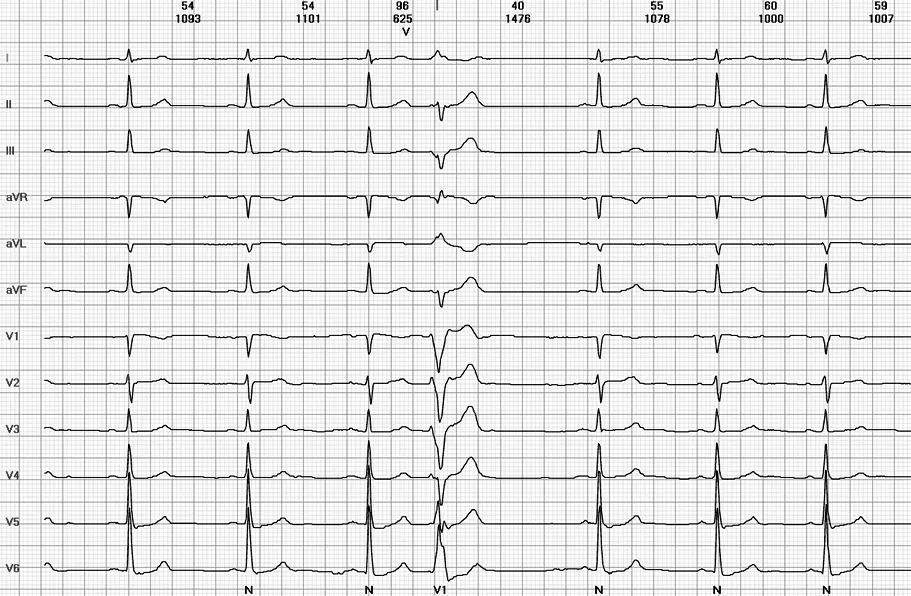
图4 起源于右心室心尖部的室性期前收缩心电图表现
Figure 4 ECG manifestations of ventricular premature beats originating from right ventricular apex
动态心电图中连续RR间期逐渐延长的现象,称为连续心率减速力(heart rate deceleration runs,DRs),反映迷走神经对窦性心率的负性调节作用[11-12]。用DR2、DR4、DR8分别表示连续3、5、9个心动周期中的后2、4、8个连续RR间期延长现象。DR2<5.4%,和/或DR4<0.05%,和/或DR8<0.005%为异常。TO、TS、DRs均由动态心电图仪软件自动分析、计算。

2 结果
2.1 室性期前收缩发生次数 病例组24h室性期前收缩>100次为109例(79.0%),对照组为68例(66.7%)。病例组24h室性期前收缩>100次比例高于对照组,差异有统计学意义(χ2=4.597,P=0.032)。两组12:00~17:59时室性期前收缩发生次数比较,差异无统计学意义(P>0.05)。病例组0:00~5:59、18:00~23:59室性期前收缩发生次数高于对照组,6:00~11:59室性期前收缩发生次数低于对照组,差异有统计学意义(P<0.05)。病例组0:00~5:59时室性期前收缩发生次数均高于其他时间段,差异有统计学意义(P<0.05,见表2)。

Table2Comparisonofventricularprematurebeatsfrequencyatdifferentperiodsbetweentwogroups

组别例数0:00~5:596:00~11:5912:00~17:5918:00~23:59对照组10266±15361±78344±7187±14病例组138414±75278±42a365±71a157±21at值22507550012332321P值<0001000202220023
注:与同组0:00~5:59比较,aP<0.05
2.2 室性期前收缩发生部位 两组室性期前收缩发生部位构成比较,差异有统计学意义(χ2=16.899,P=0.002)。两组起源于左心室流出道、右心室心尖部及其他部位的室性期前收缩比例比较,差异无统计学意义(P>0.05)。病例组起源于左心室心尖部的室性期前收缩比例高于对照组,起源于右心室流出道的室性期前收缩比例低于对照组,差异有统计学意义(P<0.05,见表3)。
表3 两组室性期前收缩发生部位比较〔n(%)〕
Table 3 Comparison of originating sites of ventricular premature beats between two groups

组别例数左心室流出道左心室心尖部右心室流出道右心室心尖部其他对照组10223(225) 3(30) 62(607) 7(69) 7(69) 病例组13830(217)21(152)55(399)17(123)15(109)χ2值002298211028319401131P值08810002000101640288
2.3 TO、TS及DRs异常 病例组TO、TS及DRs异常率均高于对照组,差异有统计学意义(P<0.05,见表4)。
表4 两组TO、TS及DRs异常率比较〔n(%)〕
Table 4 Comparison of abnormal rates of TO,TS,DRs between two groups
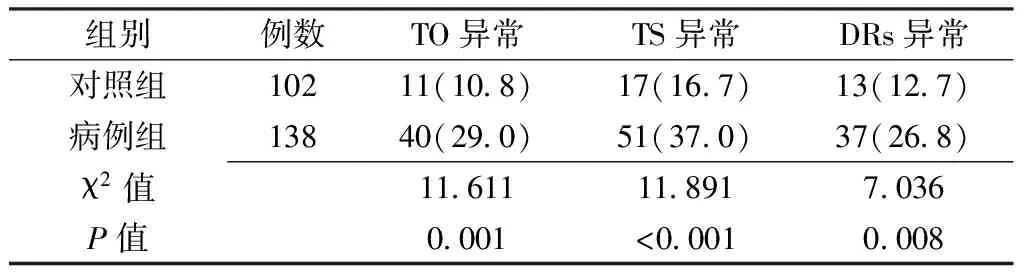
组别例数TO异常TS异常DRs异常对照组10211(108)17(167)13(127)病例组13840(290)51(370)37(268)χ2值11611118917036P值0001<00010008
注:TO=震荡起始,TS=震荡斜率,DRs=连续心率减速力
3 讨论
室性期前收缩是临床常见的心律失常,心肌缺血、电解质紊乱、自主神经功能失调、心功能不全、心肌病、瓣膜病、心力衰竭等均能诱发室性期前收缩[13]。自主神经病变是T2DM最常见的慢性并发症之一,周围神经纤维和自主神经纤维易受不同程度的损害[14-15]。
本研究显示,病例组24 h发生室性期前收缩>100次比例高于对照组,分析原因可能为:(1)长期高血糖引起冠状动脉血管壁增厚变硬,导致心肌细胞缺血缺氧,缺血区心肌细胞发生早期后除极和延迟后除极;(2)除极复极时程不一致,不应期不均一,可在局部形成折返,而折返机制是室性期前收缩产生的主要机制。本研究发现,病例组0:00~5:59室性期前收缩发生次数多于对照组。凌晨时,T2DM患者体内激素水平变化较大,升糖激素水平增高,甚至发生黎明现象,血糖波动幅度大,严重损伤自主神经内皮细胞功能,使细胞因子表达异常,释放更多氧自由基,促进室性期前收缩的发生[1-2]。
本研究显示,对照组起源于右心室流出道的室性期前收缩比例高于病例组,推测应无病理意义[5]。而病例组起源于左心室心尖部的室性期前收缩比例高于对照组,分析原因可能为:(1)长期高血糖引起冠状动脉病变,而冠状动脉病变多数发生在前降支,左心室心尖部主要由前降支供血,并且左心室相对右心室承担的射血负荷更高,耗氧量大,更加重缺血,使室性期前收缩的发生率增高;(2)T2DM患者早期易合并左心室顺应性下降,导致左心室舒张功能降低,且部分老年T2DM患者可能还合并左心室收缩功能不全[16],这些机械性因素可能是引起左心室心尖部室性期前收缩发生率增高的另一原因。
HRT是内源性室性期前收缩刺激触发的反射性调节的结果,反映自主神经对心率的快速调节。HRT常用TO、TS指标表达,两者具有较高的灵敏度和特异度[17]。老年T2DM患者长期血糖水平升高,血液黏滞及体内脂肪代谢紊乱,一定程度上影响神经营养因子的生成,从而影响神经轴索运输功能,导致自主神经功能发生紊乱。迷走神经损害,交感神经活性增强,降低压力感受器的敏感性,使其反应迟钝,致使老年T2DM患者的TO、TS异常率增高。
DRs反映迷走神经对窦性心率的负性调节作用,与死亡风险的预警和危险分层高度相关[12]。本研究发现,T2DM患者DRS异常率增高。长期高血糖引起自主神经功能紊乱,迷走神经功能降低,引起对窦性心律负性频率的调节作用降低,即迷走神经对心率的调控能力下降,使其发生连续减速的现象减弱或消失,导致DRs降低。
综上所述,老年T2DM患者室性期前收缩更加频繁,尤其在凌晨显著,以起源于左心室心尖部为主,HRT及DRs异常率增高。临床应注意监测老年T2DM患者凌晨及左心室心尖部室性心律失常的发生,并根据这些特点,及时控制室性期前收缩的频繁发生,并给予相应治疗。
作者贡献:何晓丹进行文章的构思与设计、统计学处理、结果的分析与解释、撰写论文;吕聪敏进行文章的构思与设计,对文章整体负责,监督管理;杜琼颖、胡云霞进行数据收集、整理;田晨光负责文章的质量控制及审校。
本文无利益冲突。
[1]彭朝胜,草悦鞍,张文洛.老年2型糖尿病患者血糖波动与室性心律失常的关系[J].中国老年学杂志,2011,31(8):1423-1424. PENG C S,CAO Y A,ZHANG W L.The relationship between blood glucose fluctuation and ventricular arrhythmia in elderly patients with type 2 diabetes[J].Chinese Journal of Gerontology,2011,31(8):1423-1424.
[2]PICONI L,QUAGLIARO L,DA ROS R,et al.Intermittent high glucose enhances ICAM-1,VCAM-1 and E-selectin expression in human umbilical endothelial cells in culture:the role of poly(ADP-ribose)polymerase[J].J Thromb Haemost,2004,2(8):1453-1459.
[3]潘玲.频发室性早搏24小时分布的变异性[J].世界最新医学信息文摘(连续型电子期刊),2014(35):158. PAN L.Distribution variability of frequent ventricular premature beat in 24 hours[J].World Latest Medicine Information,2014(35):158.
[4]WHO and IDF Consultation.Definition,diagnosis and classification of diabetes mellitus and its complications,part 1:diagnosis and classification of diabetes mellitus[R].Geneva:Department of Noncommunicable Disease Surveillance,1999.
[5]吕聪敏,张振香.老年常见慢性病患者心脏各部位室性早搏发生率的差异[J].中国慢性病预防与控制,2010,18(1):59-60. LYU C M,ZHANG Z X.Study on the occurrence rates of premature ventricular beats from different original positions of ventricles in common chronic diseases in old people[J].Chinese Journal of Prevention and Control of Chronic Diseases,2010,18(1):59-60.
[6]LÜ C M,ZHANG Z X,LI L,et al.Study on the relationship between myocardial ischemia assessed by 24-hour ambulatory electrocardiogram and ventricular premature beat originating from different positions in older adults[J].European Geriatric Medicine,2012,3(3):153-156.
[7]JUREK S,SREDNIAWA B,MUSIALIK-YDKA A,et al.Heart rate turbulence-a new predictor of sudden cardiac death[J].Pol Merkur Lekarski,2007,23(133):55-59.
[8]FRANCIS J,WATANABE M A,SCHMIDT G.Heart rate turbulence:a new predictor for risk of sudden cardiac death [J].Ann Noninnasive Electrocardiol,2005,10(1):102-109.
[9]BAURE A,MALIK M,SCHMIDT G,et al.Heart rate turbulence:standards of measurement,physiological interpretation,and clinical use:International Society for Holter and Noninvasive Electrophysiology Consensus[J].J Am Coll Cardiol,2008,52(17):1353-1365.
[10]SCHMIDT G,MALIK M,BAREHEL P,et al.Heart-rate turbulence after ventricular premature beats as a predictor of mortality after acute myocardial infarction [J].Lancet,1999,353(9162):1390-1396.
[11]GUZIK P,PISKORSKI J,BARTHEL P,et al.Heart rate deceleration runs for postinfarction risk prediction [J].J Electrocardiol,2012,45(1):70-76.
[12]郭继鸿.猝死预警新技术:连续心率减速力测定[J].临床心电学杂志,2012,21(3):227-233. GUO J H.New technology of sudden death for early warning:determination of continuous heart rate deceleration [J].Journal of Clinical Electrocardiology,2012,21(3):227-233.
[13]魏晓东.充血性心力衰竭合并室性早搏的发生机制[J].医学信息(下旬刊),2010,23(12):92. WEI X D.Pathogenesis of congestive heart failure and ventricular premature beat[J].Medical Information,2010,23(12):92.
[14]RODICA B,BAJKO Z,MAIER S,et al.Influence of risk factors and diabetic complications on peripheral nerve function in type 2 diabetes mellitus[J].Acta Medica Marisiensis,2016,61(1):40-46.
[15]唐键,王博,张玄娥,等.2型糖尿病患者并发糖尿病周围神经病变危险因素分析[J].中国全科医学,2015,18(30):3657-3661. TANG J,WANG B,ZHANG X E,et al.Risk factor for type 2 diabetes mellitus complicated with diabetic peripheral neuropathy[J].Chinese General Practice,2015,18(30):3657-3661.
[16]潘高云,胡元平,尤利益,等.定量组织多普勒技术评价2型糖尿病患者的左室功能[J].实用医学杂志,2012,28(2):229-231. PAN G Y,HU Y P,YOU L Y,et al.Assessment of left ventricular systolic and diastolic function by qantitative tissue velocity imaging in patients with type 2 diabetes mellitus[J].The Journal of Practical Medicine,2012,28(2):229-231.
[17]BISSINGER A,RUXER J,AHMED R B,et al.Heart rate turbulence in patients with poorly controlled diabetes mellitus type 2[J].Arch Med Sci,2014,10(6):1073-1077.
(本文编辑:吴立波)
Features of Ventricular Premature Beats in Elderly Type 2 Diabetic Patients
HEXiao-dan,LYUCong-min*,DUQiong-ying,TIANChen-guang,HUYun-xia
DepartmentofECG,theSecondAffiliatedHospitalofZhengzhouUniversity,Zhengzhou450014,China
*Correspondingauthor:LYUCong-min,Professor,Chiefphysician;E-mail:zzlcmwht@126.com
Objective To analyze the features of ventricular premature beats(VPBs) in elderly type 2 diabetic mellitus(T2DM) patients so as to provide a basis for clinical monitoring and treatment.Methods Of the people underwent routine electrocardiogram(ECG) in the Second Affiliated Hospital of Zhengzhou University from March 2014 to September 2015,we selected 138 elderly T2DM patients and 102 physical examinees who were found with VPBs as the case group and control group,respectively.Both groups were monitored by 12-lead synchronous dynamic ECG for 24 hours.The frequency and original sites of VPBs occurred in both groups were recorded and analyzed to find whether the subjects had abnormal turbulence onset(TO),turbulence slope(TS) and heart rate deceleration runs(DRs).Results The ratio of subjects had more than 100 VPBs within 24 h was higher in the case group than in the control group〔79.0%(109/138) vs.66.7%(68/102),P<0.05〕.Compared with the control group,the case group had more VPBs occurring within 0:00-5:59 and 18:00-23:59,while less VPBs occurring within 6:00-11:59(P<0.05),higher ratio of VPBs originating from left ventricular apex and lower ratio of VPBs originating from right ventricular outflow tract(P<0.05),and higher incidences of abnormal TO,TS and DRs(P<0.05).The case group had more VPBs occurring within 0:00-5:59 than those occurring within 6:00-11:59,12:00-17:59,and 18:00-23:59(P<0.05).Conclusion VPBs occur in elderly T2DM patients more frequently especially in early morning,which mainly originate from the left ventricular apex,and have a higher rate of abnormal HRT and DRs.
Ventricular premature complexes;Diabetes mellitus,type 2;Aged;Heart rate turbulence;Heart rate deceleration runs
河南省郑州市科技局基金资助项目(141PPTGG446)
R 541.7 R 587.1
A
10.3969/j.issn.1007-9572.2017.11.007
2016-08-01;
2016-12-26)
450014河南省郑州市,郑州大学第二附属医院心电图科
*通信作者:吕聪敏,教授,主任医师;E-mail:zzlcmwht@126.com
何晓丹,吕聪敏,杜琼颖,等.老年2型糖尿病患者室性期前收缩特点研究[J].中国全科医学,2017,20(11):1309-1313.[www.chinagp.net]
HE X D,LYU C M,DU Q Y,et al.Features of ventricular premature beats in elderly type 2 diabetic patients[J].Chinese General Practice,2017,20(11):1309-1313.
