Changes of microcirculation in healthy volunteers and patients with septic shock in Xining
2016-06-05SiqingMAShaohuaPENGZongzhaoHEHaoWANGJingyuanXUHaiboQIUXinhuiLiJunmingLUO
Si-qing MA, Shao-hua PENG, Zong-zhao HE, Hao WANG, Jing-yuan XU, Hai-bo QIU, Xin-hui Li, Jun-ming LUO
Changes of microcirculation in healthy volunteers and patients with septic shock in Xining
Si-qing MA1, Shao-hua PENG2, Zong-zhao HE1, Hao WANG1, Jing-yuan XU3, Hai-bo QIU3, Xin-hui Li1, Jun-ming LUO4
1. Department of Intensive Care Unit, Qinghai Provincial People’s Hospital, Xining, 810007, China;
2. Department of Pathology, Medical College of Hunan Normal University, Changsha, Hunan 410013, China;
3. Department of Intensive Care Unit, Zhongda Hospital of Southeast University, Nanjing, 210009, China;
4. Department of Pathology, Qinghai Provincial People’s Hospital, Xining, 810007, China
Objective:The purpose of this study is to investigate the characteristic of microcirculation in healthy volunteers and pati ents with septi c shock in both Xining (2 260 m) and Nanjing (10 m).Methods:A total of 62 cases, 33 healthy volunteers, 22 cases in Xining, (2 260 m above sea level) and 11 cases in Nanjing (10 m above sea level); and 29 septi c shock, 13 cases in Xining and 16 cases in Nanjing were collected. The total vessel density (TVD), perfused vessel density (PVD), proporti on of perfused vessel (PPV) and microcirculati on fl ow index (MFI) of both healthy volunteers and septi c shock had been investi gated by using sidestream dark fi eld (SDF). Analyzed and managed the image data by using AVA3.0 soft ware.Results:In the healthy volunteers in Xining area (22 cases),the volume of TVD (15.59 ± 2.58 mm/mm2), PVD (15.58 ± 2.58 mm/mm2) and PPV(96.60% ± 4.63%) were signifi cant higher than the volume of TVD (10.0 ± 2.10 mm/ mm2), PVD (10.81 ± 2.38 mm/mm2) and PPV (84.24% ± 8.00%) of the volunteers (11 cases) in Nanjing (11 cases). But the MFI (2.17 ± 0.31) of the healthy volunteers in the Xining was signifi cant lower (P<0.05) than the MFI (3.21 ± 0.34) in the healthy volunteers of Nanjing. In the septi c shock group (13 cases) in the Xining, the volume of TVD (5.44 ± 1.94 mm/mm2), PVD (4.18 ± 1.61 mm/mm2), PPV (42.14%± 5.38%) and MFI (1.05 ± 0.32) compared with the volume of the healthy volunteers in Xining, the TVD (15.59 ± 2.58 mm/mm2), PVD (5.58 ± 2.58 mm/mm2), PPV (96.60% ± 4.63%) and MFI (2.17 ± 0.30) were signifi cant lower (P<0.05). In the healthy volunteers compare with septi c shock group in Nanjing area, the TVD(6.80±1.72 vs 10.00±2.10, P<0.05), PVD(5.86±1.58 vs10.81±2.38,P<0.05), PPV(45.42±4.86 vs 84.24±4.86, P<0.05), MFI(1.28±0.28 vs 3.21±0.34 P<0.05), there was signifi cant decreased. In the septi c shock group in the Xining compared with the septi c shock in Nanjing, there was no signifi cant diff erence. 10 of 13 pati ents with septi c shock were survived in Xining. 13 of 16 pati ents with septi c shock were survived in Nanjing.Conclusion:The changes of physiological and pathophysiological characteristi c in microcirculati on induced by hypoxia would be useful for clinical treatment of septi c shock at high alti tude.
hypoxia; high alti tude; microcirculati on; septi c shock; healthy volunteers
Introduction
Xining is located in the Qinghai-Tibet plateau, with an average elevation 2 260 meters. Th e atmospheric pressure is 585 mmHg, oxygen partial pressure is 121 mmHg, and the healthy person arterial blood oxygen partial pressure is only 70 mmHg. Longterm low oxygen environment can lead red blood cell proliferation, slow blood stream. In order to meet the exchange of oxygen and nutrients, human body must increase vascular density which can result in proliferation of microcirculation. Septic shock issevere and microcirculation dysfunction. The main cause is multiple organ dysfunctions. In the healthy volunteers, the microcirculation was significantly diff erent in Xining region compared with the people living in plain area. Th e change and its physiological characteristics are significant impact the therapy of septic shock. To improve the survival rate of the treatment of septic shock in Xining region, the further study the characteristic of high altitude is necessary [1].
Sidestream dark fi eld imaging (SDF) technology is a new generation of microcirculation imaging equipment which has multiple advantages such as imaging clearly, noninvasive, portable, visual and semi-quantitative analysis etc. So it can make real time monitoring of superfi cial tissue microcirculation perfusion characteristics in bed [2]. In this study, we observed the characteristics of sublingual microcirculation of healthy people and patients with septic shock in both Xining and Nanjing area by using SDF monitoring technique. The purpose is to investigate its mechanism of microcirculation, and explore to set a possible guidance for clinical treatment of septic shock in high altitude region.
Subjects and Methods
Subjects
Informed consent was signed by all subjects (including healthy volunteers and septic shock patients) from both Xining Area and Nanjing Area. The study has been approved by ethics committee in Southeast University and in Qinghai Provincial People's Hospital. In Nanjing area, we investigated a total of 11 cases of healthy volunteers and 16 cases of septic shock patients; in Xining area, we investigated a total of 22 cases of healthy volunteers and 13 cases of septic shock patients. The basic information including age, gender, Acute Physical and Chronic Healthy Score II (APACHE II) had been enrolled in Table 1.
Inclusion criteria
Inclusion criteria for healthy volunteers
Age 20-60 years old, no any basic diseases, living in Xining area or Nanjing area 20 years or more, no alternate in plateau and plain.
Septic shock inclusion criteria
Follow to the reference [3] According to current guidelines, requirements for diagnosis with sepsis are the presence (probable or documented) of infection together with systemic manifestations of infection [4] . These manifestations may include: Tachypnea (high respiratory rate), which is defined as more than 20 breaths per minute, or when testing blood gas, a PaCO2less than 32 mmHg, which signifies hyperventilation. White blood cell count was either significantly low (< 4 000 cells/mm3) or high (> 12 000 cells/mm3). Tachycardia (rapid heart rate) is defined as a rate greater than 90 beats per minute. Altered body temperature: Fever > 38.0°C or hypothermia < 36.0°C.
Exclusion criteria
Pregnancy; age<20 years; inability to acquire the usual level of MAP; refusal of consent by the patient or relative; and had another trial within last 3 months.
Methods
Blood cell parameter determination
Th e WBC, RBC, HB, HCT, PLT were detected by using Sysmex XE-2100 (Sysmex, Japan).
Clinical data collection
Heart rate(HR), arterial blood pressure (ABP) were performed by Phillip MP50 monitor(The Netherland, Phillip), and arterial partial pressure of oxygen (PaO2), lactic acid were determined by bloodd gas analyzer (Prismer 3000, USA).
Microcirculatory measurements and analysis
The sublingual microcirculation were measured by using Sidestream dark field (SDF; MicroScan, Microvision Medical, Amsterdam,The Netherlands). Th e SDF probe was placed under the sublingual area without pressure after removal of secretions. Video sequences of 20 seconds were recorded from three different sublingual sites [5]. These images were stored and later renumbered by an identifier who was blinded to the trial [6]. Videos were converted to audio video interleaved (AVI) fi le format with video processing software (Automated Vascular Analysis 3.0, Academic Medical Center, Amsterdam, The Netherlands), and analysis for each image was performed by two diff erent investigators. Finally, all the variables were averaged to yield a single value for statistical analysis.
Based on the principle, the density of the vessels is proportional to the number of vessels crossing arbitrary lines. The measurement variables including vascular density, proportion of perfused vessels andperfused vessel density was recorded by De Backer score [7]. Large (mostly venules) and small (mostly capillaries) vessels were separated by a cut-off value of 20μm in diameter. Three equidistant horizontal and three equidistant vertical lines were drawn on the screen. Defi ned as the number of vessels crossing these lines divided by the total length of the lines, the vascular density was calculated. Th e type of fl ow was defined as no flow, intermittent, sluggish, and continuous. Vessel perfusion was categorized visually as continuous (continuous flow for at least 20 seconds), sluggish (decreased but continuous flow for 20 seconds), intermittent (no flow for less than 50% of the time), no fl ow (no fl ow for at least greater than or equal to 50% of the time). The proportion of perfused vessels was calculated as follows: 100 × (total number of vessels – no fl ow –intermittent fl ow) / total number of vessels. As an important variable with the greatest infl uence on perfusion [6], perfused vascular density was calculated by multiplying vessel density by the proportion of perfused vessels.
The microcirculatory flow index (MFI) based on determination of the predominant type of flow in four quadrants for small vessels and total vessels were determined with a semi-quantitative methodology. Flow was characterized as no fl ow = 0, intermittent = 1, sluggish = 2, continuous = 3 to refl ect blood velocity. Th e types of fl ow were identical to that described in consensus conference recommendations [6]. MFI was calculated for all quadrants of the image and averaged for each sublingual site.
Septic shock treatment
Effective primary disease therapy; using sensitive antibiotics as soon as possible; and follow SSC guidelines, including early liquid target therapy, vascular active drug application, viscera function support [8] [9].
Statistical analysis
Statistical analysis of the data was performed by using SPSS 18.0 (IBM,Somers,NY,USA) statistical soft -ware. Data is presented as the mean ± standard deviation (x±s), comparison between the groups by using independent sample t-test, count data (CFR) X2test, P < 0.05 for the diff erence was statistically signifi cant.
Results
The basic information of healthy volunteers and patients with septic shock
We collected a total of 62 cases. Th ere are a total 33 cases in healthy group, 22 cases from Xining, and 11 cases from Nanjing. Th ere are a total of 29 cases in shock group, 13 cases from Xining, and 16 cases from Nanjing. The causes of septic shock were pulmonary infection, abdominal infection, bacteremia, and urinary tract infection, etc. Twenty-three cases alive, and 6 cases died (in Xining 3 cases, in Nanjing 3 cases), as shown in table 1. The survival rate was significant difference between the Xining and Nanjing. There was lower survival rate in Xining area than the patients in Nanjing (P<0.05).
Changes of blood routine parameters
In the healthy volunteers of Xining area, the number of WBC was (6.03±1.16×109/ L), RBC (4.95±0.42 ×1012/ L), HGB (150.59 ±13.97 g/L),HCT (%) of 49.30±2.78; in Nanjing area, the volume of WBC (3.83±0.45×109/L),RBC(3.83±0.45×1012/ L), HGB (138.81±9.10 g/L), HCT (%)46.34±2.52. There are signifi cant higher in Xining area than the healthy volunteers of Nanjing area (P<0.05), while PLT is lower in Xining area than in the healthy volunteers of Nanjing area (205.27±48.28 vs266.54± 42.95)(P<0.05). In Xining shock group, the number of WBC are signifi -cantly increased than the healthy volunteers group in Xining healthy volunteers (15.03±1.29 vs 6.03± 1.16, P<0.05); while RBC, HGB, HCT, PLT are significantly decreased than the healthy volunteers group in Xining, respectively as (4.14±0.57 vs 4.95±0.42, 124.38±12.35 vs150.59±13.97, 42.91±3.25 vs 49.30± 2.78, 170.92±41.38 vs 205.27± 48.28, P<0.05). In Xining shock group of RBC (×1012/L) (4.14±0.57 vs 3.29±0.44, P<0.05) was signifi cant increased than the shock group of Nanjing; while the PLT (×109/ L) signifi cantly decreased in septic shock of Xining area than the septic shock of Nanjing area (170.92±41.38 vs 224.37± 37.86, P<0.05). Th e remaining indicators are no signifi cant diff erence. Th e results are shown in table 2.
Changes of hemodynamic, oxygenation parameters, lactic acid
The heart rate in both Nanjing and Xining area of healthy volunteers was decreased significantly (P<0.05) compared with shock group. The heart rate in Xining area of healthy volunteers was also significantly lower than the Nanjing healthy volunteers (P<0.05). While there was no significant difference between the two septic shock groups of Nanjing and Xining (P>0.05). The PaO2in healthy volunteers both Nanjing and Xining area were significantly increased compared with Nanjing andXining shock group (P<0.05).The PaO2in Xining shock group was significantly decreased than Nanjing shock group(P<0.05). The lactic acid in healthy volunteers group both Nanjing and Xining were significantly reduced (P<0.05) than the septic shock groups in both Nanjing and Xining area, but there was no signifi cant diff erence between Nanjing and Xining shock groups (P>0.05).The heart rate, arterial blood pressure, blood gas index changes of healthy volunteers and septic shock in Xining area and Nanjing area, as shown in table 3.
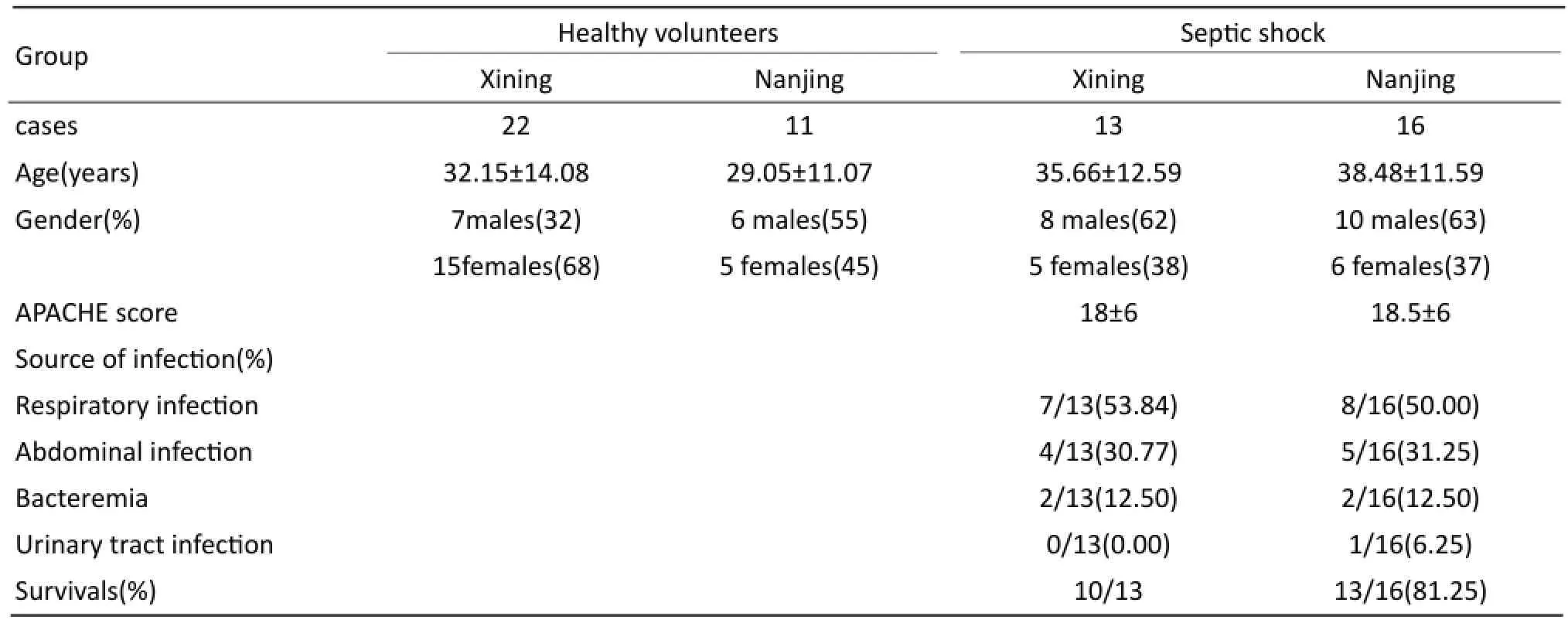
Tab. 1 The basic information of healthy volunteers and patients with septic shock.

Tab. 2 Changes in blood routine parameters of healthy volunteers and patient with septic shock in Xining.
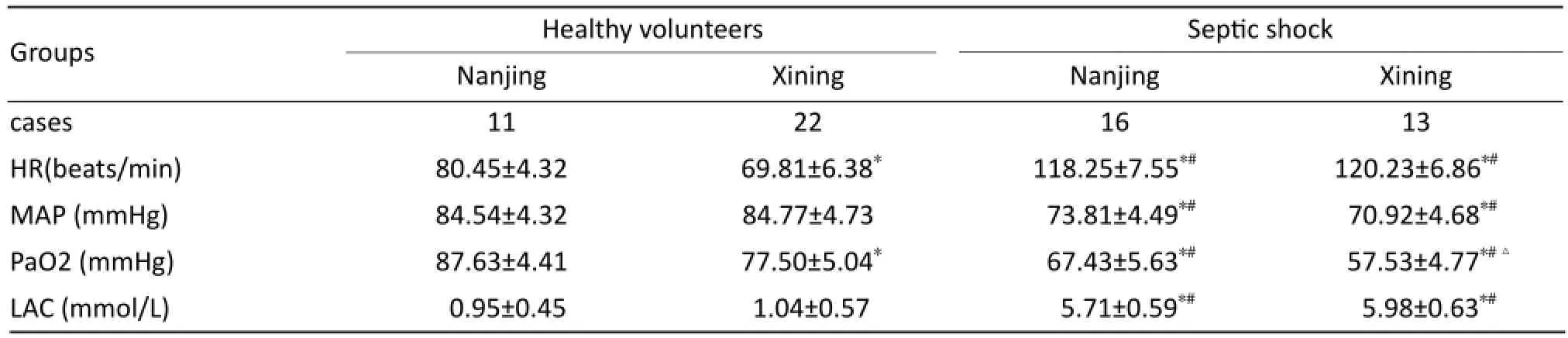
Tab. 3 Changes in HR, MAP, PaO2lactate variable of healthy volunteers and patients with septic shock in Xining.
Th e microcirculation characteristics
Th e change of healthy volunteers and septic shock in Xining area and Nanjing area, as shown in Figure1. In healthy volunteers group compared with septic shock group, the TVD were signifi cantly higher in healthy volunteer groups in both Nanjing and Xining area than the shock groups in both Nanjing and Xining area (P<0.05), but there was no signifi cant diff erencebetween the two shock groups (P>0.05). Th e PVD in healthy volunteers group was signifi cant higher than the shock group in both Nanjing and Xining. The PVD in Xining healthy volunteers was also increased signifi cantly (P< 0.05) than healthy volunteers group of Nanjing, but there was no significant difference between the two shock groups (P>0.05). In healthy volunteers group in Xining compared with the healthy volunteers group in Nanjing, the TVD in Xining area was significantly increased (P<0.05), but there was no significant difference between the two shock groups (P>0.05). Th e TVD in Xining area normal healthy group was also signifi cantly increased (P<0.05) compared with Nanjing normal, but there was no signifi cant diff erence between the two shock groups (P>0.05).The PVD in healthy volunteers group was signifi cant increased than shock group in both Nanjing and Xining.

Fig. 1 The microcirculation characteristics and change of healthy volunteers and septic shockin Xining area and Nanjing area,*P<0.05 vs Najing Healthy volunteers;#P<0.05 vs Xining Healthy volunteers;△P<0.05 vs Nanjing Septic shock.

Fig. 2 The image of dark field imaging (SDF). A: Plateau healthy volunteers, male, 48, vascular density is plain; B: Plain healthy volunteers; C: Display capillary density decreases, perfusion small blood vessels proportion reduced; D: Show each part blood perfusion imbalance.
In healthy volunteers group of Xining compared with the healthy volunteers group of Nanjing, the MFI in Xining area healthy group was significantly increased (P<0.05),but there was no significant difference between the two shock groups (P>0.05).
Th e image of dark fi eld imaging (SDF). Figure 2A showed plateau healthy volunteers, male, 48, vascular density is plain. Figure 2B showed plain healthy volunteers, figure 2C displayed capillary density decreases, perfusion small blood vessels proportion reduced, fi gure 2D showed each part blood perfusion imbalance.
Discussion
Microcirculation refers to the micro artery and vein between the microvascular (< 100 microns in diameter) of the blood circulation, is mainly composed of micro arterioles, capillaries, veins.Microcirculation is the most basic structure and terminal circulation system which is the material exchange between blood and tissue smallest unit of function. A good microcirculation perfusion is the foundation of material metabolism [10]. Septic shock is a major cause of death in critically patients and is characterized hypotension and hypoperfusion [11]. Microvascular dysfunction is associated with organ dysfunction and mortality [12] [13].
In plateau area, the low oxygen environment can lead to low arterial blood oxygen partial pressure (PaO2) and arterial blood oxygen saturation (SaO2) which can directly lead to the change of the capillary number and damage capillary wall of healthy volunteers. Increasing the number of the microcirculation is the easiest way for body’s response to hypoxic [14]. Th e mechanism of change is obviously increased the number of red blood cells under hypoxic condition under low arterial blood oxygen partial pressure. Th is study shows that the arterial blood oxygen partial pressure is signifi cantly reduce, and the number of red blood cells is signifi cantly increased in Xining area compared in plain of Nanjing area. The capillaries indexes of TVD, PVD, and PPV are significantly increased; while MFI is significantly reduce in Xining area of healthy volunteers compared with in plain of Nanjing area. The physiological significance of vascular density increased refl ected that was more exchange area between capillaries and organs to meet the physiological state of oxygen and energy requirements. Although our observation is focused on healthy normal person, the results were as similar as the radical plateau of healthy people. As Martin reports [15], 24 cases of healthy volunteers from sea level climbing to an altitude of 5 300 m plateau, 10 cases left , and the other 14 cases continued to a higher altitude (6 400 m). Th e results showed that MFI in small blood vessels (< 25 μm, P<0.0001), and middle vascular (26~50 μm, P=0.006) were significant decreased compared with the sea level. The MFI in small blood vessels (< 25 μm) and middle vascular (26~50 μm) were signifi cant decreased (P= 0.017 and P= 0.002) in higher elevation compared with 5 300 m. Number of small blood vessels (<25 μm) and middle vascular number (26~50 μm) were reduced, respectively from 2.8 to 2.5, and 2.9 to 2.4. Although the density of small blood vessels (<25 μm) in our group have no obvious increase, but middle vascular (26~50 μm) are signifi cantly increased (1.68±0.43 mm/mm2vs 2.27±0.57 mm/mm2, P= 0.005). Th e vascular density in other high altitude was also increased (P<0.01).
Twenty-four subjects were studied using sidestream dark-field imaging, as they ascended to 5 300 m; one cohort remained at this altitude(n=10) crossings (GX; an alternative density measure) were calculated. Total study length was 71 days; images were recorded at sea level(SL), Namche Bazzar (3 500 m), Everest base camp(5 300 m), the Western Cwm (6 400 m), South Col (7 950 m) and departure from Everest base camp(5 300 m). Perioheral oxygen saturation (SpO2), heart rate and blood pressure were also recorded. Compared with SL, altitude resulted in reduced sublingual MFI in small(<25 μm;P<0.01) and medium vessels(26~50 μm;P=0.006). Th e greatest reduction in MFI from SL was seen at 5 300 m; from 2.8 to 2.5 in small vessels and from 2.9 to 2.4 in medium-sized vessels. The density of vessels <25 μm did not change during ascent, but those >25μm rose from 1.68(±0.43)mm mm-2 at SL to 2.27(±0.57) mm/mm2at 5 300 m (P=0.05); GX increased at all attitudes(P<0.01). The reduction in MFI was greater in climbers than in those who remained at 5 300 m in small and medium-sized vessels (P=0.017 and P=0.002, respectively). At 7 950 m, administration of supplemental oxygen resulted in a further reduction of MFI and increase in vessel density. Th us, MFI was reduced whilst GX increased in the sublingual mucosa with prolonged exposure to hypoxia and was exaggerated in those exposed to extreme altitude.
Under hypoxic condition, the main mechanism of capillary proliferation is overexpression capillary endothelial expression factor (vascular endothelium growth, VEGF) due to the low oxygen stimulating blood vessel [16].The microcirculation compensatory can provide the bigger exchange area which benefi t both physiology signifi cance and the material exchange. In the pathological state, more number of blood vessels may increase material exchange energy, maximum satisfy the pathological state of energy supply of materials. In the meanwhile, capillary hyperplasia, high density of blood vessels and more number of capillaries may be potential harmful factors under the severe hypoxia, infection, shock, pathological factors, and capillary leak syndrome [17]. Under physiological state, the highlander obviously has more number of capillary. Th e patients of plateau septic shock need more treatment fl uid (liquid recovery) than the patients of plain areas septic shock due to high density capillary in high altitude. Th is may be a characteristic of fl uid resuscitation in plateau septic shock. At the same time, because the capillary hyperplasia in the plateau serious blood capillary leakage may occur in septic shock which may lead insufficient blood volume. The shock inhighland is more serious than the patients in plain. Studies on the diff erence of septic shock between altitude and plain are still less, deserve further research.
Like small vessel number increase, MFI obviously reduced with the increase of altitude, has its physiological and pathological significance. The hemoglobin is significant increase the healthy volunteers in Xining than the healthy volunteers in plain area which may be the main cause of leading to a less MFI. MFI reduction indicates that slow blood fl ow in microcirculation fl ow, convenience to increase material exchange between red blood cells and surrounding tissues which is another one of the mechanisms of human adaptation plateau [18]. At the same time, slow blood fl ow velocity is easy to cause blood clots, thrombosis, and promote the disseminated intravascular coagulation (DIC),more aggravating microcirculation dysfunction [19].
This study showed that the microcirculation was significant different when septic shock occurred on in both residents of Plains and Xining area. The TVD, PVD, PPV, MFI declined obviously, in septic shock of Xining area decreased more obvious, but has no obvious statistical signifi cance compared with plain area. Th is change can lead to tissue hypoperfusion, microcirculation function failure can aggravate the organ dysfunction and increased mortality [20]. How capacity distribution in shock in plateau area, how to make the liquid recovery and the regulation of microcirculation, may be research issues in the future.
Acknowledgements
Fund programe Qinghai provincial (application) basic research project (2012-YJ-2933) and Qinghai province natural science foundation of China (2016-ZJ-905).
1. Wu TY. Th e Qinghai-Tibetan plateau: how high do Tibetans live[J]? High Alt Med Biol, 2001, 2(4): 489-499.
2. Ince C. Sidestreamdark field imaging: An improved technique to observe sublingual microcirculation[J]. Crit Care, 2005, 9(5): 72.
3. Ma SQ, Wu TY, Zhang XF, et al. Acute severe high altitude disease and multiple organ dysfunction syndrome[J]. PEOPLE’S MEDICAL PUBLISH HOUSE, BEI JING, 2014, 12.
4. Levy MM, Fink MP, Marshal IE, et al. SCCM/ESICM/ ACCP/ATS/SIS international Sepsis Defi nitions Conference. Crit[J]. Care Med, 2003, 2001: 1250-1256.
5. Morelli A, Donati A, Ertmer C, et al. Microvascular eff ects of heart rate control with esmolol in patients with septic shock: a pilot study[J]. Crit Care Med, 2013, 41(9): 2162-2168.
6. De Backer D, Hollenberg S, Boerma C, et al. How to evaluate the microcirculation: report of a round table conference[J]. Crit Care, 2007, 11(5): R101.
7. De Backer D, Creteur J, Preiser JC, et al. Microvascular blood fl ow is altered in patients with sepsis[J]. Am J Respir Crit Care Med, 2002, 166(1): 98-104.
8. Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock[J]. N Engl J Med, 2001, 345(19): 1368-1377.
9. Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock[J]. Crit Care Med, 2013, 41 (2): 580–637.
10. Ince C. Th e microcirculation is the motor of sepsis[J]. Crit Care, 2005, 9(suppl 4): S13~S19.
11. Angus DC, van der poll T. Severe sepsis and septic shock[J]. N Engl J Med, 2013, 369(21): 840-851.
12. Xu JY, Ma SQ, Pan C, et al. A high mean arterial pressure target is associated with improved microcirculation in septic shock patients with previous hypertension: a prospective open label study[J]. Crit Care , 2015, 19: 130.
13. Hernandez G, Boerma EC, Dubin A, et al. Severe abnormalities in microvascular perfused vessel density are associated to organ dysfunctions and mortality and can be predicted by hyperlactatemia and norepinephrine requirements in septic shock patients[J]. J Crit Care, 2013, 28(4): 538.
14. Ma SQ, Wu TY, Cheng Q, et al. Acute respiratory distress syndrome secondary to high-altuitude pulmonary edema: A diagnostic study[J]. J Med Lab Diagn, 2013, 4(1): 1-7.
15. Daniel SM, Goedhart P, Vercueil A, et al. Changes in sublingual microcirculatory flow index and vessel density on ascent to altitude[J]. Exp Physioly, 2010, 95(8): 880-891.
16. van der Flier M, van Leeuwen HJ, van Kessel KP, et al. Plasma vascular endothelial growth factor in severe sepsis[J]. Shock, 2005, 23(1): 35-38..
17. Hackett PH, Roach RC. High-altitude illness[J]. N Engl J Med, 2001, 345(2): 107-114.
18. Penaloza D, Arias-Stella J. The heart and pulmonary circulation at high altitudes: healthy highlanders and chronic mountain sickness[J]. Circulation, 2007, 115(9): 1132-1146. 19. Edul VS, Enrico C, Laviolle B, et al. Quantitative assesment of the microcirculation in healthy volunteers and in patients with septic shock[J]. Crit Care Med, 2012, 40(5): 1443-1448. 20. De Backer D, Creteur J, Preiser JC, et al. Microvascular blood fl ow is altered in patients with sepsis[J]. Am J Respir Crit Care Med, 2002, 166(1): 98-104.
doi 10.13459/j.cnki.cjap.2016.06.011
Hai-bo QIU, MD, Professor, Department of intensive care unit, Zhongda Hospital of Southeast University, Nanjing 210009, China. E-mail: haiboq2000@163.com. Jun-ming LUO, Department of Pathology, Qinghai Provincial People’s Hospital, Xining 810007, China. E-mail: jluo099@163.com.
2016-09-26; accepted 2016-11-16
杂志排行
中国应用生理学杂志的其它文章
- 5-HT1B受体亚型对小脑顶核介导的运动行为的影响*
- Iptakalim ameliorates relaxation to acetylcholine in thoracic aortic rings impaired by microvesicles derived from hypoxia/ reoxygenation-treated HUVECs
- Association study between the angiotensin converting enzyme gene insertion/deletion polymorphism and Qinghai Han Chinese with congenital heart disease
- The infl uence of heterogeneity on the analysis of sleep-wake architecture in the single-prolonged stress rats
- Effect of creatine phosphate sodium on miRNA378, miRNA378* and calumenin mRNA in adriamycin-injured cardiomyocytes
- 当归黄芪提取物对慢性腹膜功能衰竭大鼠腹膜功能、结构及TGF-β1表达的影响*
