肩关节钙化性肌腱炎的关节镜治疗及急慢性期疗效比较
2015-06-24陈建海张一翀张殿英付中国杨明党育姜保国
陈建海 张一翀 张殿英 付中国 杨明 党育 姜保国
·论著·
肩关节钙化性肌腱炎的关节镜治疗及急慢性期疗效比较
陈建海 张一翀 张殿英 付中国 杨明 党育 姜保国
目的 评估关节镜下清除钙化性肌腱炎肩袖钙化病灶的治疗效果,探讨急性期组与慢性期组手术治疗后的疗效差别。方法 收集北京大学人民医院创伤骨科2009年9月至2014年6月收治的钙化性肌腱炎病例,符合标准者28例。按照发病至手术时间的不同分为急性期组和慢性期组,比较两组术后Constant评分提升幅度,SST问卷增长个数,前屈、外旋角度改善及VAS评分下降的情况。结果 急性期组在术后Constant评分(t=3.242,P=0.003)、SST问卷完成个数(t=2.080,P=0.048)、前屈角度(t=2.08,P=0.048)及VAS评分(t=2.394,P=0.024)四方面改善程度优于慢性期组,而两组在外旋角度改善方面差异无统计学意义(t=0.764,P=0.452)。结论 关节镜下钙化灶清除可以显著改善患者肩关节功能、缓解疼痛。急性期患者与慢性期患者临床疗效相当。
肩关节;肌腱炎;关节镜;手术治疗
肩袖钙化性肌腱炎是引起肩痛的常见疾病之一,多发于30~50岁人群[1],女性较多见[2]。钙化性肌腱炎急性发作时患者表现为无明显诱因出现的肩关节持续性剧烈疼痛,症状严重时甚至需要到急诊寻求治疗。多数急性发作患者可以通过保守治疗获得较为满意的效果;但对于保守治疗无效或症状持续不缓解,严重影响工作和生活的患者,手术直接清除钙化灶是公认的有效治疗方法。近年来,随着肩关节镜技术的不断发展,关节镜下清除钙化物成为一种常规手术方法,也获得了很好的治疗效果[3-4]。我们回顾性评估关节镜下清除钙化性肌腱炎肩袖钙化灶的治疗效果,并探讨急、慢性期患者手术治疗后的肩关节功能改善情况。
资 料 与 方 法
一、一般资料
收集本院2009年9月至2014年6月收治的钙化性肌腱炎病例。入选标准:(1)患者有剧烈肩关节疼痛的病史;(2)经保守治疗无效;(3)行关节镜手术的患者。排除标准:(1)合并肩袖损伤的患者;(2)行切开手术的患者。最终符合入选标准者28例。以急性发病到行关节镜下钙化灶清除术的时间不同分为急性期组和慢性期组。初次肩痛发作后至行关节镜下钙化灶清除术病程≤3个月的患者为急性期组;初次肩痛发作至行关节镜下钙化灶清除术病程>3个月,且经保守治疗仍未好转或反复发作者为慢性期组。28例患者均有不同程度的患侧疼痛及肩关节活动受限。所有患者术前均行影像学检查,根据X线片判断肩关节钙化灶大小、形态,了解肩峰形态。肩部X线片显示肩峰下及偏外侧的滑囊内肩袖区有类椭圆形或长条形的高密度云雾状钙化影(图1)。急性期患者共10例,年龄38~68岁,平均52.6岁,其中左肩5例,右肩5例。症状均为急性肩痛,呈针刺样感,伴局部皮温增高,肩部明显压痛,肩关节活动严重受限且影响生活。术前X线片均可见肩峰下肩袖区高密度钙化影。慢性期患者18例,年龄40~73岁,平均55.5岁;其中左肩7例,右肩11例,所有患者有剧烈肩痛史,剧烈疼痛持续一段时间后疼痛程度有所减轻,但一直没有消失,肩痛时轻时重,肩关节功能明显受限,影响正常生活。
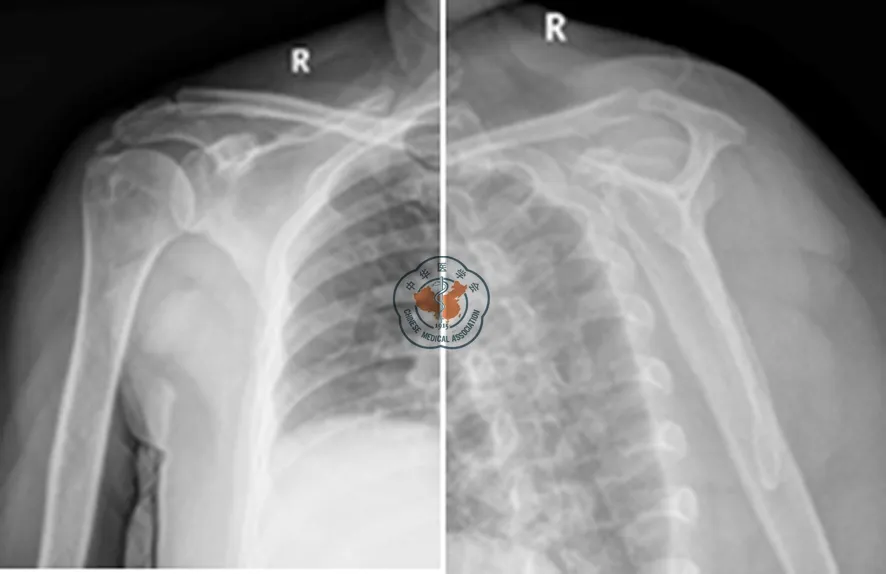
图1 钙化性肌腱炎X线片表现

图2 针头穿刺钙化灶 图3 锚钉缝线穿过切开的肌腱 图4 缝线打结,完成肩袖修复
二、手术方法
所有手术由北京大学人民医院副主任医师或主任医师完成。均采用全身麻醉、沙滩椅体位,术前做好体表标记。关节镜经后方入路置入,检查盂肱关节腔。通常关节囊内壁有严重炎性滑膜增生充血,部分关节活动受限,患者肩袖间隙挛缩,盂肱中韧带增厚,肩袖结构均完整。清理关节腔内滑膜组织,松解肩袖间隙和盂肱中韧带。使用穿刺针头经肩峰外缘穿刺冈上、冈下肌腱,寻找钙化灶位置,如果针头刺到钙化灶,针头尖部可以看到钙化物(图2)。确定钙化灶位置后经过针头引入1枚PDS线作为标记。然后将关节镜转入到肩峰下间隙,常常可以看到明显的肩峰下滑膜增生充血,有时可以在滑膜上看到已经流出的钙化物。使用刨刀彻底清理肩峰下滑膜,射频刀止血,清晰暴露肩袖滑膜侧结构。通过缝线标记定位好钙化灶位置,而后用刀片顺着肌腱纤维的走行切开肌腱显露病灶。使用刮勺清除钙化灶,可以看到逸出的钙化物似牙膏状物质,在肩峰下间隙内弥散后呈“暴风雪”征象。清除钙化灶时应尽量避免肩袖遭受进一步破坏,彻底清除钙化灶后再次仔细探查肩袖肌腱的缺损情况,对于钙化灶巨大、涉及肌腱深度超过50%或者肩袖足印骨面暴露时,应用1枚4.5 mm缝合锚进行肩袖修复(图 3,4)。9例患者术中进行了肩袖修复。如合并肩峰下骨赘需彻底去除,有8例患者同时行肩峰成形术。
三、术后康复及评估
术后即对患肢进行颈腕吊带悬吊固定,术后1周内予以适当的冰敷消肿,并开始用健侧手协助被动运动肩关节,并逐渐增加活动范围。1周后逐步进行主动活动,6 周后进行肩关节抗阻力训练并行牵拉治疗,术后3个月活动范围可达到正常,并可基本恢复日常生活。对合并有肩袖修补手术的患者应在术后6周进行主动锻炼,以免修补部位的锚钉松动或再度撕裂。每位患者术前、术后常规进行Constant评分,简明肩关节评分(SST),肩关节活动范围检查和VAS疼痛评分。
四、统计学分析
应用 SPSS 15.0软件进行统计学分析,对手术前后数据进行配对资料t检验,P<0.05为差异具有统计学意义。
结 果
共28例患者纳入本项回顾性研究,术后随访6~33个月(平均18.8个月)。术后定期复查X线片,均显示钙化点消失。所有病例均在治疗前以及术后随访时进行Constant评分、SST问卷评估、肩关节活动范围检查以及VAS评分(表1,2)。10例急性期患者,Constant评分治疗前平均为51.36分,治疗后平均为88.16分,平均增长约36.80分。其中前屈上举角度增长约77.00°,外旋角度增长约18.50°。SST问卷治疗前回答“是”的问题平均为5.02个,治疗后回答“是”的问题平均为9.32个,平均增长约4.30个。VAS评分治疗前平均为9.12分,治疗后平均为4.62分,平均下降约4.50分。18例急性期患者,Constant评分治疗前平均为63.70分,治疗后平均为88.03分,平均增长约24.33分。其中前屈上举角度增长约66.39°,外旋角度增长约15.28°。SST问卷治疗前回答“是”的问题平均为6.33个,治疗后回答“是”的问题平均为9.66个,平均增长约3.33个。VAS评分治疗前平均为7.30分,治疗后平均为4.19分,平均下降约3.11分。

表1 急、慢性期患者手术前后评分及肩关节活动范围)

表2 急、慢性期患者手术后评分及肩肘关节活动范围改善程度)
本研究中,28例钙化性肌腱炎患者经关节镜下钙化灶清除术后,肩关节功能均有不同程度的改善;且急性期钙化性肌腱炎经手术治疗后Constant 评分提升幅度(t=3.242,P=0.003)、SST增长个数(t=2.080,P=0.048)、前屈上举角度改善(t=2.08,P=0.048)及疼痛缓解程度方面(t=2.394,P=0.024)明显高于慢性期。差异具有统计学意义(P<0.05)。本研究中共有9例行肩袖修复,其中急性期2例,占急性期病例数的20%;慢性期7例,约占慢性期病例数的38.9%。
讨 论
文献报道肩袖钙化性肌腱炎的发病率在2.7%~20%。肩袖钙化灶可出现在任意的肌腱,尤以冈上肌腱的发病最为常见[1-2,5]。目前肩袖钙化性肌腱炎病因尚不明确,争论较大。多数认为其发生与肩袖退行性改变、肩袖乏血管区、代谢紊乱及细胞介入调节反应等因素有关。冈上肌在上臂外展、上举的起动运动及稳定盂肱关节方面均起重要作用,是肩袖肌群中退变发生最早的肌肉。Codman[6]在1934年提出冈上肌腱在大结节止点近侧l cm范围是乏血管区,血供最差,受应力作用的影响最大,也是引起退变的主要原因,在退变的基础上,进一步局部钙盐代谢异常导致钙盐沉着,形成冈上肌腱钙化性肌腱炎。Uhthoff等[7]根据钙化性肌腱炎的病理过程将其分为三期。第一期为钙化前期,此期无症状,肌腱组织发生纤维软骨化生,即由胶态的致密结缔组织被半固态的软骨组织替代,这种刺激物是钙化前的早期阶段,患者通常没有临床症状。第二期为钙化期,又可分为钙化形成期、静止期和吸收期。钙化形成期,肌腱内发生软骨细胞介导的钙化,形成钙化物沉积,此时可能无症状或有不同程度的疼痛。当胶原纤维组织包围钙化中心而没有出现炎症征象时即进入静止期,提示钙质沉积过程的终结。然后是吸收期,钙沉积的周边出现血管通道,接着发生钙的吸收。此阶段可出现极度的疼痛,患者多在此时开始寻求治疗。此时的钙沉积有些像奶油或牙膏。当钙沉积吸收后,死腔有肉芽组织填充。第三期为钙化后期。此期肉芽组织转变为成熟的胶原组织,纤维沿着与肌腱长轴一致的应力线排列,恢复正常的肌腱结构。此期疼痛显著减退。
急性钙化性肌腱炎有如下临床特点:(1)起病急,疼痛剧烈,患者能指出具体的发病时间,甚至需要到急诊就诊,患者有明显夜间痛;(2)肩关节通常无法耐受活动,各个方向活动明显受限;(3)受累区域常有压痛;(4)保守治疗后症状逐渐缓解,部分患者保守治疗效果不理想。因此患者常积极寻求进一步治疗。急性期病灶多处于病理分期的钙化期,此期钙化灶已经形成,病灶较为完整,易彻底清除。且钙沉积的周边出现血管通道,接着巨噬细胞及多核巨细胞等炎性细胞参与吸收过程,此阶段可出现极度的疼痛及严重的功能受限,因此术前评分较低。如在此期将病灶清除,不但阻止病情进一步进展,而且急性期患者功能评分提升幅度更大,功能改善更为显著。这就解释了为什么本研究中急性期组患者较慢性期具有更明显的疗效。而对于钙化性肌腱炎的急、慢性期的准确界定,目前国内外尚缺乏客观、统一的标准。本研究根据患者的病程长短进行分期,视初次肩痛发作后病程≤3个月的患者为急性期组;而初次肩痛发作>3个月,且经保守治疗仍未好转或反复发作者为慢性期。这实际上是一种主观分期,但按照本研究提出的分期,患者临床表现明显不同,治疗内容也有差异,比如在慢性期组有更多的患者需要进行肩袖修复和肩峰成形,这可能提示慢性期患者肩袖病变是导致疼痛反复发作的重要原因。
虽然肩袖钙化性肌腱炎有很强的自愈倾向,但是这个自愈的过程很容易受阻,且引起剧烈疼痛[8]。对于手术治疗的适应证目前仍存在争议,多数患者可通过药物、物理治疗等方法获得满意的效果[3]。调查显示仍有部分患者经保守治疗无效。Rochwerger等[9]报道的手术成功的案例,在进行切开钙化灶清除术以及肩峰成形术后,经过23个月的随访期,Constant评分由51.36分上升至88.16分。切开手术的倡导者认为这种手术更为简单,且直视下可以较容易地修补肩袖。但随着技术的发展,自1987年关节镜手术同样可以缩短住院时间及迅速恢复[10]。对于钙化性肌腱炎,关节镜的优势在于损伤小、恢复快,且能避免三角肌止点的破坏,还能对盂肱关节以及肩峰下间隙内的损伤一并处理。通常在肩袖关节面侧足印区附近可以见到草莓红斑,这代表了区域血管的增生。钙化沉积灶常见于冈上肌,距离大结节附着点1.5~2 cm[11]。当钙化灶较难明确时,需使用硬膜外穿刺针定位。有时术中透视对于定位钙化灶也是有帮助的。一旦确定钙化灶的位置,就可使用关节镜下的刀片顺着肌腱纤维的走行切开并清除病灶。在手术最后阶段可以对盂肱关节及肩峰下间隙进行冲洗,防止钙化灶的残留。这对于防止继发肩关节僵硬是非常有效的,因为关节僵硬在钙化性肌腱炎术后较为常见,约占9%~15%[12-13]。多数学者认同术中清除钙化灶的必要性,但对于是否进行肩峰下成形目前争议较大。Molé等[12]认为对于微小钙化灶有必要行肩峰成形术,也有学者认为行肩峰下减压可以促进钙化灶的吸收[14]。但也有人认为这对手术最终效果没有影响[15-17]。我们认为,对于慢性期患者,很难区分疼痛是由钙化灶还是肩峰下撞击引起。我们在术前常规拍摄冈上肌出口位X线片,术中如发现肩峰下表面有撞击磨损表现,肩峰呈Ⅱ型或Ⅲ型,则行前肩峰成形术。但这仍缺乏较为确切的理论依据,仍需今后进一步的深入研究。
Romain等[4]认为关节镜清理术残留的钙化物可逐渐被吸收,对最终疗效无明显影响。而Giuseppe等[3]却认为钙化物残留与术后疼痛关系密切。本文作者认为对于钙化灶应尽量清除,少量残留不会影响临床症状的恢复。钙化灶清除后在肩袖肌腱内遗留空隙,造成部分性肩袖损伤。Maier等[15]认为对于清理钙化灶产生的较大的肩袖损伤,需进行缝合,对于小的肩袖损伤可不予处理。我们在术中注意控制清创范围,对于损伤滑囊面深度超过肩袖肌腱厚度1/2,或者肩袖足印骨面暴露的患者,为防止术后肩袖断裂,影响肩关节功能,需行肩袖修补术。本组病例中有9例行肩袖修补,其中急性期2例,占急性期病例数的20%;慢性期7例,约占慢性期病例数的38.9%。术后功能均恢复良好。本研究中慢性期行肩袖修补患者比例较大,原因可能是多方面的,钙化灶会引起症状,肩袖退变性损伤也会引起症状,慢性期患者常伴发肩袖退变性损伤,这是进行肩袖修复比例高于急性期的一个原因。
结论:肩袖钙化性肌腱炎是引起急性肩痛的常见疾病之一。当症状严重影响日常生活,且保守治疗无效时,尽早行关节镜下钙化灶清理术可取得理想的预后。
[1] Depalma AF,Kruper JS.Long-term study of shoulder joints afflicted with and treated for calcific tendinitis[J].Clin Orthop,1961,20(20):61-72.
[2] Bosworth BM.Calcium deposits in the shoulder and subacromial bursitis-A survey of 12,122 shoulders[J].J Am Med Assoc,1941,116(116):2477-2482.
[3] Giuseppe P,Paolo P,Fabrizio C,et al.Arthroscopic treatment of calcifying tendonitis of the shoulder:clinical and ultrasonographic follow-up findings at two to five years[J].J Shoulder EIbow Surg,2004,13(5):503-508.
[4] Romain S,Heike L,Dieter K,et al.Arthroscopic treatment of chronically painful calcifying tendonitis of the supraspinatus tendon[J].Arthroscopy,2006,22(5):521-527.
[5] Rowe CR.Calcific tendinitis[J].Instr Course Lect,1985,34,196-198.
[6] Codman EA.The shoulder[M].Boston:Todd,1934:178-215.
[7] Uhthoff HK,Sarkar K.Calcifying tendinitis[J].Baillieres Clin Rheumatol,1989,3(3):567-581.
[8] 蔡第心,谭洪波,杨军,等.肩袖钙化性肌腱炎的病程研究分期及治疗进展[J/CD].中华肩肘外科电子杂志,2014,2(4):248-250.
[9] Rochwerger A,Franceschi JP,Viton JM,et al.Surgical management of calcific tendinitis of the shoulder:an analysis of 26 cases[J].Clin Rheumatol,1999,18(4):313-316.
[10] Ellman H.Arthroscopic subacromial decompression:analysis of one-to three-year results[J].Arthroscopy,1987,3(3):173-181.
[11] Lam E,Bhatra D,Van Rooyen K,et al.Modern management of calcifyingtendinitis of the shoulder[J].Curr Orthop,2006(20):446-452.
[11] Balke M,Bielefeld R,Schmidt C,et al.Calcifying tendinitis of the shoulder:midterm results after arthroscopic treatment[J].Am J Sports Med,2012,40(3):657-661.
[12] Molé D,Kempf JF,Gleyze P,et al.[Results of endoscopic treatment of non-broken tendinopathies of the rotator cuff.2.Calcifications of the rotator cuff][J].Rev Chir Orthop,1993,79(7):532-541.
[13] Sirveaux F,Gosselin O,Roche O,et al.Postoperative results after arthroscopic treatment of rotator cuff calcifying tendonitis,with or without associated glenohumeral exploration[J].Rev Chir Orthop Reparatrice Appar Mot,2005,91(4):295-299.
[14] Tillander BM,Norlin RO.Change of calcifications after arthroscopic subacromial decompression[J].J Shoulder Elbow Surg,1998,7(3):213-217.
[15] Maier D,Jaeger M,Izadpanah K,et al.Rotator cuff preservation in arthroscopic treatment of calcific tendinitis[J].Arthroscopy,2013,29(5):824-831.
[16] Jacobs R,Debeer P.Calcifying tendinitis of the rotator cuff:functional outcome after arthroscopic treatment[J].Acta Orthop Belg,2006,72(3):276-281.
[17] Loew M,Daecke W,Kusnierczak D,et al.Shock-wave therapy is effective for chronic calcifying tendinitis of the shoulder[J].J Bone Joint Surg Br,1999,81(5):863-867.
(本文编辑:李静)
陈建海,张一翀,张殿英,等.肩关节钙化性肌腱炎的关节镜治疗及急慢性期疗效比较[J/CD].中华肩肘外科电子杂志,2015,3(2):95-101.
Treatment of calcifying tendonitis of shoulder with arthroscopy and comparison of efficacy
ChenJianhai,ZhangYichong,ZhangDianying,FuZhongguo,YangMing,DangYu,JiangBaoguo.
DepartmentofTraumaandOrthopedics,PekingUniversityPeople′sHospital,PekingUniversityTrafficMedicineCenter,Beijing100044,China
JiangBaoguo,Email:jiangbaoguo@vip.sina.com
Background Calcifying tendonitis of rotator cuff is a common disease that causes pain.It frequently occurs in people at 30-50s,especially in women.The acute calcifying tendonitis is characterized by persistent severe pain of shoulder joint of unknown reason.In case of severe symptoms,emergency treatment is needed.Most patients with acute phase diseases have good efficacy for conservative treatment.However,patients who do not respond to conservative treatment or with symptoms unrelieved that severely influence work and life,surgery that removes the calcifying lesion under the arthroscopy is recognized as the effective treatment.Recently,with the development of arthroscopy,removal of calcium compounds under the arthroscopy has become a common surgery and leads to good efficacy.This study was performed to assess the efficacy of removal of calcified lesion under arthroscopy for calcifying tendonitis of rotator cuff in patients with acute and chronic phases of diseases,and to determine the difference in shoulder joint function between acute and chronic phases after surgery.Methods General data:Cases with calcifying tendonitis who
treatment from September 2009 to June 2014 were included in this study.The inclusion criteria included:(1) who had history of severe shoulder joint pain; (2) who did not respond to conservative therapy; (3) who received arthroscopy.The exclusion criteria included:(1) who had complicated injury of rotator cuff; (2) who received open surgery.28 cases who met inclusion criteria were enrolled.The patients were assigned to the acute group and the chronic group by the time from the acute onset to removal of calcified lesion under arthroscopy.The acute group received removal of calcified lesion within 3 months after the onset of shoulder pain.The chronic group received removal of calcified lesion 3 months after the onset of shoulder pain that limited range of motion.28 cases had different degrees of pain and limited range of motion in the affected shoulder joint.All patients received imaging examinations.The size,shape of the calcified lesion in the shoulder joint and the shape of the acromion were determined based on the radiograph.Plain radiograph of the shoulder indicated oval or bar-shaped high-density cloudy calcification shadow in the rotator cuff below the acromion or inside the slightly lateral mucosal bursa.There were 10 cases with acute diseases in which the patients aged 38-68 years with a mean age of 52.6 years.In 5 cases,the left shoulder was affected.In 5 cases,the right shoulder was affected.The symptom was acute pain in the last 3 months.They had no previous history of obvious pain limited range of motion.The patients had acupuncture-similar feeling,increased temperature on regional skin,markedly tenderness of the shoulder and limited range of motion that severely influenced daily life before surgery.The preoperative radiograph indicated high-density calcification shadow in rotator cuff below the acromion.There were 18 chronic cases ranged from 40-73 years with a mean age of 55.5 years.7 cases had left shoulders affected and 11 cases had right shoulders affected.All patients had a history of severe pain.The pain relieved after persistence for a certain time but did not disappear.The shoulder pain was sometimes slight and sometimes severe.The range of motion of the shoulder joint was substantially limited,which influenced daily life.Surgery method:All surgeries were performed by chief or senior physicians at the Peking University Peoples’ Hospital.The cases were subject to general anesthesia on beach chair position.The bony marks were made before surgery.The arthroscopy was inserted through posterior approach to examine the glenohumeral joint.Severe inflammatory synovial hyperplasia of congestion was often observed on the wall inside the joint capsule.Some patients with limited range of motion had contracture in the rotator interval and thickened middle glenohumeral ligament.The structure of rotator cuff remained complete.The synovial tissue in the articular cavity was removed.The rotator interval and middle glenohumeral ligament were released.A needle was used to puncture the supraspinatus tendon and infraspinatus tendon through the outer edge of acromion to position the location of calcified lesion.If the calcified lesion was detected with the needle,there was calcium compound on the needle tip.After positioning of calcified lesion,it was marked with a PDS suture placed through the needle.The arthroscopy located in the subacromial space often observed obvious hyperplasia and congestion in the synovial membrane under acromion.Sometimes calcium compound was observed on the synovial membrane.The synovial membrane under the acromion was removed using shaver.The bleeding was stopped using radiofrequency coblation.The structure of rotator cuff was clearly revealed.The locations of calcified lesion were marked using sutures.The tendons were dissected along the direction of tendon fibers using blade to expose the lesion.The calcified lesion was removed with shaver.The toothpaste shaped calcium substances were observed.After complete removal of calcified lesions,the tendon of rotator cuff was observed for defectiveness.For big calcified lesions that involved 50% depth of the tendon or footprint bone surface of rotator cuff revealed,a 4.5 mm suture anchor was used to repair the rotator cuff.9 cases received repair of the rotator cuff.The osteophyte was thoroughly removed if any under the acromion.8 cases received combined acromioplasty.Postoperative rehabilitation and assessment:The affected extremity was slinged in a shoulder immobilizer.The cold pack was appropriately used within 1 week after surgery.The passive shoulder joint motion was assisted with the normal hand.The range of motion increased gradually.1 week later,the active motion was started gradually.6 weeks later,the resistance exercise and extension treatment were applied to the shoulder joint.3 months after surgery,the range of motion returned to normal and daily living activities returned to normal.For patients with combined rotator cuff repair,active exercise should start 6 weeks after the surgery to avoid loosening or another tearing on the repaired site.Each patient was assessed for Constant score,simple shoulder test (SST) score,range of motion of the shoulder joint and VAS pain score before and after surgery.Statistical method:Paired data before and after surgery was analyzed with t test.SPSS 15.0 software was used for statistical analysis.P<0.05 indicated he statistical significance.Results 28 cases were included in the retrospective study.The patients were subject to follow-up ranged from 6-33 months (with a mean of 18.8 months).The regular follow-up radiograph after surgery showed removal of calcified shadow.All patients were assessed for Constant score,VAS pain score,range of motion of the shoulder joint and simple shoulder test (SST) score before and after surgery.For 10 cases with acute phase diseases,the mean scores of Constant scale were 51.36 before treatment and 88.16 after treatment,increased by an average of 36.80.The anteflexion and uplift angle increased by about 77.00°.The external rotation increased by about 18.50°.SST questionnaire:The mean number of answers “Yes” was 5.02 before treatment and 9.32 after treatment,increased by an average of about 4.30.The mean scores for VAS were 9.12 before treatment and 4.62 after treatment,decreased by average of about 4.50.For 18 cases with acute phase diseases,the mean Constant scores were 63.70 before treatment and 88.03 after treatment,increased by an average of about 24.33.The mean number of answers “Yes” was 6.33 before treatment and 9.66 after treatment,increased by an average of about 3.33.The mean scores for VAS were 7.30 before treatment and 4.19 after treatment,decreased by an average of about 3.11.In this study,28 cases with calcifying tendonitis underwent removal of calcified lesion under arthroscopy and presented different degrees of function improvement in shoulder joint.The patients with calcifying tendonitis in the acute group had significantly better Constant score,SST growth and anteflexion and uplift angle and pain relief than the patients in the chronic group (P<0.05).In this study,9 cases received repair of rotator cuff,including 2 cases in the acute group,accounting for 20% of patients with acute phase diseases,and 7 cases in the chronic group,accounting for 38.9% of patients with chronic phase diseases.Discussion Calcifying tendonitis of rotator cuff is a common disease that causes acute shoulder pain.When the symptom severely influences daily life and conservative therapy is not effective,early removal of calcified lesion under the arthroscopy is effective for calcifying tendonitis and leads to good prognosis.
Shoulder joint;Tendinopathy;Arthroscopy;Treatment
10.3877/cma.j.issn.2095-5790.2015.02.006
国家自然科学基金(31371210);教育部创新团队项目(IRT1021);卫生公益性产业科研专项基金(201002014)
100044北京大学人民医院创伤骨科 北京大学交通医学中心
姜保国,Email:jiangbaoguo@vip.sina.com
2015-05-16)
