肱骨头内翻畸形导致肱骨近端骨折内固定失败的生物力学研究
2015-06-24白露张洪雷陈鹏李伟江长青张文涛
白露 张洪雷 陈鹏 李伟 江长青 张文涛
·论著·
肱骨头内翻畸形导致肱骨近端骨折内固定失败的生物力学研究
白露 张洪雷 陈鹏 李伟 江长青 张文涛
目的 探讨肱骨头内翻状态下锁定钢板固定肱骨近端骨折内固定失败的生物力学原因。方法 采用防腐处理肱骨标本6对,经肱骨外科颈截骨制作肱骨近端骨折模型。根据不同临床情况分为力线正常组和肱骨头内翻组。通过循环轴向压缩试验(5 000次)和静态轴向压缩破坏试验对两组骨折内固定模型进行生物力学测试。结果 在循环轴向压缩试验早期,肱骨头内翻组骨折块间隙移位与力线正常组差异无统计学意义(P>0.05)。在循环压缩3 000次后,肱骨头内翻组骨折端移位明显高于力线正常组。在破坏力学实验中,肱骨头内翻组内固定失败所需载荷明显小于力线正常组(t=3.812,P=0.003)。内固定失败轴向最大移位,力线正常组明显高于肱骨头内翻组(t=2.994,P=0.013)。结论 肱骨头内翻畸形显著降低了肱骨近端骨折锁定钢板内固定系统的稳定效能。
肱骨骨折,近端;肱骨头;内翻畸形;锁定钢板
肱骨近端骨折是创伤骨科常见疾病,由于肱骨近端骨密度随着年龄增长而逐渐降低,故肱骨近端骨折在中老年人群中更为常见,其发生率约为全身骨折的5%[1]。而随着社会老龄化进程,肱骨近端骨折的发生率有增高的趋势[2]。近20年来,不稳定肱骨近端骨折的手术治疗方法有了较大变化。即由以往经皮穿针固定、普通钢板逐渐转变为以“内固定支架”为主流的锁定钢板固定。由于锁定钢板板钉之间“一体化”,加之多个方向的锁定螺钉可以从不同角度对肱骨头进行把持,故无论在临床实践还是生物力学研究中,其相对于普通钢板的优势均得到了很好的体现[3-4]。
随着锁定钢板大规模应用于治疗肱骨近端骨折,一些中长期的临床随访资料表明,在内侧皮质缺损的2部分或3部分肱骨近端骨折病例中出现了骨折复位丢失、肱骨头内翻畸形和继发内固定失败[5-7]等现象。临床队列研究发现,该类并发症多表现为内侧皮质缺损伴有肱骨头内翻畸形相关,并随着时间的推移继而出现肱骨头内翻脱出,螺钉断裂或钢板断裂[8-11]。从生物力学角度讲,肱骨近端缺少内侧皮质的力学支撑是潜在的不稳定因素。但并非所有伴内侧皮质缺损者都出现内固定失败,并且内固定失败的类型也各不相同。那么,肱骨头内翻是否为内固定失败的又一危险因素?我们从生物力学的角度研究肱骨头内翻畸形与锁定钢板治疗肱骨近端骨折后内固定失败的相互关系。
材 料 与 方 法
一、标本处理与骨折模型的建立
取6对防腐处理的成人肱骨标本(标本来自深圳大学医学院解剖学系),拍片检查排除骨病、陈旧骨折等病理情况。在力学实验前于-20 ℃冷藏,待进行力学实验时于室温(18 ℃)下解冻8 h。解冻过程中喷洒生理盐水以免标本干燥。
将每对标本随机取左右侧,入组肱骨头内翻组和力线正常组并制作骨折模型。骨折模型在X-Y工作台上完成。首先统一对肱骨标本自近端截取20 cm。使用摆锯在肱骨干骺端与肱骨头移行的外科颈处平行于肱骨头顶点切线位截骨。截骨时保留肱骨近端外侧大结节部周径皮质的1/3,以便PHILOS钢板打入。截骨面之间骨折间隙为10 mm。肱骨头内翻畸形的制备按照Voigt等[12]的方法:在X-Y工作台上通过角度测量尺将肱骨头内翻20°。所有骨折均采用Synthesis PHILOS五孔锁定钢板进行固定。按照AO组织推荐方法:将钢板放置于大结节上,距离结节间沟5~8 mm,距离大结节顶部8~10 mm处,均固定PHILOS钢板近端A、B、C、D、E孔。远端使用3枚锁定螺钉固定。所有螺钉均采用3.5 mm锁定螺钉。
二、力学实验流程
1.标本的固定与测试方法:力学实验在Instron 8874(2 kN,±1%)力学试验机上进行(图1)。骨折模型固定于试验机工作台,肱骨干轴线与力学试验机压头垂直。轴向压缩的力学压头内使用骨水泥预塑形,使之与肱骨头外形相适配,避免加压过程中部分区域应力集中导致肱骨头表面破坏。循环轴向压缩实验条件:最小压力50 N,最大压力300 N,允许的最大移位5 mm,测试循环数5 000次。实验得到的生物力学曲线以移位-载荷曲线表示。
2.内固定失败的判定:在循环轴向加压实验中,如每一例实验标本数据曲线的变化均在弹性变量的曲线范围以内,认定其为内固定失败。在破坏力学实验中,实时观测力学试验机移位-载荷曲线。在破坏力学实验中,以移位-载荷曲线出现趋于移位零点的“拐点”为内固定失败。内固定失败后不再进行力学测量,取下标本观察内固定失败类型并记录。
图1 Instron力学实验机及实验图片
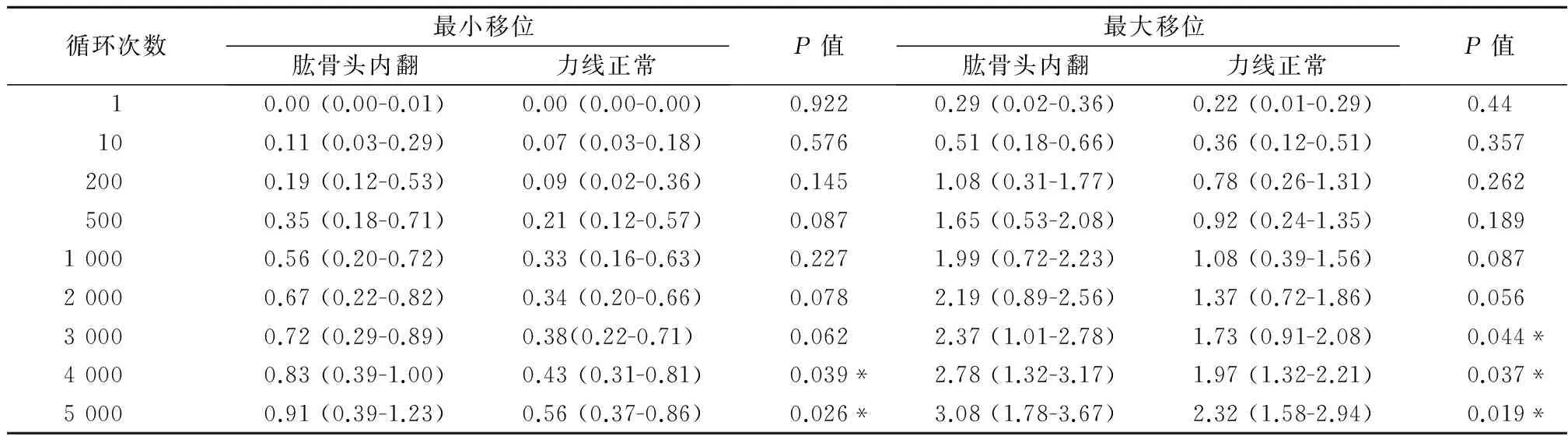
循环次数最小移位肱骨头内翻力线正常P值最大移位肱骨头内翻力线正常P值10.00(0.00-0.01)0.00(0.00-0.00)0.9220.29(0.02-0.36)0.22(0.01-0.29)0.44100.11(0.03-0.29)0.07(0.03-0.18)0.5760.51(0.18-0.66)0.36(0.12-0.51)0.3572000.19(0.12-0.53)0.09(0.02-0.36)0.1451.08(0.31-1.77)0.78(0.26-1.31)0.2625000.35(0.18-0.71)0.21(0.12-0.57)0.0871.65(0.53-2.08)0.92(0.24-1.35)0.18910000.56(0.20-0.72)0.33(0.16-0.63)0.2271.99(0.72-2.23)1.08(0.39-1.56)0.08720000.67(0.22-0.82)0.34(0.20-0.66)0.0782.19(0.89-2.56)1.37(0.72-1.86)0.05630000.72(0.29-0.89)0.38(0.22-0.71)0.0622.37(1.01-2.78)1.73(0.91-2.08)0.044*40000.83(0.39-1.00)0.43(0.31-0.81)0.039*2.78(1.32-3.17)1.97(1.32-2.21)0.037*50000.91(0.39-1.23)0.56(0.37-0.86)0.026*3.08(1.78-3.67)2.32(1.58-2.94)0.019*
注:测量值平均数 *P<0.05
三、统计学分析

结 果
一、循环力学结果
在轴向载荷5 000次中,6对标本均未出现内固定失败。在轴向循环压力检测中,肱骨头内翻组在2 000次以内的轴向压缩中,最小移位和最大移位均较力线正常组大,但差异无统计学意义(P>0.05)。在循环轴向加压3 000次肱骨头内翻组平均最大移位为2.37 mm (1.01~2.78),较力线正常组1.73 mm(0.91~2.08)差异有统计学意义(P=0.044)。在循环轴向加压4 000次后,肱骨头内翻组最小移位(P=0.039)与最大移位(P=0.037)均明显高于力线正常组。在循环轴向加压5 000次时。肱骨头内翻组平均最小移位为0.91 mm (0.39~1.23),平均最大移位为3.08 mm (1.78~3.67)。力线正常组则分别为0.56 mm(0.37~0.86)和2.32 mm(1.58~2.94),其平均最小移位(P=0.026)和平均最大移位(P=0.019)均明显小于肱骨头内翻组。见表1。
二、破坏力学实验结果
在标本完成循环载荷实验后,即刻进行破坏力学实验。力线正常组平均破坏载荷(870±104) N,内翻畸形组为(632±111) N。组间比较差异有统计学意义(t=3.812,P=0.003)。内固定失败时力线正常组平均骨折间隙移位为(6.72±0.71) mm,肱骨头内翻组为(5.67±0.53) mm组间比较差异有统计学意义(t=2.994,P=0.013),见表2和图2。
讨 论
近10年来,肱骨近端骨折在治疗理念上完成了由过去的“T型钢板+松质骨螺钉内固定”向“角度稳定的锁定钢板内固定”的转变。在锁定钢板将稳定固定的问题推上了新高度的同时,复位丢失和内翻畸形成为了临床关注的另一焦点。在以往使用普通钢板固定骨折时,由于肱骨头内骨量不足,肱骨近端生物力学的不稳定往往导致螺钉松动脱出,或者螺钉难以把持肱骨头,与肱骨头之间不断出现相对活动,最终造成螺钉松动,内固定失败。当锁定钢板固定虽然改善了固定物对骨质疏松骨的把持力,但同时也出现了不同于以往的内固定失败的类型:肱骨头内翻,内固定螺钉不能把持肱骨头;或内固定钢板或螺钉自肱骨大结节外侧壁处断裂,而有的病例即使使用了肱骨距螺钉也依然出现内固定失败[13-15]。肩关节虽为非负重关节,但由于肩胛带周围肌肉的张力作用,肱骨头仍对关节盂有一定的应力。在体生物力学研究表明:肩关节在静息状态下盂肱关节面的受力方向为与肱骨头轴线在冠状面成角大约22.5°~23°,在矢状面成角40°左右。且该致畸力量达到整个体重的1/3~1/2。在术后7个月,肩关节正常状态下外展时肱骨头受力约为整个体重的1.1倍;肩关节上举时受力约为整个体重的1.3倍[16]。正因如此,肱骨近端骨折内固定系统处于上述应力中,如存在其他不稳定因素如复位不良、骨缺损等,则有可能内固定系统出现应力集中或局部松动,从而出现内固定失败。
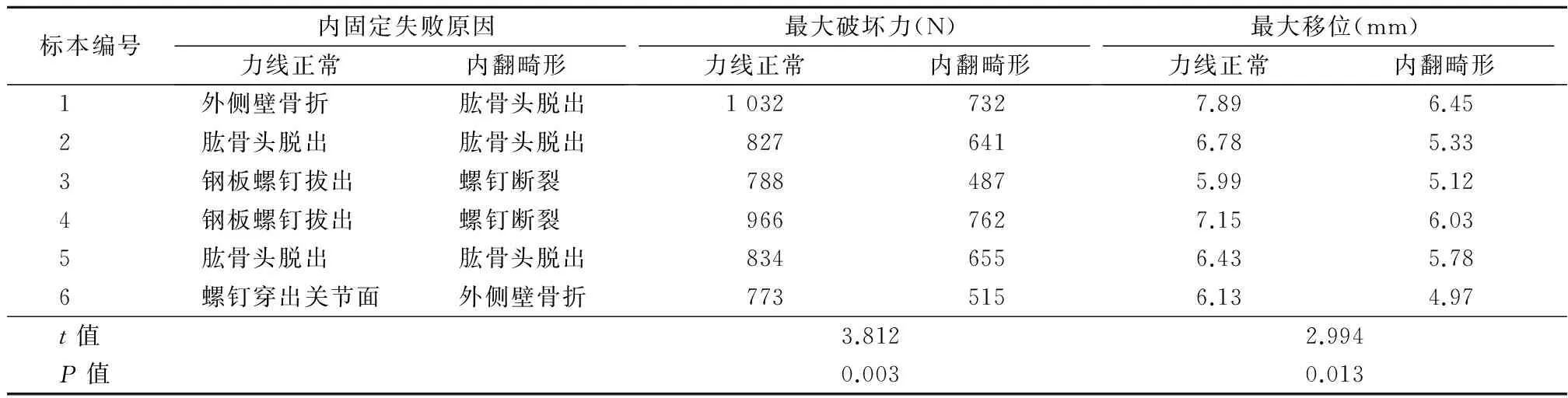
表2 各组标本破坏力学实验数据
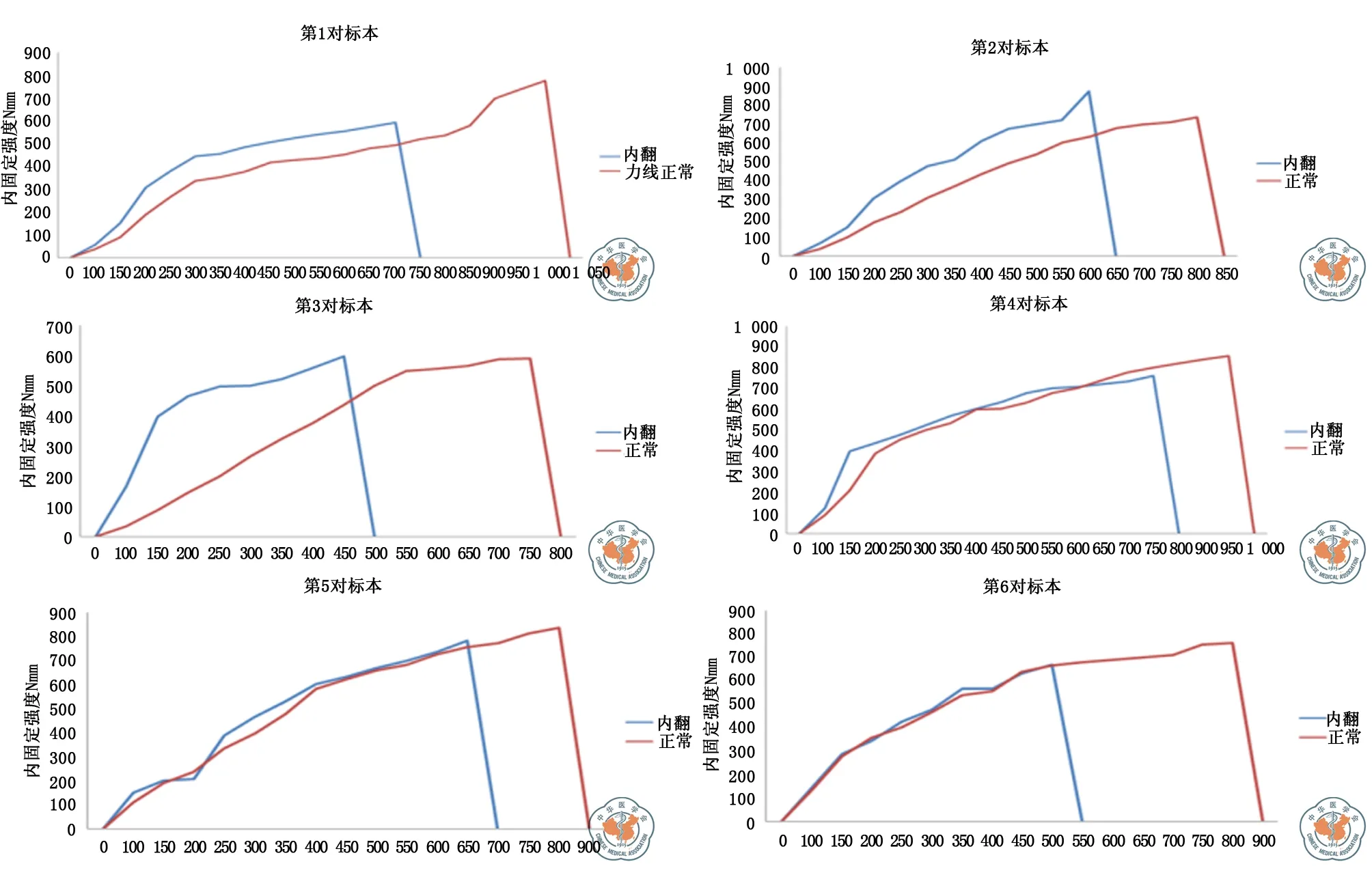
注:蓝色曲线代表内翻畸形标本,红色曲线代表正常对照标本,在相同轴向载荷加载过程中,骨折间隙的移位随着载荷增加而增大,在标本内固定系统失败时达到曲线拐点图2 6对标本的移位-载荷曲线
在肱骨近端骨折内固定生物力学研究中,内侧皮质缺损与复位丢失的相互关系及病理生理变化均已经得到阐明[15,17-19]。但内翻畸形与内固定失败的关系尚不完全明了。Lescheid等[20]对缺少内侧皮质支撑的肱骨近端骨折进行的破坏生物力学测试。结果显示:无内侧皮质支撑的肱骨近端骨折更加容易移位,具有冠状面(旋转)和矢状面(内翻)的不稳定。虽然内侧皮质缺损已被证实是导致肱骨近端骨折术后复位丢失的重要原因,但在内侧支撑不稳定的力学条件下,肱骨头出现了怎样的致畸移位,而该过程是否能继发内固定失败也未得到完全阐明。Voigt等[12]证明,内翻状态下的肱骨近端骨折在力学构型上更加不稳定,但并未对内翻是如何影响肱骨近端内固定的动态稳定进行研究。在本研究中,肱骨头固定于内翻畸形状态较力线正常组在轴向压力下更容易出现骨折间隙的移位[(6.72±0.71) mm VS (5.67±0.53) mm,t=2.994,P=0.013]。而就内固定系统的稳定性而言,内翻畸形内固定破坏强度显著低于力线正常组[(870±104) N VS (632±111) N,t=3.812,P=0.003]。由于肱骨头位于肱骨近端所受应力的偏心位,而内翻则可能增加致畸作用的力臂,从而使得肱骨头处于不稳定的力学状态。
临床报道的肱骨近端骨折锁定钢板术后内固定失败者大致可分为两种:(1)肱骨头内翻畸形,骨折端不愈合或畸形愈合。此时,由于肱骨头的内翻,锁定螺钉相对于肱骨头位置发生变化,出现螺钉穿出关节面。(2)内侧皮质缺损较大,肱骨头内侧缺乏有效的力学支撑,肱骨头内翻的致畸力作用于锁定钢板,导致内固定疲劳,钢板断裂或钢板螺钉锁定部位断裂[12,14,21-22]。在本研究的动态力学实验中,随着循环载荷的增加,内翻畸形组骨折端移位明显高于力线正常组。这有可能解释上述临床情况:内翻带来的内固定系统的不稳定,而不稳定的骨折端又成为内固定系统的骨-螺钉界面的薄弱环节。使得骨折端不能得到稳定的力学环境而影响愈合。由于锁定钢板固定是一种整体稳定,即肱骨头内打入的锁定螺钉与钢板为一整体,所以在肱骨头渐进性内翻畸形的过程中,位于肱骨近端外侧壁的钢板受的是偏心作用力,应力集中于肱骨-锁定钢板的外侧,从而可能导致钢板或钢板螺钉锁定部位在反复多次的集中应力作用下出现断裂。如钢板未发生断裂,肱骨头畸形移位,螺钉钉道扩大,出现继发性螺钉穿出。
就本研究而言,由于内翻成角,肱骨近端的主要承力结构(内侧皮质)并非处于解剖复位状态,而由于内侧支撑的缺失,肱骨头在应力作用下更容易出现内翻的倾向。作为偏心固定的锁定钢板,压力侧的支撑缺损必然会引起张力侧的应力集中。故临床多见肱骨头内翻畸形后继发锁定钢板在外科颈骨折线水平断裂。
肩关节虽为非负重关节,但从本实验来看,肱骨近端骨折术后内固定失败也难以用经典的“负重→内固定失效或骨折局部应力集中→骨折端过度活动→复位丢失→内固定失效”理论来解释。但本研究尚有不足:(1)未能测量各组标本的骨密度,没有将骨密度作为另一个考证参数印证其与内固定失败的关系。(2)本研究仅测量了肱骨近端在致畸作用力下轴向移位,而未能对旋转稳定进行研究。也就是说,内翻的肱骨头在三维平面内的致畸移位与肱骨近端内固定失败的关系仍需进一步的实验探索。
[1] Kannus P,Palvanen M,Niemi S,et al.Rate of proximal humeral fractures in older Finnish women between 1970 and 2007[J].Bone,2009,44(4):656-659.
[2] Bell JE,Leung BC,Spratt KF,et al.Trends and variation in incidence,surgical treatment,and repeat surgery of proximal humeral fractures in the elderly[J].J Bone Joint Surg Am,2011,93(2):121-131.
[3] Brunner F,Sommer C,Bahrs C,et al.Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate:a prospective multicenter analysis[J].J Orthop Trauma,2009,23(3):163-172.
[4] Miller DL,Goswami T.A review of locking compression plate biomechanics and their advantages as internal fixators in fracture healing[J].Clin Biomech,2007,22(10):1049-1062.
[5] Zhang L,Zhang JY,Wang WL,et al.The clinical benefit of medial support screws in locking plating of proximal humerus fractures:a prospective randomized study[J].Int Orthop,2011,35(11):1655-1661.
[6] Robinson CM,Wylie JR,Ray AG,et al.Proximal humeral fractures with a severe varus deformity treated by fixation with a locking plate[J].J Bone Joint Surg Br,2010,92(5):672-678.
[7] Lanting B,Macdermid J,Drosdowech D,et al.Proximal humeral fractures:a systematic review of treatment modalities[J].J Shoulder Elbow Surg,2008,17(1):42-54.
[8] Agudelo J,Schürmann M,Stahel P,et al.Analysis of efficacy and failure in proximal humerus fractures treated with locking plates[J].J Orthop Trauma,2007,21(10):676-681.
[9] Osterhoff G,Ossendorf C,Wanner GA,et al.The calcar screw in angular stable plate fixation of proximal humeral fractures--a case study[J].J Orthop Surg Res,2011,24(6):50.
[10] Gardner MJ,Weil Y,Barker JU,et al.The importance of medial support in locked plating of proximal humerus fractures[J].J Orthop Trauma,2007,21(3):185-191.
[11] 吴克俭,王晓宁,张建,等.复杂肱骨近端骨折[J/CD].中华肩肘外科电子杂志,2014,2(4):209-218.
[12] Voigt C,Kreienborg S,Megatli O,et al.How does a varus deformity of the humeral head affect elevation forces and shoulder function? A biomechanical study with human shoulder specimens[J].J Orthop Trauma,2011,25(7):399-405.
[13] Ockert B,Pedersen V,Geyer L,et al.Position of polyaxial versus monoaxial screws in locked plating for proximal humeral fractures:analysis of a prospective randomized study[J].Eur J Orthop Surg Traumatol,2014,24(5):747-752.
[14] Clavert P,Adam P,Bevort A,et al.Pitfalls and complications with locking plate for proximal humerus fracture[J].J Shoulder Elbow Surg,2010,19(4):489-494.
[15] Bai L,Fu Z,An S,et al.The Effect of Calcar Screw Use in Surgical Neck Fractures of the Proximal Humerus with Unstable Medial Support:A Biomechanical Study[J].J Orthop Trauma,2014,28(8):452-457.
[16] Bergmann G,Graichen F,Bender A,et al.In vivo glenohumeral contact forces--measurements in the first patient 7 months postoperatively[J].J Biomech,2007,40(10):2139-2149.
[17] Südkamp NP,Audigé L,Lambert S,et al.Path analysis of factors for functional outcome at one year in 463 proximal humeral fractures[J].J Shoulder Elbow Surg,2011,20(8):1207-1216.
[18] Sproul RC,Iyengar JJ,Devcic Z,et al.A systematic review of locking plate fixation of proximal humerus fractures[J].Injury,2011,42(4):408-413.
[19] 白露,张文涛,江长青,等.内侧皮质缺损对肱骨近端骨折锁定钢板内固定轴向稳定性影响的生物力学研究[J/CD].中华肩肘外科电子杂志,2014,2(2):75-79.
[20] Lescheid J,Zdero R,Shah S,et al.The biomechanics of locked plating for repairing proximal humerus fractures with or without medial cortical support[J].J Trauma,2010,69(5):1235-1242.
[21] Lever JP,Aksenov SA,Zdero R,et al.Biomechanical analysis of plate osteosynthesis systems for proximal humerus fractures[J].J Orthop Trauma,2008,22(1):23-29.
[22] Ring D.Current concepts in plate and screw fixation of osteoporotic proximal humerus fractures[J].Injury,2007,38(Suppl 3):S59-S68.
(本文编辑:李静)
白露,张洪雷,陈鹏,等.肱骨头内翻畸形导致肱骨近端骨折内固定失败的生物力学研究[J/CD].中华肩肘外科电子杂志,2015,3(2):74-80.
Biomechanical study of failed internal fixation for proximal humerus fractures caused by varus deformity of humeral head
BaiLu,ZhangHonglei,ChenPeng,LiWei,JiangChangqing,ZhangWentao.
DepartmentofSportsMedicine,PekingUniversityShenzhenHospital,Shenzhen518000,China
ZhangWentao,Email:zhangwt2007@sina.cn
Background Proximal humerus fracture (PHF) is a common disease in the traumatic orthopedics due to decreased density of bone in the proximal humerus with age.It occurs more often in the medium-and old-age people,accounting for 5% of fractures.With the process of aging population,the incidence of PHF tends to increase.In recent 20 years,the surgery methods of unstable PHF change greatly from the percutaneous fixation and common plate for fractures to locking plate fixation with "internal fixator" as mainstay.As the locking plate is widely used for PHF,some medium-and long-term clinical follow-up data indicated loss of reduction of fracture,varus deformity of humeral head,and secondary internal fixation failure were found in PHF cases with two or three sites of defective medial cortex.These complications are characterized by defective medial cortex and varus deformity of humeral head.Over time,it causes varus and prolapsed of humeral head,breakage of screws or plate.From biomechanics,the loss of support for proximal humerus by the medial cortex is an unstable factor.But not all cases with defective medial cortex develop internal fixation failure.The types of internal fixation failure vary in patients.Is the varus deformity of humerus head another risk factor for internal fixation failure? This study investigated the relationship between the varus deformity of humeral head and the internal fixation failures after locking plate treatment for PHF from the biomechanics.Methods Sample treatment and establishment of fracture model:6 pairs of adult humeral samples with antiseptic treatment were obtained from the anatomy department of the Shenzhen University-affiliated Medical School.The pathological symptoms such as bone disease and chronic fracture were excluded by radiograph.The samples were stored at -20 ℃ before biomechanical study and thawed at room temperature (18 ℃) for 8 h when the biomechanical study was about to start.During thawing,samples were sprayed with normal saline to prevent drying.Either right or left side of the samples was randomly assigned to the varus deformity group and normal alignment group to establish the fracture model.The fracture model was established on the X-Y workbench.First,20 cm was removed from the proximal ends of all samples.The osteotomy was performed in parallel with the vertex tangent of the humeral head at the surgical neck on the junction between humeral metaphysis and the humeral head using oscillating saw.The cortex of the lateral greater tuberosity in proximal humerus was reserved at an amount accounting for 1/3 of the perimeter,which helped to insert the PHILOS plate.The fracture gap between the osteotomy surfaces was 10 mm.The varus deformity of humeral head was prepared using the method described by Voigt et al.The varus of humeral head by 20° was measured using gauge on the X-Y workbench.All fractures were fixed using 5-hole Synthesis PHILOS locking plate.According to recommendation by the AO Organization,the plate was placed on the greater tuberosity 5-8 mm away from the intertubercular sulcus,8-10 mm away from the greater tuberosity tip.The PHILOS plate was fixed in holes A,B,C,D and E.Three locking screws were used to fix the distal end.All screws were 3.5 mm locking screws.Procedures of mechanical study:Fixation and testing of samples:The mechanics study was performed on the Instron 8874 (2 kN,±1%) mechanical tester.The fracture model was fixed at the workbench of the tester.The axis of the humeral shaft was vertical to the pressure head of the mechanical tester.The pre-moulding for mechanical pressure head in the axial compression was prepared using bone cement,which was matched for the shape of humeral head to avoid damage of the surface of humeral head at the area with concentrating stress during compression.The circular axial compression experiment was performed under the following conditions:minimum pressure of 50 N,maximum pressure of 300 N,permitted maximum displacement of 5 mm,cycle number of 5,000.The biomechanical curve was expressed by displacement-load curve.Determination of internal fixation failure:In the axial compression experiment,the sample was regarded as internal fixation failure if the variation of the data curve of each sample was within the range of the curve for flexible variables.In the damage mechanical experiment,real-time displacement of mechanical tester-load curve was observed.In the damage mechanical experiment,the presence of inflection point on the displacement-load curve when the displacement curve tended to be zero indicated failure of internal fixation.The mechanical measurement was stopped after failure of internal fixation.The samples were removed for observation.The types of internal fixation were recorded.Statistical analysis:The statistical analysis was performed using PASW18.0 (SPSSInc IBM Chicago,USA).The measurement data was expressed as±s.The difference of maximum load to damage internal fixation in different groups was compared using student t test.The differences in the maximum and minimum displacement of circular mechanics between the varus group and alignment normal group were compared using Mann Whitney-Wilcoxon.The independent-sample test was performed for comparison of differences in maximum damage load and maximum displacement of the samples with internal fixation failure between groups.P<0.05 indicated statistical significance.Results (1)Results of circular mechanics:In 5,000 axial compressions,6 pairs of samples did not show internal fixation failure.In measurement of the pressure during axial cycles,the varus group had greater minimum and maximum displacements than the normal alignment group within 2,000 cycles of axial compression,although no significant difference was found (P>0.05).The mean maximum displacement in the varus group was 2.37 mm (1.01-2.78) at 3,000 cycles of axial compression,significantly different from 1.73 mm (0.91-2.08) in the normal alignment group (P=0.044).After 4,000 cycles of axial compression,the varus group had significantly higher minimum displacement (P=0.039) and maximum displacement (P=0.037) than the normal alignment group.After 5,000 cycles of axial compression,the varus group had a mean minimum displacement of 0.91 mm (0.39-1.23) and a mean maximum displacement of 3.08 mm (1.78-3.67).The normal alignment group had a mean minimum displacement of 0.56 mm (0.37-0.86) and a mean maximum displacement of 2.32 mm (1.58-2.94).The normal alignment group had significantly lower mean minimum displacement (P=0.026) and mean maximum displacement (P=0.019) than the normal alignment group.(2) Results of damage mechanics:The damage mechanical experiment was performed immediately after the circular load experiment.The mean damage loads were 870±104 N for the normal alignment group and 632±111 N for the varus deformity group.There was significant difference between two groups (t=3.812,P=0.003).In cases with internal fixation failure,the mean fracture gap displacements were 6.72±0.71 mm for the normal alignment group and 5.67±0.53 mm for the varus group.There was significant difference between the two groups (t=2.994,P=0.013).Conclusion The varus deformity of the humeral head significantly lowered the stabilization performance of the locking plate internal fixation system for the PHF.
Humral fracture,proximal;Humral head;Inversion deformity;Locking plate
10.3877/cma.j.issn.2095-5790.2015.02.002
深圳市卫生计生系统科研项目(201402027)
518000北京大学深圳医院运动医学科
张文涛,Email:zhangwt2007@sina.cn
2015-03-16)
