肝癌射频消融术与切除术分别联合脾切除治疗小肝癌伴脾亢进临床疗效对比分析
2016-03-01朱海林
朱海林
(宝鸡市中心医院肝胆外科,陕西 宝鸡 721000)
肝癌射频消融术与切除术分别联合脾切除治疗小肝癌伴脾亢进临床疗效对比分析
朱海林
(宝鸡市中心医院肝胆外科,陕西 宝鸡721000)
摘要:目的比较肝癌射频消融术与切除术分别联合脾切除治疗小肝癌伴脾亢进临床疗效。方法127例小肝癌伴脾亢进患者根据患者手术方式分为射频消融组(n=62)和手术切除组(n=65),射频消融组患者采取肝癌射频消融术联合脾切除术,手术切除组患者采取手术切除术联合脾切除术。记录两组患者手术一般情况,比较两组患者术后12个月并发症发生情况,所有患者随访截止到2015年2月,比较两组患者术后1、3和5年生存情况,以及无肿瘤生存情况。结果射频消融组患者热缺血时间、手术时间和住院时间均短于手术切除组,术中失血量和输血量均少于手术切除组,差异均有统计学意义(P<0.05);射频消融组患者术后12个月总并发症发生率6.4%,显著低于手术切除组的41.5%,差异有统计学意义(P<0.05);射频消融组患者术后1、3、5年生存率分别为99.5%、74.8%和71.4%,手术切除组分别为96.9%、68.2%和66.3%,两组相比差异无统计学意义(P>0.05),射频消融组患者术后无肿瘤生存中位时间29.3个月,长于手术切除组的26.7个月,但差异无统计学意义(P>0.05)。结论射频消融联合脾切除术治疗小肝癌伴脾亢进,与手术切除联合脾切除术治疗效果相当,且可有效减少术后并发症发生,有利于患者术后恢复。
关键词:小肝癌;脾功能亢进;射频消融术;手术切除术;脾切除术
小肝癌是肝胆外科常见的肝癌类型,我国每年约有11万人死于该病[1],由于我国小肝癌患者常合并有肝炎肝硬化门脉高压,因此,常伴有脾功能亢进[2],临床上在对患者进行手术治疗时,在切除肝癌组织的同时需将脾脏切除,但该手术操作风险较大,且患者术后并发症较多,影响了患者预后[3]。近年来,随着射频消融术在临床的应用,其在局灶性肿瘤治疗方面的疗效已得到临床认可[4]。本研究对合并有脾功能亢进的小肝癌患者进行射频消融术联合脾切除治疗,并与手术切除术联合脾切除进行比较,探讨该方法临床应用效果及优缺点,以期为临床实践提供基础资料。
1资料与方法
1.1一般资料选取2007年1月至2011年1月在我院肝胆外科择期行手术治疗的小肝癌伴脾亢进患者127例,其中,男性53例,女性74例,年龄(51.7±4.1)岁,病例纳入标准:(1)原发性肝癌诊断标准,存在慢性乙肝或丙肝,出现肝硬化,影像学检查有两项出现典型原发性肝癌征象,或有一项出现典型原发性肝癌征象且AFP≥200 μg·L-1,若不满足上述条件,则行穿刺活检病理证实;(2)肿瘤直径≤3.0 cm,且数量≤3个;(3)影像学检查未发现出现肝门静脉系统血栓;(4)Child-Pugh分级A或B级;(5)未发生远处转移,无梗阻性黄疸,重要脏器无严重功能障碍;术前脾脏出现Ⅱ度肿大。同时排除严重凝血功能障碍者、Child-Pugh分级C级者,以及临床资料不全者。所有入选患者既符合射频消融术又符合手术切除术治疗,在患者及家属知情同意基础上,由患者及家属选择手术方式,根据患者手术方式分为射频消融组和手术切除组,其中,射频消融组62例,男性26例,女性36例;手术切除组65例,男性28例,女性37例。
1.2方法两组患者术前均完善各项检查,均采取相同的术前准备。手术均行双侧肋缘下切口,对腹腔和肝癌等情况进行观察。手术切除组:所有患者行肝癌切除术联合脾切除术,患者在切除脾脏后,对肝脏相邻韧带进行游离,用钳夹的方法对肝癌组织进行手术切除。射频消融组:所有患者行肝癌射频消融术联合脾切除术,在对脾脏进行手术切除后,利用冷循环射频消融治疗系统(购自美国Cool-tipTM)于术中对肝癌组织行射频消融治疗。在超声引导下进行穿刺入肝癌组织后界0.5~1.0 cm,将冷循环泵打开,让冰纯水流动于针体内使针尖温度维持在15~25 min,设定功率在90~120 W,进行自动射频消融12~15 min。之后将冷循环关闭,对针道加热到90℃以上,使针道损毁,将冷循环电极拔除。对于位于肝脏表明的肿瘤,尽量在入电极单针时保证经过一定厚度的肝组织,功率调整过程要由小到大,以防止发生肝癌细胞腹腔播散。术后2 d开始,每12 h将4 250~4 500 U低分子肝素钙于皮下注射1次,连续进行7~14 d。出院后患者持续进行3~6月口服阿司匹林治疗。
所有患者术后28 d进行增强CT复查,对于术后完全消融的患者,在前2年随访中,每3~4月进行增强CT复查,均对肝功能、AFP、血常规和门静脉进行检查,每半年进行一次胸片复查。术后随访超过2年的,每6个月进行一次随访。
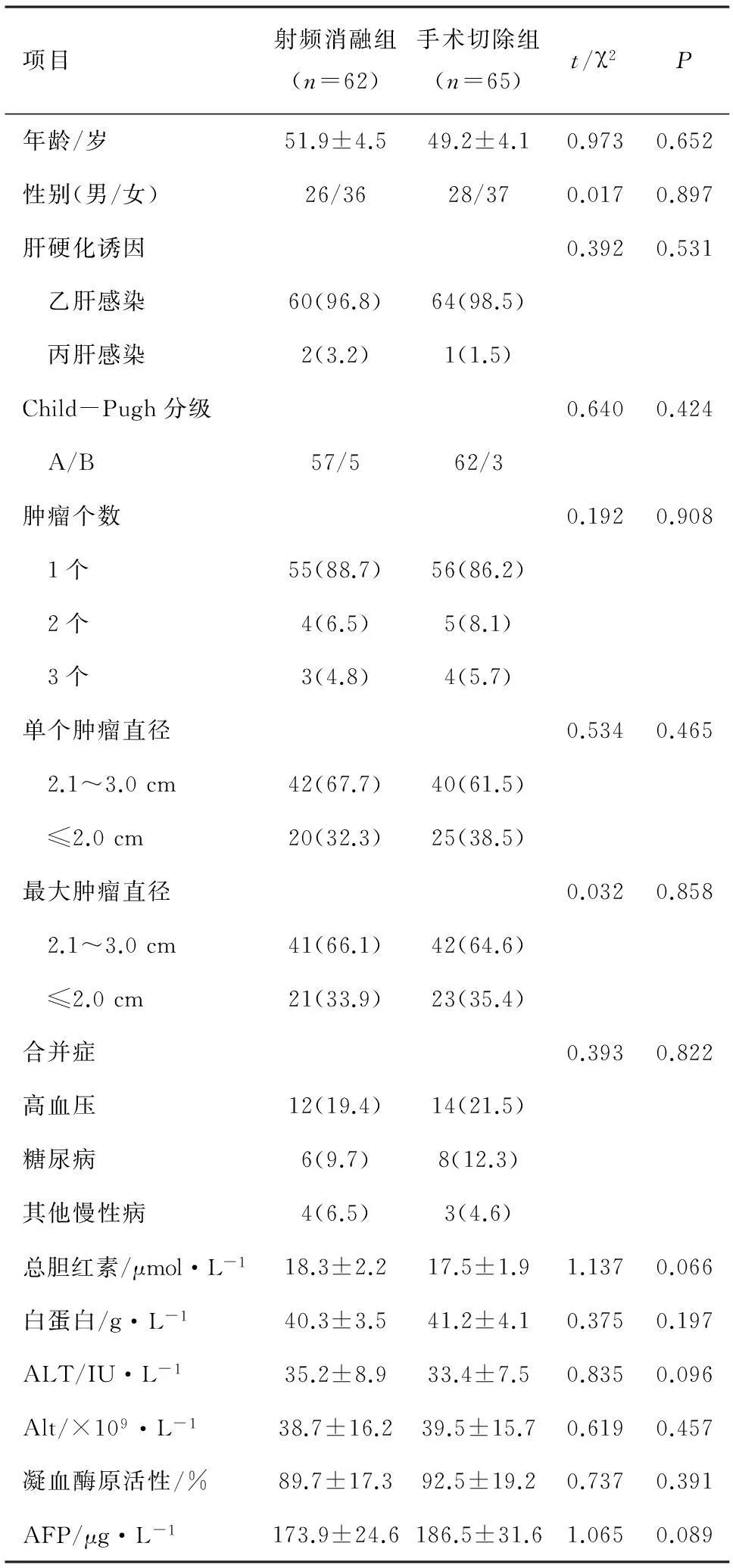
表1 两组患者一般临床资料比较
1.3评价指标记录两组患者手术一般情况、住院时间等,以及患者术后12个月并发症发生情况,所有患者随访截止到2015年2月,比较两组患者术后1、3和5年生存情况,以及无肿瘤生存情况。
1.4统计学处理利用SPSS21.0统计分析软件进行统计学处理,计量资料采用均值±标准差表示,组间比较采用t检验,计数资料采用率值表示,组间比较采用χ2检验,两组生存时间的比较采用Log Rank检验,P<0.05差异有统计学意义。
2结果
2.1两组患者临床一般情况比较两组患者临床一般资料相比差异均无统计学意义(P>0.05),见表1。
2.2两组患者手术一般情况比较射频消融组患者热缺血时间、手术时间和住院时间均短于手术切除组,术中失血量和输血量均少于手术切除组,差异均有统计学意义(P<0.05),详见表2。
2.3两组患者术后12个月并发症发生情况射频消融组患者术后12个月总并发症发生率6.4%,显著低于手术切除组的41.5%,差异有统计学意义(P<0.05);两组患者术后有8例出现早期出血,利用可吸收止血纱布进行处理后停止出血;4例胆漏患者经过引流处理后自行闭合;10例胸腔积液患者经穿刺抽吸后缓解;10例顽固性腹水患者经引流后缓解,详见表3。
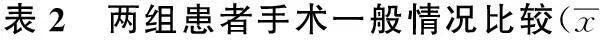
±s)

表3 两组患者术后12个月并发症发生情况/n(%)
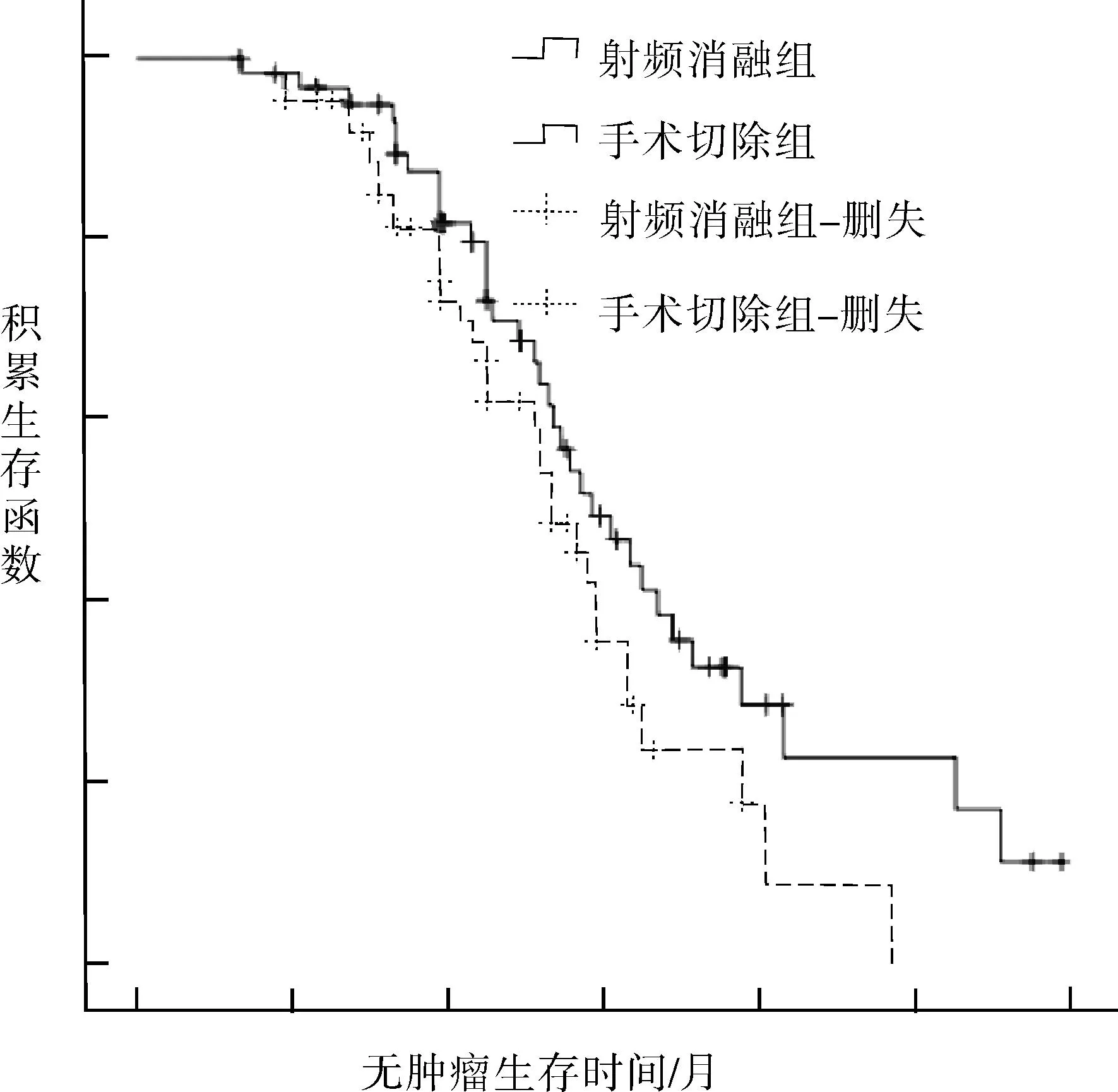
图1 两组患者无肿瘤生存中位时间分析
2.4两组患者术后预后情况射频消融组患者术后1、3、5年生存率分别为99.5%、74.8%和71.4%,手术切除组患者术后1、3、5年生存率分别为96.9%、68.2%和66.3%,两组相比差异无统计学意义(χ2=0.679,P>0.05),射频消融组患者术后无肿瘤生存中位时间29.3个月,手术切除组为26.7个月,Log Rank检验显示,两组患者无肿瘤生存中位时间差异无统计学意义(χ2=3.046,P=0.081),见图1。
3讨论
由于我国人群乙肝病毒感染率较高,我国小肝癌患者多数合并肝硬化门脉高压,常伴有脾功能亢进[5-6],在手术切除肿瘤组织的同时需对门脉高压进行处理,否则会导致患者凝血功能异常而影响患者预后[7]。有研究认为[8],对于合并有脾亢进的小肝癌患者联合脾切除可降低门脉压,减少对患者凝血功能的影响,有利于改善患者预后。临床上在对小肝癌手术方式的选择时,主要采取局部肿瘤组织切除术,以更好的保护正常肝组织,同时,局限性根治手术不会影响手术效果且有利于患者长期预后[9]。射频消融手术是近年来广泛应用临床的治疗方法,有研究对其在小肝癌中的治疗效果进行了研究,并获得了理想的治疗效果[10]。
本研究分别将射频消融术和手术切除术联合脾切除术应用于小肝癌患者,在进行射频消融操作时,利用超声作为辅助引导工具,不仅有效增加了消融区范围,而且不需阻断肝门,结果显示,射频消融组患者热缺血时间、手术时间和住院时间均短于手术切除组,术中失血量和输血量均少于手术切除组,说明采取射频消融联合脾切除治疗小肝癌可有效减少术中失血量及手术和住院时间,避免了手术切除术后创面大量出血的不足[11]。本研究显示,射频消融组患者术后12个月总并发症发生率6.4%,显著低于手术切除组的41.5%,说明射频消融联合脾切除治疗小肝癌可有效降低术后并发症的发生,这可能与射频消融术对患者创伤较小有关[12-13]。本研究显示,射频消融组患者术后1、3、5年生存率与手术切除组患者无差异,同时,射频消融组患者术后无肿瘤生存中位时间29.3个月长于手术切除组的26.7个月,但差异无统计学意义,说明射频消融联合脾切除术治疗小肝癌术后疗效与手术切除相当,不会影响患者预后,与Zhang L等[14]研究结论相同,但鉴于本研究样本量较少、随访时间有限,尚需进一步开展多中心、大样本、长期的随访研究予以证实。
综上所述,射频消融联合脾切除术治疗小肝癌伴脾亢进患者,治疗效果与手术切除联合脾切除术相当,不会影响患者预后,且可有效减少术后并发症发生,有利于患者术后恢复。
参考文献:
[1]Li JJ,Zheng JS,Cui SC,et al.C-arm Lipiodol CT in transcatheter arterial chemoembolization for small hepatocellular carcinoma[J].World J Gastroenterol,2015,21(10):3035-3040.
[2]Xu RH,Gao W,Wang C,et al.Retraction Note:Systematic evaluation of percutaneous radiofrequency ablation versus percutaneous ethanol injection for the treatment of small hepatocellular carcinoma:a meta-analysis[J].Eur J Med Res,2015,20(1):41-46.
[3]Hefaiedh R,Sabbegh M,Ennaifer R,et al.Percutaneous treatment versus hepatic resection for the treatment of small hepatocellular carcinoma[J].Tunis Med,2014,92(12):711-716.
[4]Feng K,Yan J,Li X,et al.A randomized controlled trial of radiofrequency ablation and surgical resection in the treatment of small hepatocellular carcinoma[J].J Hepatol,2012,57(4):794-802.
[5]项昆,赵鹤亮,张亚杰.多排螺旋 CT 与 MRI 对乙型肝炎肝硬化背景小肝癌检出的比较研究[J].医学综述,2015,21(4):744-745.
[6]苏瑛, 龚昭.经手术切除的原发性小肝癌患者复发的危险因素分析[J].安徽医药,2014,18(7):1306-1307,1308.
[7]高孟,李开艳,罗洪昌,等.原发性小肝癌超声引导下经皮微波消融与手术切除疗效的对比研究[J].中华超声影像学杂志,2015,24(1):35-39.
[8]胡善雷. 经皮射频消融与手术切除治疗小肝癌的疗效对比分析[J].实用癌症杂志,2015,30(2):188-190.
[9]Cho YK.A comparison of surgical resection and radiofrequency ablation for the treatment of single small hepatocellular carcinoma≤2 cm[J].Hepatology,2014,59(4):1653-1659.
[10] Pompili M,De Matthaeis N,Saviano A,et al.Single hepatocellular carcinoma smaller than 2 cm:are ethanol injection and radiofrequency ablation equally effective[J].Anticancer Res,2015,35(1):325-332.
[11] Fu C,Liu N,Deng Q,et al.Radiofrequency ablation vs.surgical resection on the treatment of patients with small hepatocellular carcinoma: a system review and meta-analysis of five randomized controlled trials[J].Hepatogastroenterology,2014,61(134):1722-1729.
[12] Park HJ,Lee MW,Rhim H,et al.Percutaneous ultrasonography-guided radiofrequency ablation of hepatocellular carcinomas: usefulness of image fusion with three-dimensional ultrasonography[J].Clin Radiol,2015,70(4):387-394.
[13] Bu X,Ge Z,Ma J,et al.Long-term efficacy of radiofrequency ablation compared to surgical resection for the treatment of small hepatocellular carcinoma[J].J BUON, 2015,20(2):548-554.
[14] Zhang L,Ge NL,Chen Y,et al.Long-term outcomes and prognostic analysis of radiofrequency ablation for small hepatocellular carcinoma: 10-year follow-up in Chinese patients[J].Med Oncol,2015,32(3):77-81.
Comparison on the clinical efficacies of radiofrequency ablation and
surgical resection combined with splenectomy in treatment of
small hepatocellular carcinoma associated with hypersplenis
ZHU Hai-lin
(The Department of Hepatobiliary Surgery, Central Hospital of Baoji City, Baoji,Shaanxi721000, China)
Abstract:ObjectiveTo comparison on the clinical efficacies of radiofrequency ablation and surgical resection combined with splenectomy in treatment of small hepatocellular carcinoma associated with hypersplenis.Methods127 cases of small hepatocellular carcinoma associated with hypersplenis were divided into radiofrequency ablation group (n=62) and surgical resection group (n=65), according to surgical methods. Cases in radiofrequency ablation group were taken radiofrequency ablation combined with splenectomy, while in surgical resection group were taken surgical resection combined with splenectomy. The general of the surgery of the two groups were recorded. The occurrences of complications after surgery 12 months in the two groups were compared. All patients were followed ended at February 2015, the 1, 3 and 5-year survival and tumor-free survival of the two groups were compared.ResultsThe warm ischemia time, operative time and hospital stay of the patients in the radiofrequency ablation group were shorter than surgical resection group, and the volumes of intraoperative blood loss and transfusion were less than surgical resection group, the differences were statistically significant (P<0.05). The occurrence of complications after surgery 12 months in radiofrequency ablation group was 6.4%, which was significantly lower than 41.5% of the surgical resection group, the difference was statistically significant (P<0.05). The 1, 3, 5-year survival rates of radiofrequency ablation group were 99.5%, 74.8% and 71.4%, while the surgical resection group were 96.9%, 68.2% and 66.3%, the two groups showed no significant difference (P>0.05). The median tumor-free survival time of radiofrequency ablation group was 29.3 months, which was longer than 26.7 months of the surgical resection group, but the difference was not statistically significant (P>0.05).ConclusionsThe treatment effect of radiofrequency ablation combined with splenectomy in treatment of small hepatocellular carcinoma associated with hypersplenis was quite with and surgical resection combined with splenectomy, and could effectively reduce postoperative complications and conducive to postoperative recovery.
Key words:small hepatocellular carcinoma;hypersplenism;radiofrequency ablation;surgical resection;splenectomy
收稿日期:(2015-06-06,修回日期:2015-09-09)
doi:10.3969/j.issn.1009-6469.2016.01.027