胫骨近端闭合性粉碎性骨折环形外固定架治疗的疗效分析
2014-07-18张里程赵燕鹏唐佩福
张 巍,张里程,郝 明,赵燕鹏,唐佩福
胫骨近端闭合性粉碎性骨折环形外固定架治疗的疗效分析
张 巍,张里程,郝 明,赵燕鹏,唐佩福
目的探讨环形外固定架治疗胫骨近端闭合性粉碎性骨折的临床效果。方法选择2010-05至2012-05解放军总医院收治的胫骨近端闭合性粉碎性骨折25例,均属于闭合性骨折Tscherne分型中CⅡ型。OTA/AO骨折分型:A3型10例,C2型9例,C3型6例。均采用闭合复位或者有限切开复位骨折块后,应用Orthofix hybrid 外固定架治疗。结果术后均获得随访,随访时间12~16个月,平均(13.4±3.5)个月。所有患者均获得愈合,时间为4~11个月,平均6个月。术后针道反应4例,经局部换药,口服抗生素后治愈。2例骨折延迟愈合,给予局部自体骨植骨术后愈合。末次随访时影像学RRS评分优良率80%,HSS 膝关节临床功能评分优良率84%。结论利用环形外固定架治疗胫骨近端闭合性粉碎性骨折临床疗效满意。
胫骨近端;骨折,粉碎性;外固定架
胫骨近端骨折多由高能量暴力创伤引起,一般伴有严重软组织或骨组织缺损,使得其治疗极具挑战性[1]。胫骨近端骨折治疗的目标主要是重建正常的力线、稳定的关节及可活动的膝关节。常用治疗方法包括切开复位内固定、切开或手法复位外固定。切开复位内固定的优势在于可以直视下对骨折进行解剖复位[2],缺点是牺牲软组织的完整性,可能引起骨折不愈合、骨折延迟愈合等并发症。采用闭合复位或有限切开复位外固定架固定,远离不易愈合骨折部位的软组织窗进行操作,对于减少并发症促进骨折愈合更加具有优势[3,4]。笔者对2010-05至2012-05我科连续收治,并采用环形外固定架治疗的25例胫骨近端闭合性粉碎性骨折患者随访,评价其临床和影像学效果,以期为今后的临床工作提供参考。
1 对象与方法
1.1 对象 25例中,男21例,女4例;年龄34~55岁,平均(44.4±8.9)岁。车祸伤15例,爆炸伤4例,重物砸伤6例。受伤至手术时间为4~30 h,平均(14.3±6.8) h。根据闭合性骨折Tscherne分型:所有25例胫骨近端骨折均为CⅡ型。根据OTA/AO骨折分型:A3型10例,C2型9例,C3型6例。
1.2 手术方法 所有伤者入院时软组织条件较差,短期内无法行切开复位钢板内固定,因此急诊采用Orthofix hybrid 外固定架系统。手术在全麻或者硬膜外麻醉下进行。患者采取仰卧位,屈膝30°。术中不使用止血带。骨折复位在 C形臂X线机下进行。采用牵引等闭合复位方法,恢复下肢力线。对于涉及到关节面的骨折,首先通过胫骨近端前内侧骨皮质小切口,使用弯钝3 mm克氏针或者植骨棒在C形臂X线机监视下,从皮质小窗来顶起关节面骨折块,巾钳左右侧钳夹,前后纵向用克氏针临时稳定,然后用空心螺钉固定。闭合复位或者有限切开复位骨折块后,应用Orthofix hybrid 外固定架,并且将外固定架与螺钉连接固定。C形臂X线机透视下确认复位满意后,完全锁定外固定架各个关节。
对严重粉碎性骨折,术后应采取后托固定保护,常规钉道护理。术后24 h开始膝关节被动活动,48 h鼓励患者进行膝关节控制运动。术后8~12周根据影像学检查结果确定是否进行渐进性负重锻炼。
1.3 疗效评定 统计骨折愈合时间,记录不良反应发生情况,并在末次随访时进行HSS 膝关节临床功能评分( the hospital for special surgery knee-rating score)[5]和影像学RRS评分(Rasmussen’s radiological score)[6]。
2 结 果
术后均获得随访,随访时间12~16个月,平均(13.4±3.5)个月。骨折愈合时间4~11个月,平均(6.0±2.3)个月,典型病例见图1。术后4例有钉道反应,属于 Paley分级的1级即软组织炎性反应,经局部换药、口服抗生素静后治愈。2例骨折出现延迟愈合,给予局部自体骨植骨后3个月骨折获得愈合。
末次随访时所有骨折均愈合良好,力线恢复正常,无疼痛,步态无明显跛行。HSS 膝关节临床功能评分,优16例(64%),良5例(20%),可3例(12%),差1例(4%),优良率84%。影像学RRS评分结果为,优14例(56%), 良6例(24%), 可4例(16%), 差1例(4%),优良率80%。见表1。

图1 环形外固定架固定胫骨近端闭合性粉碎性骨折治疗前后X线片(女性,30岁,车祸伤,AO分型C3型骨折)
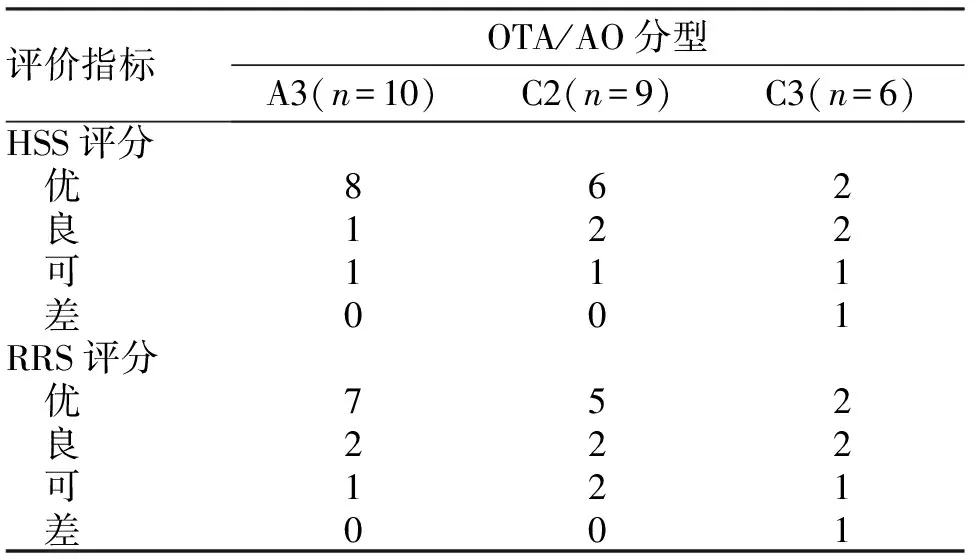
表1 骨折OTA/AO分型及末次随访HSS 膝关节临床功能评分与RRS评分结果
3 讨 论
由高能量损伤导致的胫骨近端骨折,往往伴有严重的局部软组织损伤,因此避免骨折周围软组织损伤进一步加重对于其治疗效果具有重要意义[7]。传统的切开复位会加剧局部血运的破坏,增加骨延迟愈合和感染风险。从这个角度来说,间接复位技术和通过远离骨折部位的软组织窗对断端进行操作无疑更具有优势[8]。笔者在C形臂X线机透视下采用手法复位,用环形外固定架外固定治疗胫骨近端的粉碎性骨折疗效满意。
在治疗时,通过闭合操作、小切口切开等方法可以在恢复关节面平整的同时,最大程度减少对局部软组织损伤,从而显著降低术后感染率。在一项回顾性研究中,Egol等[9]按照分期治疗方案,对胫骨近端骨折进行了切开复位内固定治疗,术后深部感染率仍达到了5%;而Catagni等[4]应用Ilizarov外固定架治疗59例胫骨近端骨折患者,术后无一例发生深部感染。本研究同样没有发现深部感染的患者,这与Catagni等的研究结果一致,发生钉道反应4例均通过应用抗生素和钉道护理得到有效控制。
对于胫骨近端粉碎严重的不稳定骨折患者,环形外固定架联合有限切开空心钉固定,可为骨折端提供足够的固定强度。在Ramos等[8]的一项前瞻性研究中,30例通过Ilizarov环形外固定架治疗的胫骨近端骨折患者均进行了早期负重康复训练,均未发现骨质丢失现象。本研究中除骨折粉碎严重C3型骨折外,其余患者均进行早期功能锻炼,随访期间没有出现外架松动及固定针断裂问题,末次随访HSS评分和RRS评分优良率均达80%,表明环形外固定架具有良好的稳定性,与Babis等[10]报道结果相似。
Parekh等[11]应用两阶段方法(初期应用外固定,软组织恢复后更换内固定)治疗高能量胫骨近端骨折也是一种有效的手段,患者可以获得良好的功能和骨折愈合。但是二次手术的痛苦、医疗费用的增加,限制了这种治疗方法的广泛应用。本研究将外固定架作为终极治疗手段,既避免了二次手术,又节省了医疗费用。然而,不足之处在于患者带架时间较长,日常生活不便,活动受到一定限制,且钉道需要长期护理等。
利用环形外固定架固定胫骨近端闭合性粉碎性骨折,可最大限度保护软组织及骨折周围血供,最大程度减少切开复位内固定引起的并发症,为骨折愈合创造最佳愈合基础,是一种可以选择的治疗方法。
[1] Schneidmueller D, Gercek E, Lehnert M,etal. Proximal tibial fractures [J]. Unfallchirurg, 2011, 114(5): 396-402.
[2] Feng W, Fu L, Liu J,etal. Biomechanical evaluation of various fixation methods for proximal extra-articular tibial fractures [J]. J Surg Res, 2012, 178(2): 722-727.
[3] Thaller P H, Fürmetz J, Wolf F,etal. Limb lengthening with fully implantable magnetically actuated mechanical nails (PHENIX((R)))-preliminary results[J]. Injury, 2014,45(Suppl 1):S60-65.
[4] Catagni M, Ottaviani G, Maggioni M. Treatment strategies for complex fractures of the tibial plateau with external circular fixation and limited internal fixation[J]. J Trauma, 2007,63(5):1043-1053.
[5] Liu F, Tao R, Cao Y,etal. The role of LISS (less invasive stabilisation system) in the treatment of peri-knee fractures [J]. Injury, 2009, 40(11):1187-1194.
[6] Malakasi A, Lallos S N, Chronopoulos E,etal. Comparative study of internal and hybrid external fixation in tibial condylar fractures[J]. Eur J Orthop Surg Traumatol, 2013,23(1):97-103.
[7] Stannard J P, Finkemeier C G, Lee J,etal. Utilization of the less invasive stabilization system internal fixator for open fractures of the proximal tibia: a multi-center evaluation[J]. Indian J Orthop, 2008,42(4):426-430.
[8] Ramos T, Ekholm C, Eriksson B I,etal. The Ilizarov external fixator - a useful alternative for the treatment of proximal tibial fractures: a prospective observational study of 30 consecutive patients [J]. BMC Musculoskelet Disord, 2013,14(1):11-16.
[9] Egol K A, Tejwani N C, Capla E L,etal. Staged management of high-energy proximal tibia fractures (OTA types 41): the results of a prospective, standardized protocol [J]. J Orthop Trauma, 2005,19(7):448-455.
[10] Babis G C, Evangelopoulos D S, Kontovazenitis P,etal. High energy tibial plateau fractures treated with hybrid external fixation [J]. J Orthop Surg Res, 2011,6:35-45.
[11] Parekh A A, Smith W R, Silva S,etal. Treatment of distal femur and proximal tibia fractures with external fixation followed by planned conversion to internal fixation [J].J Trauma, 2008,64(3):736-739.
(2014-01-15收稿 2014-03-18修回)
(责任编辑 武建虎)
Applicationofcircularexternalfixatortotreatmentofclosedcomminutedproximaltibialfracture
ZHANG Wei, ZHANG Licheng, HAO Ming, ZHAO Yanpeng, and TANG Peifu. Department of Orthopaedics, General Hospital of PLA, Beijing 100853,China
ObjectiveTo study the clinical efficacy of circular external fixator in treatment of the closed and comminuted proximal tibia fracture.MethodsTwenty-five patients with closed and comminuted proximal tibia fracture, including 21 males and 4 females, who were admitted to this department from May 2010 to the corresponding time in 2012 were included in this retrospective analysis. The fracture of all these patients with a mean age at 44 years belonged to CⅡtype according to Tscherne classification while ten of them were classified into A3 type, nine into C2, six into C3 under OTA/AO fracture classification. All the patients were treated with Orthofix hybrid external fixator after closed reduction or limited open reduction.ResultsAll the patients were followed up and the follow-up time was between 12 and 16 months, with an average of(13.4±3.5)months. Patients included in this research all gained bone union, however the time for full healing varied, ranging from 4 to 11 months, with a mean of six months. Four of the cases experienced needle reaction postoperatively, and were all healed by using antibiotics combined with local dressings therapy. Delayed union occurred in 2 cases and healed by bone autograft. The radiographical RRS assessment was performed during the final follow-up, which showed a 80% of the excellent rate. In addition, The excellent rate of HSS score was 84%.ConclusionsCircular external fixator contributes to a satisfying outcome in treatment of the closed and comminuted proximal tibia fracture.
proximal tibial; fracture, comminuted; circular external fixation
解放军总医院科技创新苗圃基金课题(13KMM11)
张 巍,博士,主治医师, E-mail: bszw@hotmail.com
100853北京,解放军总医院骨科
唐佩福, E-mail: pftang301@163.com
R683.42
