HbA1c水平对PCI术后冠心病伴糖尿病患者心血管不良事件的影响
2015-02-19网络出版时间20150113网络出版地址httpwwwcnkinetkcmsdetail525012201501131930028html
网络出版时间:2015-01-13 网络出版地址:http://www.cnki.net/kcms/detail/52.5012.R.20150113.1930.028.html
李 源, 房 卿, 周庆元
(陕西汉中中航工业3201医院 呼吸科, 陕西 汉中 723000)
HbA1c水平对PCI术后冠心病伴糖尿病患者心血管不良事件的影响
网络出版时间:2015-01-13网络出版地址:http://www.cnki.net/kcms/detail/52.5012.R.20150113.1930.028.html
李源, 房卿, 周庆元
(陕西汉中中航工业3201医院 呼吸科, 陕西 汉中723000)
[摘要]目的: 探讨糖化血红蛋白(HbA1c)水平与经皮冠状动脉介入治疗(PCI)术后冠心病(CHD)伴糖尿病患者心血管不良事件(MACE)发生率的关系。方法: 行PCI治疗的CHD患者83例,根据入组患者的HbA1c水平将其分为A、B两组,A组(HbA1c<6.5%) 38例, B组(HbA1c≥6.5%)45例,比较两组患者资料、术前术前C反应蛋白(CRP)、血沉(ESR)、肿瘤坏死因子(TNF-α)及白介素6(IL-6)水平、观察2组经PCI治疗后6和24月MACE发生率。结果: A组患者术前的CRP、TNF-α水平均显著低于B组(t=5.944、5.095,P<0.01),两组ESR及IL-6差异无统计学意义(P>0.05);治疗6月后,A、B两组患者MACE结果差异无统计学意义(P>0.05);治疗24月后A组患者出现心梗、病变血管再狭窄的比例均低于B组,差异有统计学意义(χ2=5.385、6.629,P=0.020、0.010)。结论: PCI术后,与高HbA1c患者比较,HbA1c水平低的CHD伴糖尿病患者的预后较好。
[关键词]冠心病; 糖尿病; 心血管疾病; 糖化血红蛋白; 经皮冠状动脉介入
冠心病伴糖尿病患者的血糖水平会影响患者的死亡率和发生率产生[1]。糖化血红蛋白(HbA1c)是糖尿病检测的金标准,HbA1c能够对测量前2~3个月的血糖的平均水平进行准确地反映,与糖尿病并发症有密切关系[2-3]。本研究旨在探讨HbA1c水平与经皮冠状动脉介入治疗(PCI)术后冠心病(CHD)伴糖尿病患者心血管不良事件(MACE)发生率的关系。
1对象与方法
1.1研究对象选择2011-2012年心内科就诊的83例接受PCI治疗的CHD伴糖尿病患者,符合1997年美国糖尿病协会(ADA)2型糖尿病诊断糖尿病标准,症状、体征、冠脉造影结果明确为CHD。排除标准:已经确诊为主动脉夹层、其它非心源性因素导致胸痛以及肺动脉栓塞,经PCI手术后未能显著缓解或者消失心绞痛的症状,需在造影后进行主动脉—冠状动脉旁路移植术及未在造影后植入支架者。根据入组患者的HbA1c水平分为两组:A组(HbA1c<6.5% )38例,平均(64.3±11.6)岁; B组(HbA1c≥6.5%)45例,平均(62.4±13.4)岁。两组年龄、性别等资料相比,差异无统计学意义(P<0.05)。
1.2方法抽取2组患者空腹静脉抗凝全血,使用美国BIO-RADD-10TM型糖化血红蛋白仪测定HbA1c。采用ELISA法测定患者术前血清C反应蛋白(CRP)、血沉(ESR)、肿瘤坏死因子(TNF-α)及白介素6(IL-6)水平。
1.3观察指标观察2组患者HbA1c、CRP、ESR、TNF-α及IL-6,随访治疗后6和24月后MACE(死亡、心梗、支架内血栓、病变血管出现再狭窄)发生率。

2结果
2.1术前炎性指标两组CHD伴糖尿病患者术前炎性指标比较,A组患者术前的CRP、TNF-α水平均低于B组,差异有统计学意义(P<0.05),见表1。

表1 两组CHD伴糖尿病患者PCI术前的
2.2治疗6月、24月MACE发生率治疗6月后 A、B两组CHD伴糖尿病患者MACE发生率比较,差异无统计学意义(P>0.05);治疗24月后,A组出现心梗、病变血管再狭窄病例均低于B组,差异具有统计学意义(P<0.05),见表2。
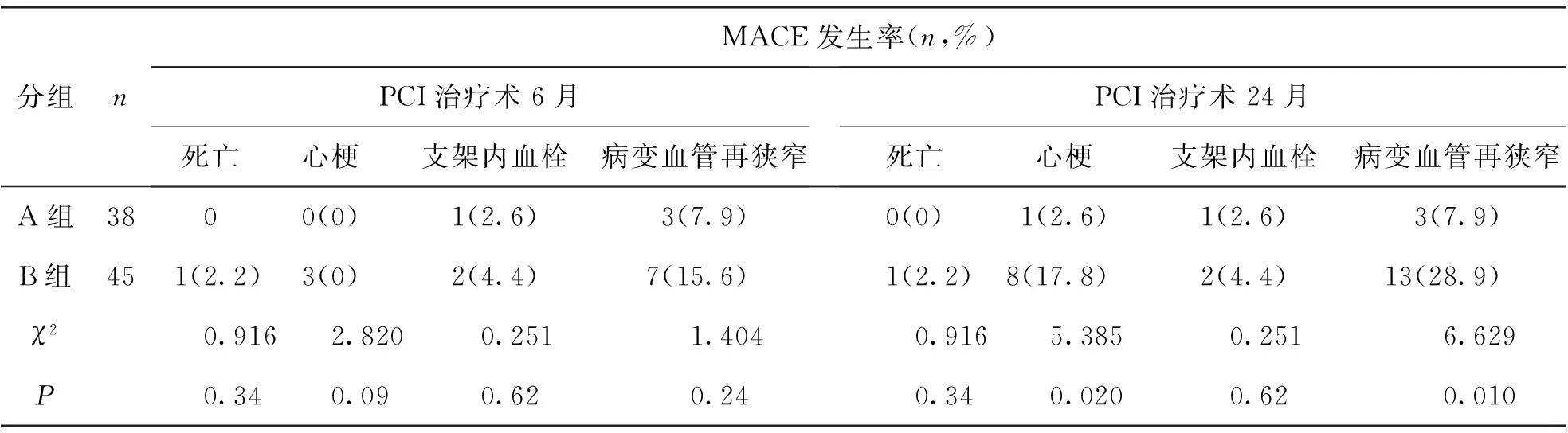
表2 两组CHD伴糖尿病患者PCI治疗术6月后MACE发生率
3讨论
随着介入诊疗技术发展,PCI已经成为一种治疗CHD最有效的方法,但CHD伴高血糖症会使各种类型的CHD患者PCI手术后血栓、心梗等并发症的发生率上升[4-6]。在CHD患者中,女性糖尿病发病率是非CHD患者的5倍,男性糖尿病发病率是非CHD患者的2倍[7]。严格控制患者的血糖水平,可以降低糖尿病并发症的发生,HbA1c虽然可以评价糖尿病患者体内血糖控制的情况,但只能反映2~3个月的血糖平均水平,而没能对血糖变化的频率以及程度进行精确反映[8]。但患者用餐后血糖往往处于高、低交替状态,而HbA1c仍处在一个较低水平的状态,不能反映患者当时的水平[9]。研究还发现,单纯以HbA1c预测CHD伴糖尿病患者MACE仍有局限性[10]。提示临床中在监测HbA1c时,还应对患者血糖进行检测。本研究以CHD伴糖尿病患者行PCI术前HbA1c水平进行分组,结果发现HbA1c水平越高,相对应的血液炎性介质水平也越高,提示冠心病患者机体的炎症反应与糖尿病的病程进展有着一定的相关性[11]。PCI术后CHD合并糖尿病的患者HbA1c高水平组,MACE发生率高于HbA1c低水平组,说明HbA1c高水平组行PCI治疗后的远期疗效(24个月)低于HbA1c低水平组。提示HbA1c水平低的CHD伴糖尿病患者PCI治疗的预后好于HbA1c水平高者,
参考文献4
[1]Lerchbaum E, Schwetz V, Giuliani A et al. Assessment of glucose metabolism in polycystic ovary syndrome: HbA1c or fasting glucose compared with the oral glucose tolerance test as a screening method[J]. Hum Reprod, 2013(9):2537-2544.
[2]Pischon T, Hu FB, Girman CJ, et al. Plasma total and high molecular weight adiponectin levels and risk of coronary heart disease in women[J]. Atherosclerosis, 2011(1):322-329.
[3]Nielsen BM, Nielsen MM, Jakobsen MU, et al. A cross-sectional study on trans-fatty acids and risk markers of CHD among middle-aged men representing a broad range of BMI[J]. Br J Nutr, 2011(8):1245-1252.
[4]Carter P, Achana F, Troughton J et al. A Mediterranean diet improves HbA1c but not fasting blood glucose compared to alternative dietary strategies: a network meta-analysis[J]. J Hum Nutr Diet, 2014(3):280-297.
[5]Fharm E, Cederholm J, Eliasson B, et al. Time trends in absolute and modifiable coronary heart disease risk in patients with Type 2 diabetes in the Swedish National Diabetes Register (NDR) 2003-2008[J]. Diabet Med, 2012(2):198-206.
[6]Suljic E, Kulasin I, Alibegovic V. Assessment of Diabetic Polyneuropathy in Inpatient Care: Fasting Blood Glucose, HbA1c, Electroneuromyography and Diabetes Risk Factors[J]. Acta Inform Med, 2013(2):123-126.
[7]刘晓桥, 杨天和, 张陈匀, 等. 不同临床类型冠心病介入术后Hs-CRP的变化规律[J]. 贵阳医学院学报, 2007(5):492-495.
[8]Hwang JY, Park JE, Choi YJ et al. Carbohydrate intake interacts with SNP276G>T polymorphism in the adiponectin gene to affect fasting blood glucose, HbA1C, and HDL cholesterol in Korean patients with type 2 diabetes[J]. J Am Coll Nutr, 2013(3):143-150.
[9]张科, 谭红霞, 卢建刚. 老年冠心病患者PCI后hs-CRP和脑钠肽水平改变[J]. 贵阳医学院学报, 2014(1):67-69.
[10]Rajan P, Nera M, Pavalura AK, et al. Comparison of glycosylated hemoglobin (HbA1C) levels in patients with chronic periodontitis and healthy controls[J]. Dent Res J (Isfahan), 2013(3):389-393.
[11]Rasmussen NH, Smith SA, Maxson JA, et al. Association of HbA1c with emotion regulation, intolerance of uncertainty, and purpose in life in type 2 diabetes mellitus[J]. Prim Care Diabetes, 2013(3):213-221.
[12]闫兴国,王锋,刘杰,等.急性心肌梗死溶栓再通与糖化血红蛋白的关系[J].实用临床医药杂志, 2014(3):84-85.
(2014-09-11收稿,2014-11-28修回)
中文编辑: 吴昌学; 英文编辑: 刘华
The Effect of HbA1c Level on the Incidence of MACE in Postoperative
Patients of CHD & DM after PCI Therapy
LI Yuan, FANG Qing, ZHOU Qingyuan
(PneumologyDepartment, 3201HospitalofZhonghangIndustry,Hanzhong723000,Shanxi,China)
[Abstract]Objective: To explore the relationship of HbA1c level with the incidence of adverse cardiovascular events(MACE) of CHD & DM patients after PCI therapy. Methods: Eighty-three cases of CHD & DM patients after PCI operation were selected and divided into group A (HbA1c<6.5%) and group B (HbA1c≥6.5%),with 38 cases in group A and 45 in group B. The preoperative CRP, ESR, TNF-α IL-6 in group A and group B were compared and MACE incidences were observed in 6 months and 24 months after PCI respectively. Results: The preoperative average CRP and TNF-α levels in group A were obviously higher than those in group B (t=5.944, 5.095, P<0.01), but the differences of ESR and IL-6 levels were not significant between groups A and B. The MACE incidence in 6 months after PCI therapy was not significantly different between groups A and B (P>0.05); But in 24 months after PCI therapy, the proportion of myocardial infarction and vascular restenosis in the patients in group A was significantly lower than that in group B (χ2=5.385, 6.629; P=0.020, 0.010). Conclusion: After PCI therapy, the prognosis of CHD & DM patients with lower HbA1c level is better than that of patients with higher HbA1c level.
[Key words]coronary heart disease; diabetes mellitus; cardiovascular diseases; HbA1c; percutaneous coronary intervention
[中图分类号]R459.9;R541.4;R587.1
[文献标识码]A
[文章编号]1000-2707(2015)01-0104-03
