经阴道腹腔镜胆囊切除术的临床应用
2016-01-11向川南,姚健,王宁等
经阴道腹腔镜胆囊切除术的临床应用*
向川南姚健王宁桑晓梅
(泸州市人民医院外二病区, 四川 泸州 646000)
【摘要】目的探讨经阴道腹腔镜胆囊切除术的可行性与安全性。方法 对5例于2009~2014年入院的胆囊结石患者行经阴道腹腔镜胆囊切除术。其中3例伴有妇科并发症患者先行阴式子宫全切术,然后经阴道残端放入SILS PORT,其余患者经阴道后穹隆3 cm切口安放SILS PORT,三通道内分别插入3个软性器械套管,建立防止漏气的通道,充气后首先于SILS PORT 6点位通道置入腹腔镜,探查腹盆腔情况,并监视硬质弯曲操作器械通过3点及9点位通道到达胆囊区附近。分离钳分离出胆囊管及胆囊动脉,置入钛夹分别夹闭胆囊管及胆囊动脉,常规切除胆囊,电凝胆囊床;经阴道取出胆囊;缝合阴道残端或阴道后穹窿,安置尿管。其中3例患者因腹腔有粘连,为防止对肠管造成损伤,经脐戳孔安置trocar放入腹腔镜监视下放入操作器械。1例合并右肾囊肿者完成胆囊切除后,游离出囊肿,距肾实质0.5 cm切除囊壁,残留囊壁适当电凝,检查无出血及胆漏、尿漏,胆囊及囊壁组织经阴道切口取出体外。于脐部辅助戳孔并放置引流管。直视下用可吸收线连续缝合阴道后穹隆切口,安置尿管。结果5例均无中转开腹。胆囊切除时间27~55 min,平均胆囊切除术时间(38.4±10.4)min;肾囊肿切除时间49 min,术中平均出血量(28±10.4)ml。术后平均住院时间为(3.8±0.8)d。术后随访6~12个月,全组无出血,无明显腹壁手术瘢痕,无胆漏、尿漏等并发症发生。结论经阴道腹腔镜胆囊切除术安全可行,并可同期治疗多脏器病变,具有临床推广应用价值。
【关键词】胆囊切除术; 自然腔道; 阴道; 腹腔镜
【中图分类号】R 616.5【文献标志码】A
基金项目:四川省卫生厅科研课题(120390)
通讯作者:王宁,E-mail:wn_lzsryw2k@163.com
收稿日期:( 2014-11-24; 编辑: 张文秀)
The clinical application of transvaginal laparoscopic cholecystectomy XIANG Chuannan, YAO Jian, WANG Nning,etal
(SurgicalDepartmentTwo,TheLuzhouPeople'sHospital,Luzhou646000,Sichuan,China)
Abstract【】ObjectiveTo investigate the feasibility, safety and superiority of natural orifice translumenal (transvaginal) endoscopic cholecystectomy. Methods5 inpatients with cholecystolithiasis were treated with the transvaginal lapatoscopic cholecystectomy during 2009 to 2014. 3 cases with gynecological complications were treated with the vaginal hysterectomy, firstly. Then place single incision laparoscopic surgery port (SILS PORT) through the vaginal residue. The rest of patients placed the SILS PORT through the 3cm incision on the posterior fornix of vagina. Three soft manipulator cannulas were inserted in three channels separately to establish the channels against leakage. After inflation, we placed the laparoscope in the abdominal cavity through 6 o'clock position channel of SILSPORT to check the condition of abdominal cavity and cavitas pelvis and to monitor the curvate manipulator to reach at the cholecyst through the 3 and 9 o'clock channels. We separated the cystic duct and cystic artery, and did the occlusion with the titanium clamp separately. Then we did the routine cholecystectomy and electrocoagulation of gallbladder bed. After that, the gallbladder was removed out from the vagina. Then the vaginal residue or posterior fornix of vagina was closed. Finally, the catheter placed. The 3 cases with abdominal adhesion were completed by the umbilical auxiliary trocar in order to prevent from intestinal injury. One case accompanied by the right kidney cyst was dissociated the cyst and cut the wall of the cyst 0.5cm far from the kidney and electrocoagulate the rest of the wall after the cholecystectomy. After checking, if there were hemorrage, bile leakage and urine leakage, we removed the gallbladder and cyst wall from the vagina orifice, then placed the drainage tube. Finally, using the absorbed surgical suture closes the incision on the posterior fornix of vagina under direct vision. Finally place the catheter. ResultsAll of five patients were without laparotomy, bleeding, and bile leakage, urinary leakage and other complications. The gallbladder removal time was 27~55 min. The average time of surgical gallbladder removal was (38.4±10.4) min. Renal cyst removed at 49 min. The average hospitalization time was (3.8±

0.8)d.The average amount of bleeding during the operation was (28±10.4)ml There was no surgical scar on abdominal wall and no abnormality after six-month -to -one-year review.ConclusionCompared with the traditional laparoscopic surgery, transvaginal laparoscopic cholecystectomy is feasible and safe. It has obvious advantages and can do the treatment of multi-organ diseases in the same time.
【Key words】Cholecystectomy; Natural orifice; Vagina; Laparoscopy
经自然腔道内镜手术(natural orifice translumenal endoscopic surgery,NOTES)是通过胃、阴道、结直肠等自然腔道进入腹腔治疗疾病的手术方式,其优势是减轻患者术后疼痛,促进术后康复等,并达到体表无瘢痕的效果。因其术后腹壁无瘢痕,引起了微创外科界的广泛关注。NOTES由于受设备和器械的限制,如何选择安全的腹腔入路、空腔脏器穿刺口的安全闭合、预防感染和缝合等均处于探索阶段[1]。而在直视或腹腔镜辅助入口可视下,采用经阴道后穹窿入路进入人体开展NOTES,是安全可行的[2]。我院2009年~2014年施行经阴道腹腔镜胆囊切除术5例,均获成功,现报告如下。
1资料与方法
1.1一般资料观察病例为2009~2014年入住我科的5例胆囊结石患者,年龄17~60岁,平均(44.8±16.4)岁。其中3例为胆囊多发结石,2例为胆囊单发结石。胆囊结石最大直径0.5~1.0cm,平均(0.8±0.2)cm。其中2例患者合并子宫肌瘤,1例合并子宫Ⅱ度脱垂;1例患者合并右肾囊肿,B超示囊肿大小为7. 4 cm×6.5 cm,静脉肾盂造影检查证实囊肿与集合系统不相通,见表1。病例入选标准:胆囊良性病变,无严重炎症粘连及其他手术禁忌症。
1.2手术方法采用美国Stryke腹腔镜系统,5 mm 30°镜头、电钩、电凝棒、钛夹钳;杭州康基医疗器械有限公司硬质弯曲器械,软性器械套管及“三通转换器”(single incision laparoscopic surgery port,SILS PORT)。德国ERBE Vio 200D型电外科工作站。
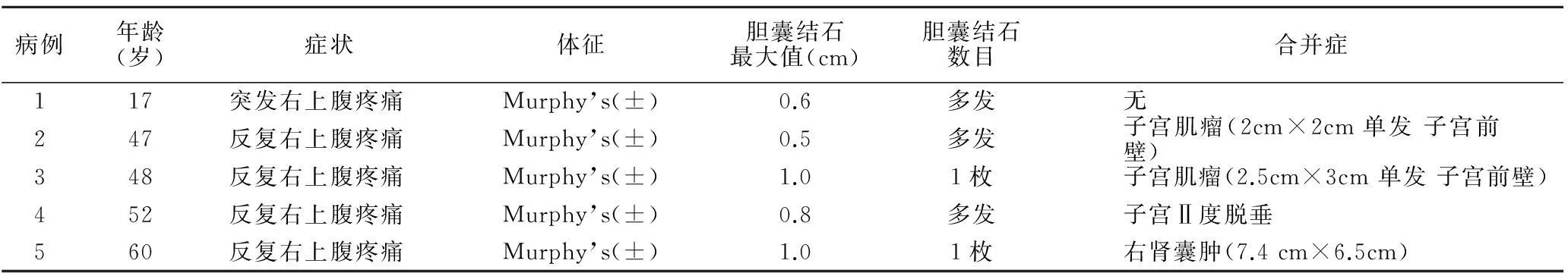
表1 一般资料
于全身麻醉后,3例伴有妇科并发症患者取膀胱截石位,先行阴式子宫全切术,而后取头低足高30°截石位,于阴道残端安置SILS PORT;其余患者全麻后取头低足高30°截石位。直视下切开阴道后穹隆3 cm。切口处安放SILS PORT,三通道内分别插入3个软性器械套管建立防止漏气的通道。充气后首先于SILS PORT 6点位通道置入腹腔镜,探查腹盆腔情况,并监视硬质弯曲操作器械通过3点及9点位通道到达胆囊区附近。调整体位至头高足低30°,右侧倾斜15°,用抓钳向上提起胆囊颈,分离钳分离出胆囊管及胆囊动脉,辨清胆囊管、肝总管和胆总管的关系后,置入钛夹分别夹闭胆囊管及胆囊动脉,常规切除胆囊,电凝胆囊床;经阴道取出胆囊。3例行阴式子宫全切术患者直视下用可吸收线连续缝合阴道残端、膀胱腹膜返折处,修补阴道前后壁,缝合会阴部皮肤;其余患者缝合阴道后穹隆切口。阴道内填入碘伏纱布,安置尿管,手术结束。1例合并右肾囊肿者完成胆囊切除后,游离出囊肿,距肾实质0.5 cm切除囊壁,残留囊壁适当电凝,检查无出血及胆漏、尿漏后,将胆囊及囊壁组织经阴道切口取出体外, 直视下用可吸收线连续缝合阴道后穹隆切口于脐部辅助戳孔并放置引流管1根,安置尿管后完成手术。其中3例患者因有腹腔粘连,为防止对肠管造成损伤,经脐戳孔安置trocar放入腹腔镜监视下放入操作器械,见表2。
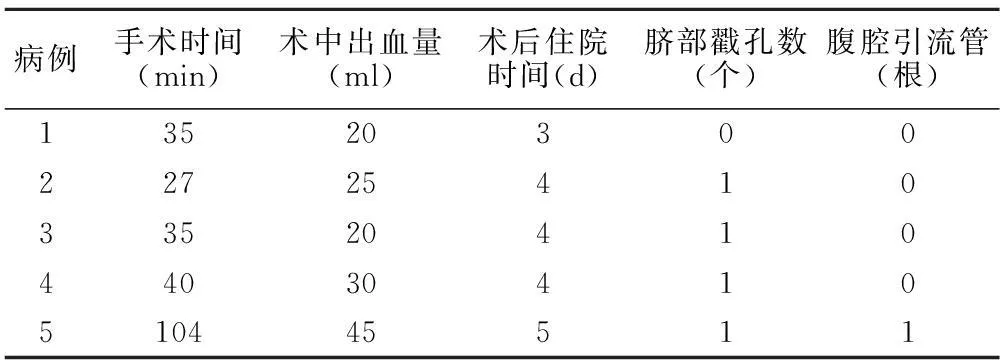
表2 术中及术后情况
2结果
2.15例患者手术均顺利完成,无中转开腹。胆囊切除时间27~55 min,平均胆囊切除术时间(38.4±10.4)min;肾囊肿切除时间49 min。术中出血量平均(28±10.4)ml,术后住院平均(3.8±0.8)d,见表2。
2.2术后随访6~12个月,全组无出血,无明显腹壁手术瘢痕,无胆漏、尿漏等并发症发生。
3讨论
2004年,Kalloo等[3]首先提出NOTES概念,发表了经胃内镜动物腹腔探查的实验报告。随后NOTES成为国内外研究的热点。我国王子恺等[4]于2009年进行了经自然腔道内镜手术的动物实验研究。至今动物模型已包括了NOTES的诸多应用,如经胃胆囊切除术、脾切除术、胃空肠吻合术等。而Gettman等[5]最早报道在猪模型中实施经阴道的肾切除术。因经阴道途径无需考虑渗漏问题,可直视下缝合,是国内外许多学者常用的研究路径[6-8]。 显示这项技术的优越性。我院由初期成功进行经阴道联合经脐腹腔镜胆囊切除术,积累经验后,成功完NOTES经阴道腹腔镜胆囊切除术[9],并探索经阴道腹腔镜下同期行多脏器手术。
阴道是女性解剖的自然腔隙,具有伸展性强、愈合能力好等解剖特点。妇产科医生已经证实应用腔镜联合阴道内镜进行子宫切除具有安全性,与开腹手术相比,对患者创伤小,并发症少,认为经阴道入路是可行的[10]。此外,外科医师也经由阴道切口取出大型标本,包括胆囊、结肠、脾脏、肾脏等。阴道后穹隆切口便于缝合,不易发生感染,愈合后美容效果良好,可预防切口疝的发生,很少发生女性性功能障碍。上述为经阴道内镜手术奠定了技术基础,并克服了伦理方面的问题。
操作通道的建立及器械的置入一直是经阴道腹腔镜手术的难点,关系到手术操作的灵活性,甚至决定了手术的成功与否。第1例在建立气腹时采用阴道内填入纱布,效果差,操作时器械不稳定,后改为SILS PORT,有效地克服了上述不足。经SILS PORT放置超长尾端去除进气螺栓的trocar。trocar端错开,不在同一平面,可减少或避免器械间的冲突,使操作相对较灵活。超长trocar使腔镜操作器械容易到达手术区域,有效防止放置过程中对大网膜或肠管的损伤[11]。在初期行经阴道腹腔镜手术建立操作通道及器械置入时,最好经脐孔置入trocar置入腹腔镜监视,防止损伤肠管,熟练后再行PURE NOTES。术中如遇操作困难,也应及时于脐部辅助戳孔,以利于手术安全完成。脐部切口隐蔽,不增加手术创伤,术后同样可以达到腹壁无瘢痕的美容效果。
我们体会到,使用常规腹腔镜手术器械操作时缺乏满意的立体感、空间感,而且“同轴平行-管状视野”的缺陷比较明显,给手术带来很大困难,需要预先将手术器械置入手术区域才能进行操作。因手术器械长,不易控制远端,要求手术操作动作幅度小,操作更精细,才能避免损伤邻近组织。为防止术中“热分离”时发生灼热副损伤,在解剖胆囊三角区时均采用“冷分离”方式。术中使用弯曲操作器械,较好地克服了使用常规腹腔镜器械时手柄在体外“拥挤”的现象,更接近腹腔镜遵循的“三角型”最佳操作角度,降低手术难度。该技术可以同时处理两个以上腹部病变[12],避免患者多次手术,降低手术风险及费用,具有良好的微创和美容效果。
经阴道腹腔镜手术操作难度大,不足之处为:①器械相对集中,空间狭小,难以形成操作三角,相互干扰,影响操作。②腹腔镜与器械几乎平行,器械之间易发生遮挡,影响手术视野。③操作受患者体形影响较大,肥胖、身材较高的患者,常规器械的长度难以达到要求。本院近期引进了一种新型迷你抓钳-Minilap抓钳(直径2.3mm),在经脐入路腹腔镜胆囊切除中应用,大大降低了手术难度[13]。Minilap抓钳应用于本术式,选用3D技术将会使手术得以简化,医师操作时更有底气[14]。
4结论与展望
创伤、疼痛、瘢痕一直被认为是手术的必然产物,但近年来一种无痛无瘢痕的全新技术引起了腹腔镜外科医生和内镜医生的极大兴趣,成为研究和争论的焦点,这就是NOTES[15]。经阴道腹腔镜手术既具有无瘢痕、微创的优点,又避免了穿刺口闭合和腹腔感染的潜在危险,是腹腔镜不断发展的成果,也是现阶段最可行的NOTES。此技术的发展速度依赖于手术器械的进步,相信随着经验的积累和技术水平的提高,可以应用于更多的腹部手术,将成为微创外科的发展方向。
【参考文献】
[1]杨勇致,潘雪萍,景宇,等.透明帽吸引内镜夹闭合法在经自然腔道内镜外科手术切口闭合中的实验研究[J].重庆医学,2014,43(33):4498-4499.
[2]曹月敏.NOTES的发展史、现状与前景[J].中国微创外科杂志,2010,10(1):25-27.
[3]Kalloo AN,Singh VK,Jagannath SB,etal.Flexible transgastric peritoneoseopy:a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity[J].Gastrointest Endosc,2004,60(1):114-117.
评估[J].临床肺科杂志. 2007, 12(12):1323-1324.
[8]Boldrini R,Fasano L,Nava S. Noninvasive mechanical ventilation [J]. Curr Opin Crit Care. 2012, 18(1):48-53.
[9]Basnet S,Mander G,Andoh J,Klaska H,Verhulst S,Koirala J.Safety efficacy and tolerability of early initiation of noninvasive positive pressure ventilation in pediatric patients admitted with status asthmaticus: a pilot study [J].Pediatr Crit Care Med. 2012, 13(4):393-398.
[10] Garcia Vicente E,Sandoval Almengor JC,Díaz Caballero LA,Salgado Campo JC. Invasive mechanical ventilation in COPD and asthma]. [J] Med Intensiva. 2011, 35(5):288-298.
[11] 颜明治,吕祖铭,陈黎.无创正压通气对轻度哮喘急性发作患者的影响[J]. 重庆医学2005, 7(8):345-348.
[12] Kida Y,Minakata Y,Yamada Y,Ichinose M.Efficacy of noninvasive positive pressure ventilation in elderly patients with acute hypercapnic respiratory failure[J]. Respiration. 2012, 83(5):377-382.
[13] 吕祖铭,陈黎,张晓星.无创正压通气治疗支气管哮喘急性发作[J].中华急诊医学杂志2005, 7(14): 596-598.
[14] 赵旭文,刘春涛. 支气管哮喘急性发作患者死亡相关因素分析[J].西部医学.2011, 23(7) :1270-1272.
[15] Soroksky A, Klinowski E, Ilgyev E, Mizrachi A, Miller A, Ben Yehuda TM, Shpirer I,Leonov Y.Noninvasive positive pressure ventilation in acute asthmatic attack.Eur Respir [J] Rev. 2010, 19(115):39-45.
[16] Nakasone C, Touyama M, Namisato S, Okudaira S, Fujita J. Therapy for acute exacerbation of bronchial asthma using noninvasive positive pressure ventilation by critical care ventilator[J]. Nihon Kokyuki Gakkai Zasshi. 2010, 48(5):370-374.
[17] Scala R.Noninvasive ventilation in severe acute asthma? Still far from the truth[J].Respir Care. 2010, 55(5):630-637.