椎间孔入路经皮内镜技术摘除脱出髓核 36 例报告
2014-02-14董健文戎利民刘斌王其友冯丰陈瑞强谢沛根张良明
董健文 戎利民 刘斌 王其友 冯丰 陈瑞强 谢沛根 张良明
. 脊柱微创外科 Minimally invasive spine surgery .
椎间孔入路经皮内镜技术摘除脱出髓核 36 例报告
董健文 戎利民 刘斌 王其友 冯丰 陈瑞强 谢沛根 张良明
目的分析椎间孔入路经皮内镜技术治疗脱出型腰椎间盘突出症的困难性及其处理对策。方法2011 年 2 月至 2014 年 2 月,采用椎间孔入路经皮内镜技术治疗 36 例脱出型腰椎间盘突出症,男 21 例,女 15 例,平均年龄 41 岁。突出节段 L3~42 例、L4~523 例、L5~S111 例。基于 Lee 分类法,将36 例脱出分类为重度头端脱出 5 例、轻度头端脱出 7 例、轻度尾端脱出 15 例、重度尾端脱出 9 例。首先采用“Between”技术摘除椎间隙平面脱出物并行硬膜外松解获得操作空间,然后将鞘管移向脱出方向采用“椎管内”技术镜下摘除剩余脱出物。结果平均手术时间为 108 min。术后短期大腿前方麻木 4 例、短期髂腰肌肌力下降 1 例、硬脊膜损伤合并多根神经根损伤 1 例、出口神经根损伤 1 例且脱出髓核摘除不彻底,其余 35 例脱出髓核摘除彻底。平均随访时间 16 ( 3~38 ) 个月,术后第 1 天腰痛 VAS )、腿痛 VAS评分 ( visual analogue scale ) 较术前改善 ( P<0.01 ),术后 3 个月 VAS、JOA 腰痛评分 ( japanese orthopaedic association scores )、Oswestry 功能障碍指数 ( oswestry disability index,ODI ) 指数较术前改善 ( P<0.01 ),MacNab疗效优 25 例、良 7 例、可 3 例、差 1 例。随访期内无复发与再手术。结论椎间孔入路经皮内镜结合应用“Between”技术与“椎管内”技术治疗绝大部分脱出型腰椎间盘突出症可获得良好的疗效,椎间孔扩大成形、初始通道建立与鞘管椎管内移动、镜下脱出髓核的准确判断是其技术关键,但对重度脱出仍然是一项挑战,其手术失败率、并发症发生率较高。
腰椎;椎间盘移位;椎间盘切除术,经皮;内窥镜检查
椎间孔入路经皮内镜技术近年来在国内发展迅速,尤其是 TESSYS ( transforaminal endoscopic spine system ) 技术几乎可应用于治疗所有类型的腰椎间盘突出症[1-7],包括脱出型[8-12]。然而,由于镜下手术视野的局限性,即使是采用完全 TESSYS 即椎管内技术,对于脱出髓核尤其是严重脱出者也不能确保在可视情况下能将其完全取出,易造成脱出髓核残留而导致手术失败[8,13]。本研究旨在分析椎间孔入路经皮内镜技术运用于脱出型腰椎间盘突出症的疗效和针对各种技术困难的相应对策。
资料与方法
一、一般资料
2011 年 2 月至 2014 年 2 月,采用椎间孔入路经皮内镜技术治疗 36 例脱出型腰椎间盘突出症,男 21 例,女 15 例,平均年龄 41 ( 17~76 ) 岁。突出节段 L3~42 例、L4~523 例、L5~S111 例。在 Lee分类法基础上[8],将脱出超过上位椎弓根下缘以下3 mm 平面定义为重度头端脱出、脱出位于上位椎体下终板与上位椎弓根下缘以下 3 mm 之间为轻度头端脱出、脱出位于下位椎体上终板与下位椎弓根中部之间为轻度尾端脱出、超过下位椎弓根中部为重度尾端脱出 ( 图 1 ), 按照此分类方法,矢状面脱出包括重度头端脱出 5 例、轻度头端脱出 7 例、轻度尾端脱出 15 例、重度尾端脱出 9 例。重度脱出中 1 例头端脱出超出上位椎弓根上缘、2 例尾端脱出超出下位椎弓根下缘 ( 表 1 )、4 例游离;水平面脱出包括中央、旁中央、椎间孔内、椎间孔外脱出,依次为 4 例、27 例、4 例、1 例。合并侧隐窝与 ( 或 ) 椎间孔狭窄 8 例、突出钙化 5 例。
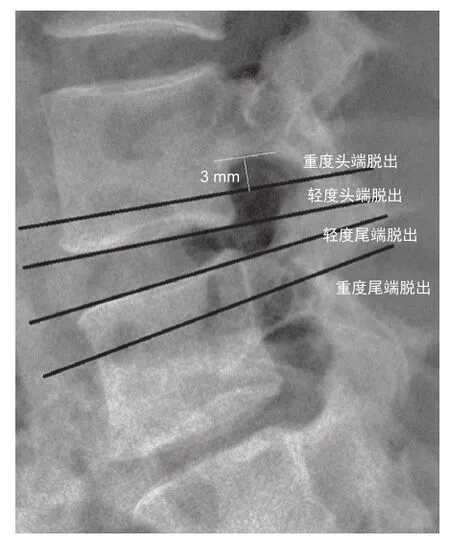
图 1 矢状面脱出分类示意图Fig.1 Classifcation of disc migration on the sagittal plane
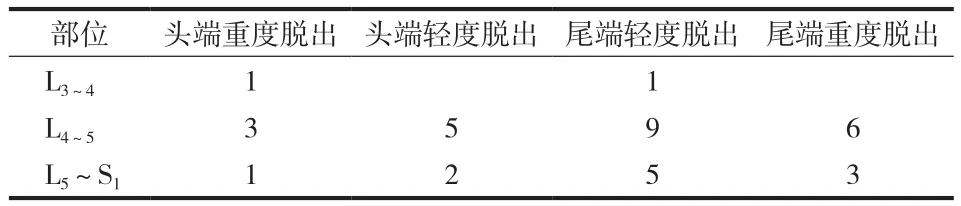
表1 各种类型脱出分布情况Tab.1 Distribution of different types of disc migration
纳入标准:单侧下肢放射性疼痛麻木 ( 伴 / 不伴腰痛 )、相应神经根支配区感觉与肌力减退或缺失、直腿抬高试验阳性,CT、MRI、椎管照影、CTM 征象与临床相符、保守治疗效差或反复发作,其中术前背伸与 ( 或 ) 踝背伸瘫痪 3 例。排除标准:多节段突出、合并马尾综合征、腰椎不稳、病变节段既往手术史。
手术由同一组脊柱外科医师完成,采用设备为 SPINENDOS 脊柱内镜系统 ( SPINENDOS Gmbh,Germany ) 与 Ellman 等离子消融刀头系统 ( Ellman Innovation,New York,USA )。
二、手术方法
侧卧位,患侧在上,腰部垫枕。术前仅标记后正中线与患侧髂脊体表投影线,L4~5、L5~S1节段穿刺点分别位于后正中线旁开 12 cm、14 cm 髂脊上缘稍高处,L3~4穿刺点为其椎间隙水平线于后正中线旁开 10 cm 处。皮肤、筋膜层与关节突周围采用0.5% 利多卡因分层浸润麻醉,术中辅助静滴氟比洛芬酯 100 mg。根据髓核脱出部位、椎间孔形态大小确定穿刺靶点,对无需椎间孔扩大成形者穿刺靶点直接选择 AP 透视位于椎弓根内缘、侧位透视位于椎间盘后缘中点处,对需行椎间孔扩大成形者尤其是L5~S1节段穿刺靶点选择偏向背侧或上关节突尖部。G 型臂透视引导下将 18 号穿刺针针尖穿刺到达靶向部位,置入导丝后取出穿刺针,作 8 mm 皮肤切口,导丝引导下逐级扩张软组织,采用环锯清除椎间孔内韧带软组织,对须进行椎间孔扩大成形者去除部分上关节突前外侧骨质,在软组织扩张与椎间孔扩大成形过程中均可对穿刺靶点不满意者进行微调,置入工作鞘管,根据脱出方向,侧位透视显示鞘管斜面可稍高于或低于椎间盘后缘中点、且斜面各 50% 横跨于椎间隙与椎管 ( 即 Between 技术 )[14],椎间盘髓核蓝染造影可在穿刺过程中或鞘管置入后进行。
镜下操作首先摘除脱出髓核基底部,显露确认镜下解剖关系,进一步清除椎间隙后部松动或游离髓核碎片,确认硬膜囊搏动以及其与纤维环后缘之间隙,如为旁中央型与中央型脱出,须显露后纵韧带并探查其深、浅面。采用等离子射频消融、止血与纤维环成形,同时松解纤维环与硬膜囊之间隙,以利于根据脱出方向将工作鞘管向头端或尾端于椎管内倾斜,此时部分鞘管斜面位于椎体后方。如为轻度脱出,则可直视下将脱出物完全取出,如为重度脱出尤其是远端超出椎弓根范围,则先采用等离子刀头松解脱出物周围,尽可能将其大块完整取出,如脱出物碎裂无法整块取出,则需反复用等离子刀头探查椎弓根内侧区域,如患者疼痛麻木主述症状消失、镜下硬膜囊神经根搏动恢复良好、取出脱出物量与术前影像学相符,则可结束手术( 图 2,3 )。
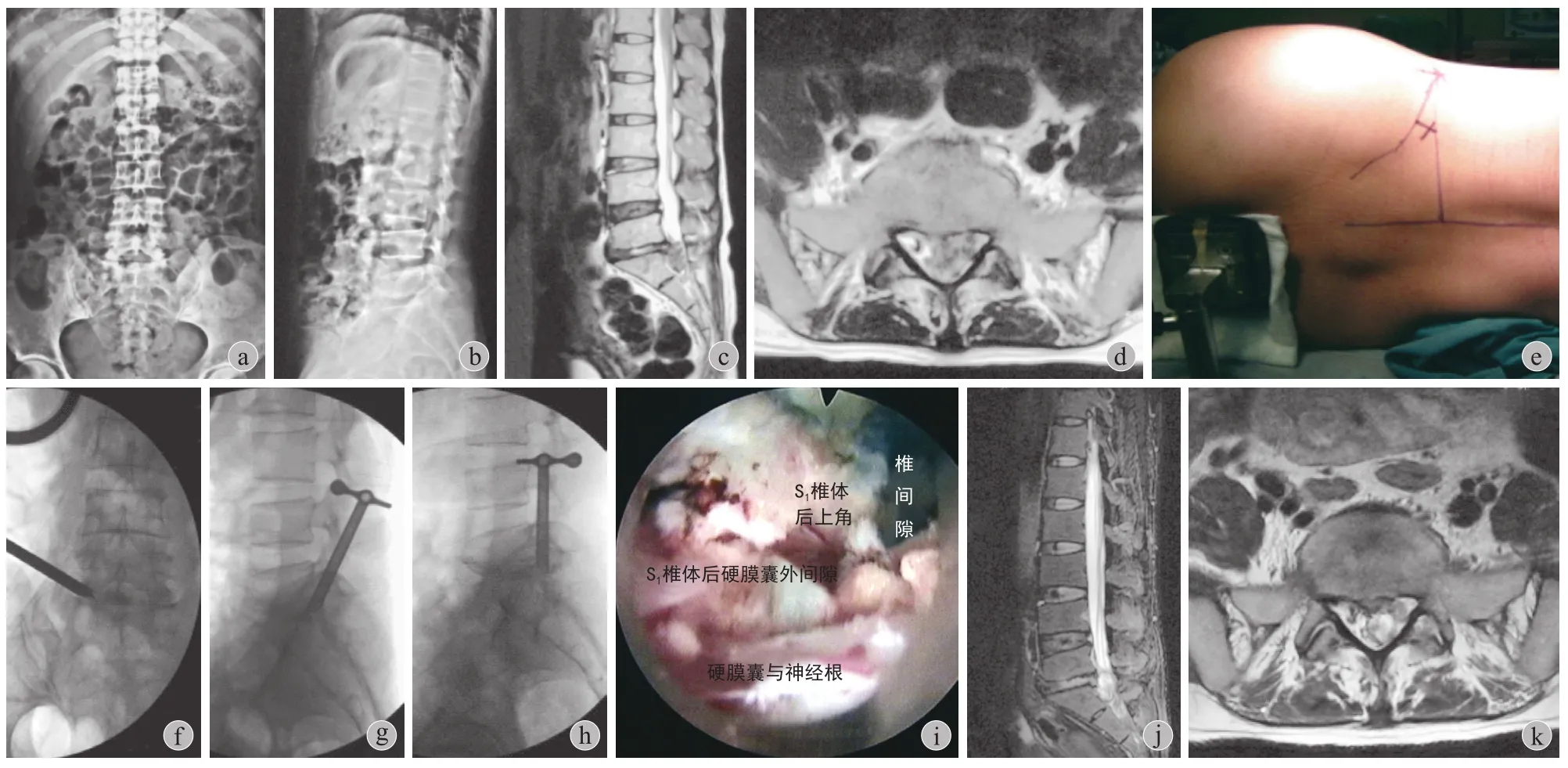
图 2 a:术前前后位;b:术前侧位;c:术前 MRI 示 L5~ S1椎间盘重度尾端脱出;d:术前 MRI 轴位示 L5~ S1椎间盘巨大旁中央脱出;e:手术侧卧位与穿刺点体表标记;f:术中前后位透视示工作通道鞘管位于椎弓根内缘;g:术中侧位透视示工作通道鞘管斜面位于椎间盘后缘中点、各 50% 横跨于椎间隙与椎管;h:鞘管椎管内移向尾端,显示完全椎管内技术;i:鞘管到达 S1椎体后硬膜外间隙,将脱出物摘除,硬膜囊搏动良好;j ~ k:术后 MRI 示脱出物摘除彻底Fig.2 a: The preoperative anteroposterior ( AP ) X-ray image; b: The preoperative lateral X-ray image; c: The preoperative MRI sagittal image showed L5-S1high-grade downward migration; d: The preoperative MRI axial image showed L5-S1huge paracentral extrusion; e: The superfcial marker of the puncture point in the lateral position; f: The AP fuoroscopic view showed the position of the beveled cannula at the medial pedicular line; g: The lateral fuoroscopic view showed the beveled cannula was “half-and-half” positioned across the disc space to the epidural space; h: The beveled cannula was advanced along the direction of migration in the epidural space which was called complete “intracanal” endoscopic technique; i: The remanent fragments migrated downward were completely removed and a good visualization of dura sac pulsation was achieved; j-k: The postoperative MRI images showed the L5-S1down-migrated disc was removed completely
三、术后处理
术后次日戴腰围下床行走,术后即刻复查三维CT 或 MRI 了解脱出髓核摘除与椎间孔扩大成形情况,术后 1~2 天出院,戴腰围 6 周。术后 1 个月、3 个月、半年、1 年、2 年定期复查,采用 MacNab疗效评定、视觉模拟评分 ( visual analogue scale,VAS )、JOA 腰痛评分与 Oswestry 功能障碍指数( oswestry disability index,ODI ) 评价疗效。
四、统计学分析
对所有数据采用 SPSS 21.0 软件 ( SPSS Inc,Chicago,IL,USA ) 进行统计学分析处理,采用非参数检验方法对 JOA 评分、ODI 指数、VAS 评分等不符合正态分布的数据进行分析,P<0.05 为差异显著性标准。
结 果
平均手术时间为 108 min。4 例术后短期大腿前方麻木,1 例重度头端脱出为 L4~5椎间盘向上脱出至 L3~4椎间隙平面,术前踝背伸与趾背伸肌力0 级,术中 L4神经根损伤,术中造影显示仍存在压迫改开放手术,发现上位椎弓根下缘以上脱出部分残留,术后神经功能无恢复 ( 图 4 ),其余35 例术后复查 MRI 或 CT 均显示脱出髓核摘除彻底。1 例 L4~5重度尾端脱出术中损伤硬脊膜,术后出现多根神经根损伤表现,对症治疗后部分恢复;1 例 L3~4头端重度脱出术后短期髂腰肌肌力下降,对症治疗后恢复。平均随访 16 ( 3~38 ) 个月,术后第 1 天腰痛 VAS、腿痛 VAS 评分分别为 1.95±0.53、1.01±0.56,均较术前改善 ( P<0.01 ),术后 3 个月腰痛 VAS、腿痛 VAS、JOA、ODI 依次为 0.58±0.42、0.51±0.38、27.44±1.36、11.78±2.65,均较术前改善 ( P<0.01 ) ( 表 2 )。改良 MacNab 疗效为优 25 例、良 7 例、可 3 例、差1 例,优良率 88.89%,各种脱出类型疗效优良率依次为轻度脱出 100%、重度头端脱出 80%、重度尾端脱出 66% ( 表 3 )。随访期内无复发与再手术。
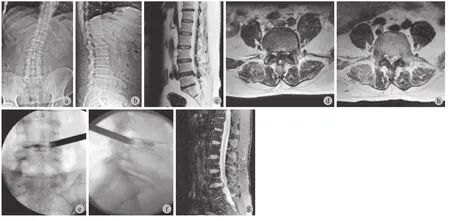
图 3 a:术前前后位;b:术前侧位;c:术前 MRI 示L4~5椎间盘轻度尾端脱出;d:术前 MRI 轴位示 L4~5椎间盘旁中央脱出;e ~ f:术中 AP、侧位透视示初始工作鞘管位置良好;g ~ h:术后 MRI 示脱出物摘除彻底Fig.3 a: The preoperative AP X-ray image; b: The preoperative lateral X-ray image; c: The preoperative MRI sagittal image showed L4-5low-grade downward migration; d: The preoperative MRI axial image showed L4-5paracentral extrusion; e-f: The AP and lateral fluoroscopic images showed satisfactory initial position of the beveled cannula; g-h: The postoperative MRI images showed the L4-5down-migrated disc was removed suffciently
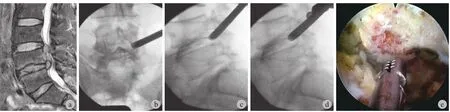
图 4 a:术前 MRI 示 L4~5椎间盘重度头端脱出;b ~ c:术中前后位、侧位位透视示初始工作鞘管位置良好;d:鞘管椎管内移向头端;e:镜下显示 L4椎体后空间脱出物已摘除,4 点钟为 L4神经根损伤,改开放手术证实 L4椎弓根下缘以上脱出物残留Fig.4 a: The preoperative MRI sagittal image showed L4-5high-grade upward migration; b-c: The AP and lateral fuoroscopic images showed satisfactory initial position of the beveled cannula; d: The beveled cannula was advanced towards the head in the epidural space; e: The endoscopic image showed the L4-5upward migrated disc behind the posterior wall of L4vertebrae was removed and L4nerve root was incompletely injured at 4 o’clock. Residual migrated fragments beyond the inferior margin of L4pedicle were found during the subsequent open surgery
讨 论
根据北美脊柱协会、美国脊柱放射学协会、美国神经放射学协会联合推荐腰椎间盘突出症命名与分类方法,如椎间盘突出物离开其突出部位,不论是否与其基底部连续,均视为脱出型,其中无连续性者特别命名为游离型[15]。矢状面上椎管内脱出椎间盘组织可向头端或尾端脱出,而在水平面上可向中央、旁中央、椎间孔内、椎间孔外脱出,临床大多数为向尾端旁中央脱出[15-16],本组病例脱出类型分布与既往文献报道一致。椎间孔入路经皮内镜TESSYS 技术采用不同直径的环锯逐级去除上关节突前外侧部分骨质以行椎间孔扩大成形,故工作鞘管可置入椎管内直接摘除突出髓核与直接神经根松解减压,已被运用于治疗包括脱出型在内的各种类型腰椎间盘突出症。水平面上不论是中央型还是椎间孔外型脱出,通过调整工作鞘管进入的深度均可直视脱出物,故对于椎间孔入路而言将其摘除并不困难。然而,对于矢状面上的脱出,由于镜下视野的局限性,当脱出超出上位椎弓根下缘与下位椎弓根上缘时,脱出物远端并不可见,即使脱出物与其基底部相连,也难以确保通过夹住其基底部而将其完整取出以避免残留,如脱出物已游离甚至碎裂,即使被蓝染也难以被确认与整块或分块取出。尽管TESSYS 技术可将工作鞘管在椎管内移动以尽可能接近脱出物远端,但这种可调整性与椎间孔大小及其扩大成形效果有关,对于 L5~S1节段髂脊较高位者尤其困难,由于存在这些技术局限性,因而对于通过椎间孔入路经皮内镜摘除脱出尤其是重度脱出物而言无疑是一种挑战。
表2 术前-、术后第 1 天、术后 3 个月 VAS、JOA 评分、ODI 指数比较 (±s )Tab.2 Comparison of VAS, JOA and ODI- scores preope-ratively and at 1 day and 3 months after the operation (±s )
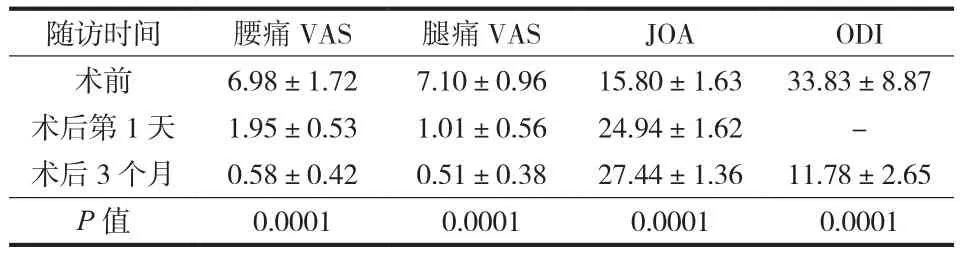
表2 术前-、术后第 1 天、术后 3 个月 VAS、JOA 评分、ODI 指数比较 (±s )Tab.2 Comparison of VAS, JOA and ODI- scores preope-ratively and at 1 day and 3 months after the operation (±s )
注:P 值为术后 3 个月与术前比较Notice: P referred to the comparison between the preoperative scores and that at 3 months after the operation
随访时间 腰痛 VAS 腿痛 VAS JOA ODI术前 6.98±1.72 7.10±0.96 15.80±1.63 33.83±8.87术后第 1 天 1.95±0.53 1.01±0.56 24.94±1.62 -术后 3 个月 0.58±0.42 0.51±0.38 27.44±1.36 11.78±2.65 P 值 0.0001 0.0001 0.0001 0.0001
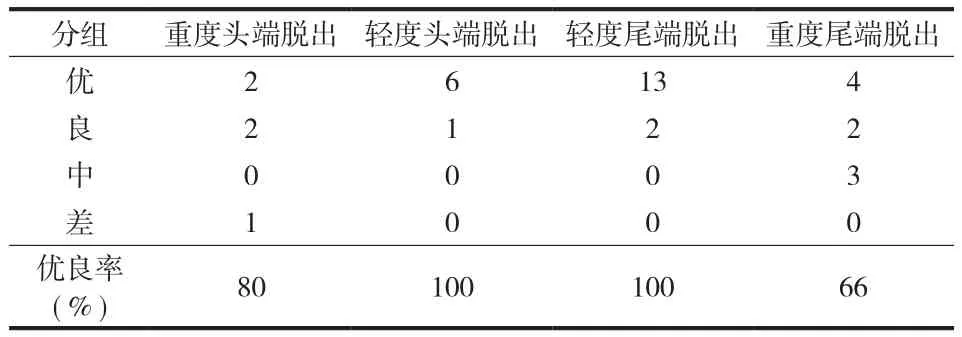
表3 术后 3 个月改良 MacNab 疗效评价Tab.3 Modifed MacNab evaluation at 3 months after the operation
与处理非脱出椎间盘不同的是,对于脱出型包括游离型,椎间孔扩大成形与脱出物周围松解在技术要求上显得格外重要。即使是椎间孔狭窄不明显者,适当的扩大成形也有利于鞘管的置入及其位置微调,而 L5~S1椎间孔常存在不同程度的狭小,且鞘管置入角度相对较大,受髂脊影响,鞘管往往难以向头端倾斜调整,因此,良好的椎间孔扩大成形是保证其手术成功的前提条件。不论是轻度还是重度脱出,工作鞘管在矢状面的初始位置建议仍然选择在椎间盘后缘中点附近,其斜面各 50% 横跨于椎间隙与椎管,即“Between”技术,其优点在于易于辨别解剖关系与处理椎间隙后部松动或游离髓核碎片、即脱出基底部,这有别于经典 TESSYS 技术,从某种意义上说其实是一种由盘内到盘外操作技术。如果将鞘管初始位置直接向脱出方向置于椎管内,在尚未辨明解剖关系的情况下就贸然摘除脱出物易造成神经组织损伤,也缺乏对脱出状况整体的认识而易遗漏。摘除基底部脱出物后可形成下一步操作的空间,也能初步判断硬膜囊搏动情况,对于中央型脱出需将鞘管深入,探查后纵韧带深、浅面。采用等离子射频消融刀头松解硬膜囊与脱出物、椎体后缘间隙,直至上位椎弓根下缘或下位椎弓根上缘可见,处理相应椎弓根上下缘与椎体上下终板后角与椎体后缘周围软组织以获得充足的椎管内空间,如椎间孔扩大成形不理想导致上关节突影响视野与操作,可在镜下采用骨凿与 Pounch 钳处理上关节突及其深面附着黄韧带,将鞘管沿脱出方向在椎管内移动,所有操作均在硬膜囊前方进行,至此可完全显露轻度脱出物,对于重度脱出也可大部分显露。
由此可见,对于轻度脱出,不论是头端还是尾端脱出,既往文献与本组病例研究结果均表明通过椎管内技术完全可将其完整摘除以获得良好的疗效,而对于重度脱出,尤其是超出镜下可视范围时,能否彻底摘除仍然是存在诸多不确定性。尽管通过脱出物周围充分松解以尽可能将其大块取出,镜下可见脱出物摘除完毕后再使用等离子刀头反复探查椎弓根区域,并结合患者主观症状消失、镜下硬膜囊神经根搏动、取出量与术前影像学相符等方面综合判断可提高彻底摘除成功率,但仍然存在残留可能。严格选择病例有助于减少手术失败率,正如 Lee 等[8]则对于脱出超出上位椎弓根下缘与游离超出下位椎弓根中部者不主张采用椎间孔入路,可见对于重度头端脱出尤其需更加慎重,临床上向头端脱出更多发生于高位间隙[16],由于神经走行解剖原因,在建立通道与镜下操作易造成出口根损伤,本组病例中 1 例 L3~4重度头端脱出术后短期髂腰肌肌力下降便与通道建立有关。对于病史较长、经过反复甚至过度按摩等保守治疗的重度脱出,极有可能游离,则更增加了手术难度,既不易整块取出,也由于粘连不易松解且易硬膜外出血而影响操作。
显然,椎间孔入路本身的局限性与目前普遍采用硬鞘管内镜系统是造成无法确保彻底摘除重度脱出椎间盘组织的根本原因,即使有学者采用极外侧入路、或是对于重度尾端脱出采用椎弓根上入路与去除部分下位椎弓根上缘骨质以增大视野,也无法从根本上克服这一缺陷[9,17]。Kim 等[18]对 5 例重度尾端脱出从对侧椎间孔入路置入鞘管并逐渐到达患侧脱出物处,这一大胆的技术尝试理论上可解决患侧椎弓根与上关节突对脱出物的遮挡,但几乎需要摘除大部分后方纤维环甚至后纵韧带以获得操作空间,且鞘管在硬膜囊前方表面横跨椎管内也大大增加了神经损伤的风险,同时对技术掌握要求极高。因此,对侧椎间孔入路目前尚不能为大多数术者所接纳,且是否有必要采用这样一种有可能创伤更大、风险更高的技术去处理重度脱出椎间盘值得商榷,而采用椎板间入路,不论是显微内镜 ( MED ) 还是全脊柱内镜 ( PELD ) 技术[19-20],会较椎间孔入路更易将脱出物彻底摘除。
本研究表明,椎间孔入路经皮内镜结合应用“Between”技术与“椎管内”技术,可成功摘除绝大部分的椎间盘脱出物并获得良好的疗效,椎间孔扩大成形、初始通道建立与鞘管椎管内移动、镜下脱出髓核的准确判断是其技术关键,但对于重度脱出尤其是 L5~S1节段手术操作困难且手术失败率、并发症发生率较高,需与患者良好的沟通,如术前或术中判断脱出物无法彻底摘除,需及时改用其它术式。
[1]Hoogland T, Schubert M, MikliIz B, et a1. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopagain: a prospective randomized study in 280 consecutive cases. Spine, 2006, 3l(24):E890-897.
[2]Jang JS, An SH, Lee SH. Transforaminal percutaneous endoscopic discectomy in the treatment of foraminal and extraforaminal lumbar disc herniations. J Spinal Disord Tech, 2006, 19(5):338-343.
[3]Ruetten S, Komp M, Merk H. Full endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective randomized, controlled study. Spine, 2008, 33(9):931-939.
[4]Hoogland T, Sehubert M, Miklitz B, et a1. Endoscopic transforaminal discectomy for recurrent lumbar disc herniation: a prospective, cohort evaluation of 262 consecutive cases. Spine, 2008, 33(9):973-978.
[5]周跃, 李长青, 王建, 等. 椎间孔镜YESS与TESSYS技术治疗腰椎间盘突出症. 中华骨科杂志, 2010, 30(3):225-231.
[6]Nellensteijn J, Ostelo R, Bartels R, et al. Transforaminal endoscopic surgery for symptomatic lumbar disc herniations: a systematic review of the literature. Eur Spine J, 2010, 19(2):181-204.
[7]Gibson JN, Cowie JG, Iprenburg M. Transforaminal endoscopic spinal surgery: the future ‘gold standard’ for discectomy? - A review. Surgeon, 2012, 10(5):290-296.
[8]Lee S, Kim SK, Lee SH, et al. Percutaneous endoscopic lumbar discectomy for migrated disc herniation: classifcation of disc migration and surgical approaches. Eur Spine J, 2007, 16(3):431-437.
[9]Kim HS, Ju CI, Kim SW, et al. Endoscopic transforaminal suprapedicular approach in high grade inferior migrated lumbar disc herniation. J Korean Neurosurg Soc, 2009, 45(2):67-73.
[10]Choi G, Lee SH, Lokhande P, et al. Percutaneous endoscopic approach for highly migrated intracanal disc herniations by foraminoplastic technique using rigid working channel endoscope. Spine, 2008, 33(15):E508-515.
[11]Jasper GP, Francisco GM, Telfeian AE. Endoscopic transforaminal discectomy for an extruded lumbar disc herniation. Pain Physician, 2013, 16(1):E31-35.
[12]隰建成, 马远征, 崔旭, 等. 椎间孔镜治疗脱出型腰椎间盘突出症疗效分析. 中国疼痛医学杂志, 2013, 19(1):35-38.
[13]Lee SH, Kang BU, Ahn Y, et al. Operative failure of percutaneous endoscopic lumbar discectomy: a radiologic analysis of 55 Cases. Spine, 2006, 31(10):E285-E290.
[14]Liu KX, Massoud B. Transforaminal endoscopic lumbar procedure for disc herniations: a “between” technique. Surg Technol Int, 2010, 19:203-210.
[15]Fardon DF, Milette PC. Nomenclature and classification of lumbar disc pathology. Recommendations of the combined task forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine, 2001, 26(5):E93-113.
[16]Daghighi MH, Pouriesa M, Maleki M, et al. Migration patterns of herniated disc fragments: a study on 1,020 patients with extruded lumbar disc herniation. Spine J, 2013, Pii: s1529-9430(13)01985-2.
[17]Ruetten S, Komp M, Godolias G. An extreme lateral access for the surgery of lumbar disc herniations inside the spinal canal using the full-endoscopic uniportal transforaminal approachtechnique and prospective results of 463 patients. Spine, 2005, 30(22):2570-2578.
[18]Kim JS, Choi G, Lee SH. Percutaneous endoscopic lumbar discectomy via contralateral approach: a technical case report. Spine, 2011, 36(17):E1173-1178.
[19]Ikuta K, Tono O, Senba H, et al. Translaminar microendoscopic herniotomy for cranially migrated lumbar disc herniations encroaching on the exiting nerve root in the preforaminal and foraminal zones. Asian Spine J, 2013, 7(3):190-195.
[20]Kim CH, Chung CK, Woo JW. Surgical outcome of percutaneous endoscopic interlaminar lumbar discectomy for highly migrated disc herniation. J Spinal Disord Tech, 2012, [Epub ahead of print].
( 本文编辑:马超 )
Percutaneous transforaminal endoscopic surgery for migrated lumbar disc: 36 cases
DONG Jian-wen, RONG Li-min, LIU Bin, WANG Qi-you, FENG Feng, CHEN Rui-qiang, XIE Pei-gen, ZHANG Liang-ming. Department of Spinal Surgery, the third affliated Hospital of Sun Yat-sen University, Guangzhou, Guangdong, 510630, PRC
ObjectiveTo analyze the pitfalls and technical notes of percutaneous transforaminal endoscopic surgery for migrated lumbar disc herniation.MethodsThirty-six consecutive patients with different types of migrated lumbar disc herniation received percutaneous transforaminal endoscopic discectomy from February 2011 to February 2014. There were 21 males and 15 females, with an average age of 41 years old. There were 2 cases of migrated L3-4disc, 23 cases of migrated L4-5disc and 11 cases of migrated L5-S1disc. Based on Lee’s classifcation of migrated disc, there were high-grade upward migration in 5 cases, low-grade upward migration in 7 cases, low-grade downward migration in 15 cases and high-grade downward migration in 9 cases. The disc fragments at the intervertebral level were removed frst by “between” technique, and then the epidural space was released to create manipulation space. Finally, the beveled cannula was manually advanced along the migration direction to perform endoscopic discectomy for the remanent migrated disc, which was called “intracanal” technique.ResultsThe mean operation time was 108 minutes. The postoperative complications included transient numbness in the anterior thigh in 4 cases, transient iliopsoas weakness in 1 case, multiple nerve root injuries caused by dura tears in 1 case and exit nerve root injuries as well as incomplete endoscopic discectomy in 1 case. Complete removal of migrated disc was confrmed in the other 35 cases. All the patients were followed up for a mean duration of 16 months ( range: 3-38 months ). The Visual Analogue Scale ( VAS ) scores of low back pain and leg pain at 1 day after the surgery were signifcantly improved when compared with that preoperatively ( P<0.01 ). The low back pain VAS score, leg pain VAS score, Japanese Orthopedic Association ( JOA ) score and Chinese Oswestry Disability Index ( ODI ) score at 3 months after the surgery were signifcantly improved when compared with that preoperatively ( P<0.01 ). According to the Macnab criteria, the clinical results were excellent in 25 cases, good in 7 cases, fair in 3 cases and bad in 1 case respectively. There was no recurrence or revision during the follow-up.ConclusionsGood clinical results can be achieved by percutaneous transforaminal endoscopic surgery combined with “between” technique and “intracanal” technique inmost patients with migrated lumbar disc herniation. The technical notes include proper foraminotomy, satisfactory initial position of beveled cannula, manipulation of beveled cannula along the direction of migration in the epidural space and accurate discrimination of migrated disc materials. It’s still a challenge to treat high-grade migration via the transforaminal approach, due to a higher failure rate and a higher incidence of complications.
Lumbar vertebrae; Intervertebral disc displacement; Diskectomy, percutaneous; Endoscopy
10.3969/j.issn.2095-252X.2014.08.009
Th776.1, R681.5
510630 广州,中山大学附属第三医院脊柱外科
2014-06-01 )
