退行性半月板撕裂患者理疗与关节镜下手术疗效的前瞻性比较研究
2014-02-13付东单连成蔡郑东李国东
付东 单连成 蔡郑东 李国东
. 膝关节外科 Knee surgery .
退行性半月板撕裂患者理疗与关节镜下手术疗效的前瞻性比较研究
付东 单连成 蔡郑东 李国东
目的评估针对退行性半月板撕裂,联合关节镜手术与理疗疗效是否优于单纯理疗。方法40 例年龄>50岁,经磁共振 (MRI ) 确诊为半月板撕裂患者根据数字随机法分为两个治疗组。一组接受关节镜手术治疗 (关节镜手术+理疗组 ) 20 例,术后实施物理治疗;另一组接受单纯物理治疗方案 (物理治疗组 ) 20 例。治疗方案完成后 6、12、24 个月,比较两组在膝关节损伤与骨关节炎评分 (knee injury and osteoarthritis outcome score,KOOS ) 方面的差异。结果治疗后 6 个月,手术治疗组和物理治疗组疼痛、运动和娱乐、日常活动和 KOOS 总分评分均较术前明显改善,差异有统计学意义,其中物理治疗组疼痛由术前 46.35 改善至40.10 (P<0.001 )、运动和娱乐 21.45 上升至 42.60 (P<0.0001 )、日常活动由 27.85 上升至 41.75 (P<0.0001 )、KOOS 总分从 26.12 提高至 46.85 (P<0.0001 );镜下手术组疼痛由 47.05 改善至 33.25 (P<0.0001 )、运动和娱乐由 21.55 上升至 38.10 (P=0.002 )、日常活动由 26.00 上升至 46.84 (P<0.0001 )、KOOS 总分由 23.05 上升至 39.26 (P<0.0001 )。治疗后 12 个月与 6 个月相比,临床症状进一步缓解,差异有统计学意义,物理治疗组疼痛降至 29.20 (P<0.0001 )、运动和娱乐 (P=0.007 )、日常活动 (P<0.0001 )、KOOS 总分 (P=0.001 ) 分别上升至 53.16、53.10、50.90;镜下手术组疼痛降至 24.55 (P<0.001 )、运动和娱乐 (P<0.0001 )、日常活动(P<0.0001 )、KOOS 总分 (P<0.0001 ) 分别改善至 54.10、57.65、50.77。治疗后 24 个月,患者各项评分与术后 12 个月基本持平。不同随访阶段,尽管手术组整体评分优于物理治疗组,差异并无统计学意义 (P>0.05 )。结论随访2 年,未发现两组治疗后在功能改善和疼痛缓解方面存在显著差异,物疗治疗应视为退行性半月板撕裂的首选治疗方案。
半月板,胫骨;关节镜;膝损伤;前瞻性研究;康复;膝关节
随着影像学技术的发展,越来越多受膝关节疼痛和功能受限困扰的中年患者经 MRI 诊断为非创伤性、退行性半月板撕裂,部分伴有退行性骨关节炎。但就治疗而言,退行性半月板撕裂到底是否需要关节镜手术还是保守疗法即可,临床一直都存在争议。Jeffrey 等[1]和 Herrin 等[2]报道,退行性内侧半月板撕裂,伴有轻度骨关节炎患者,经关节镜下手术+物理治疗和单纯物理治疗组,随访期间发现疗效并无差异。国内尚未见报道。本研究旨在评估针对中老年退行性半月板撕裂,关节镜手术+物理治疗与单纯物理治疗相比是否具有优势。假设关节镜手术对患者康复无显著影响。
资料与方法
一、一般资料
2009 年 9 月至 2012 年 9 月,共经治 40 例。入院时根据数字随机法分为关节镜下手术+物理治疗组 (简称:镜下手术组 )、单纯物理治疗组 (简称:物理治疗组 ) 两组,每组 20 例。本组 40 例全部完成治疗计划,并获随访。本研究通过上海市第十人民医院伦理委员会审核。所有患者充分告知研究内容并签署知情同意书。
1. 入选标准:(1) 年龄 50~60 岁;(2) 近3 个月持续的膝关节疼痛和 (或 ) 关节活动受限;(3) 否认外伤病史;(4) 经 MRI 证实为半月板撕裂 (可伴有轻度骨关节炎 )。
2. 排除标准:(1) 有明确外伤史;(2) 合并严重的骨关节炎或类风湿关节炎等:(3) 合并膝关节不稳、韧带损伤、髌股关节炎等;(4) 既往患侧膝关节手术史。
所有患者在治疗前和治疗后第 6、12、24 个月患侧膝关节摄 X 线片评估骨关节炎变化。此外,还需按要求填写 KOOS 问卷[3]。以门诊随访,电话回访和信件寄回的形式获得问卷结果。这个评分主要包括五个方面:日常活动 (17 项 ),疼痛 (9 项 ),运动和娱乐功能 (7 项 ),症状 (7 项 ) 和膝关节相关的生活质量 (4 项 )。每个问题被分为 0~4 五个等级,每个方面得分和总分转化为标准分 (0~100 )。本研究仅对 KOOS 前3 项内容及相应总分进行比较,分值越高,说明患者症状越重。
由同一名高年资医师完成 20 例关节镜手术。所有患者术中采用腰麻和标准膝前入路,术中依次探查髌股关节、内外侧半月板、十字韧带、股骨内外侧髁及髁间窝。休整半月板撕裂的边缘,清除关节内游离体和碎片。充分负压吸引关节腔内积液后,注射利多卡因5 ml,复方倍他米松注射液1 ml,玻璃酸钠 40 ml。加压包扎。术后患者如能耐受疼痛可自行下地活动,不使用保护性支具。
理疗由我院康复科医师指导完成。两组患者接受相同的康复训练。每周进行2 次康复治疗,平均治疗时间为2 个月。具体理疗方案参照 Herrin 提出的康复流程[4]。
二、统计分析
分别于术前、术后 6、12、24 个月时,记录患者 KOOS 每个方面得分和总分并汇总转化为标准分。所有数据以平均值±标准差 (±s) 表示,统计学分析借助 STATA 11 (College Station,Texas 77845USA ) 进行分析。所得定量数据采用配对 t 检验分析,定性数据采用卡方检验。P<0.05 认为差异有统计学意义。
结 果
本组 40 例均获得平均 27 (10~46 ) 个月的随访。手术治疗组男女比例为 9 / 11,平均年龄(55.1±2.55 ) 岁,术前 13 例合并轻度骨关节炎;物理治疗组男女比例为 7 / 13,平均年龄 (53.2±2.78 )岁,术前 10 例合并轻度骨关节炎。两组性别、年龄、合并骨关节炎人数所占比例差异均无统计学意义 (P>0.05 ),具有可比性。
两组术前疼痛、运动和娱乐、日常活动和 KOOS总分评分差异均无统计学意义。术后 6、12 个月,手术治疗组和物理治疗组评分均较术前明显改善,差异有统计学意义;治疗后 12 个月所测得评分与术后 6 个月相比,各项参数值仍然持续下降,总的下降趋势不如术前 6 个月明显。治疗后 24 个月,患者各项主述症状与术后 12 个月相比差异无统计学意义。在比较不同随访阶段两组各项参数差异过程中,结果发现尽管手术组整体评分均优于物理治疗组,但差异并无统计学意义 (表1) (图 1,2 )。
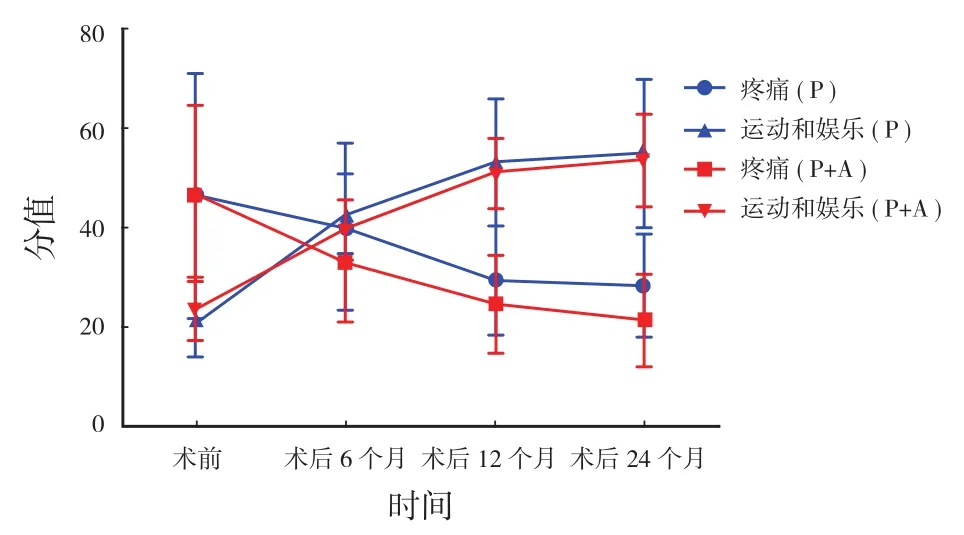
图1 各阶段疼痛、运动和娱乐分值变化 P (Physiotherapy ), P+A (Physiotherapy+Arthroplasty )Fig.1 The score changes of the pain and sports and entertainment at different stages P referred to Physiotherapy, and P+A referred to Physiotherapy+Arthroplasty
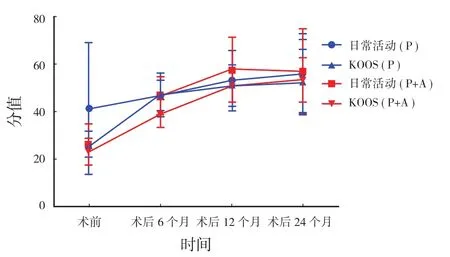
图2 各阶段日常生活、KOOS 总分分值变化 P (Physiotherapy ), P+A (Physiotherapy+Arthroplasty )Fig.2 The score changes of the daily activities and KOOS at different stages P referred to Physiotherapy, and P+A referred to Physiotherapy+Arthroplasty
表1 患者术前、术后 KOOS 评分数据 (±s)Tab.1 The KOOS scores of the patients before and after the operation (±s)
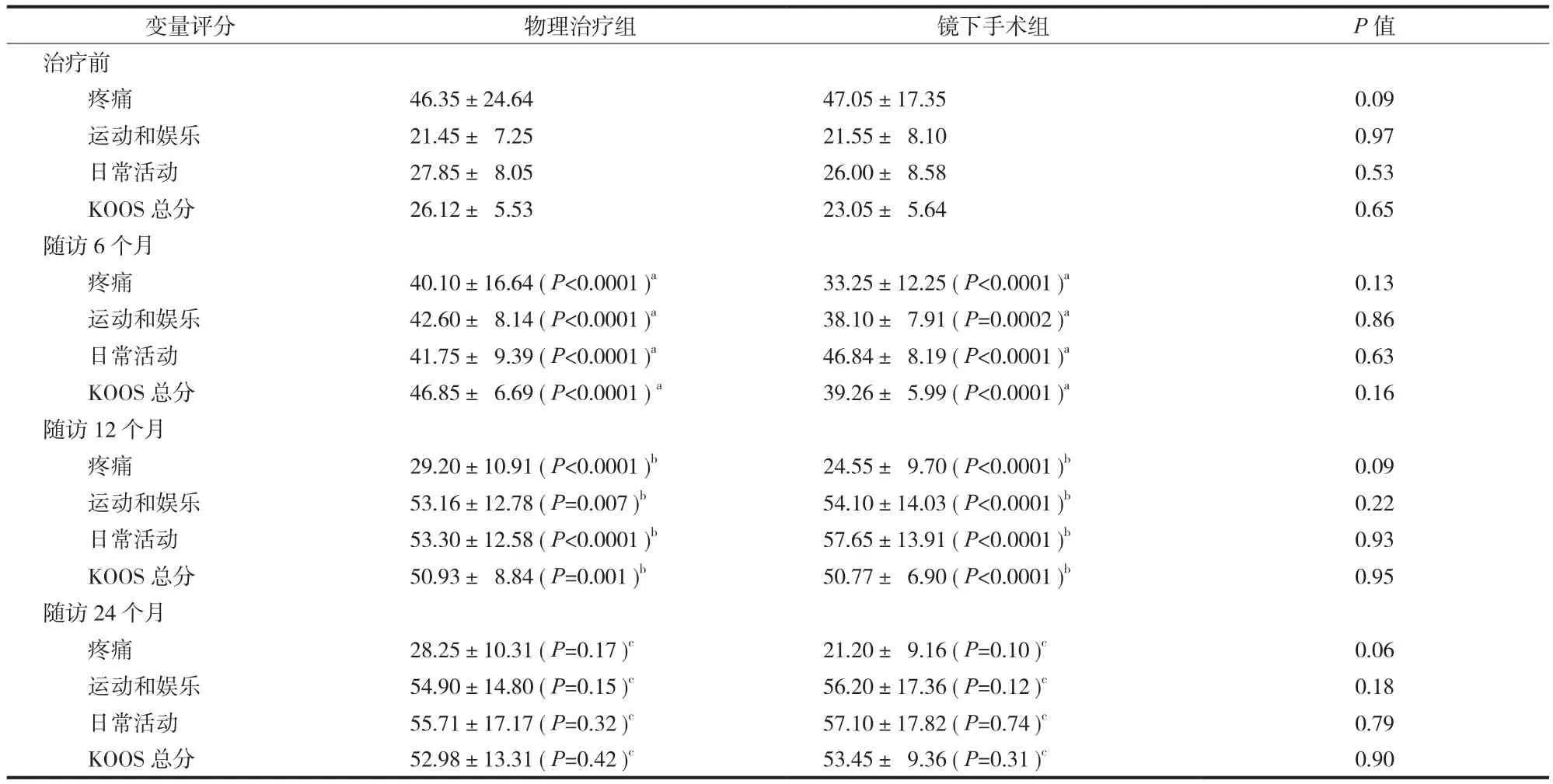
表1 患者术前、术后 KOOS 评分数据 (±s)Tab.1 The KOOS scores of the patients before and after the operation (±s)
注:治疗前与随访 KOOS 各项评分 (均数和标准差 )。a随访 6 个月与治疗前比较;b随访 12 个月与随访 6 个月比较;c随访 24 个月与随访 12 个月比较Notice: The KOOS scores of all the items before the treatment and during the follow-up (means & standard deviations).aReferred to the differences at 6 months after the treatment and before the treatment.bReferred the differences at 12 and 6 months after the treatment.cReferred to the differences at 24 and 12 months after the treatment
变量评分 物理治疗组 镜下手术组 P 值治疗前疼痛 46.35±24.64 47.05±17.35 0.09运动和娱乐 21.45± 7.25 21.55± 8.10 0.97日常活动 27.85± 8.05 26.00± 8.58 0.53 KOOS 总分 26.12± 5.53 23.05± 5.64 0.65随访 6 个月疼痛 40.10±16.64 (P<0.0001 )a 33.25±12.25 (P<0.0001 )a0.13运动和娱乐 42.60± 8.14 (P<0.0001 )a 38.10± 7.91 (P=0.0002 )a 0.86日常活动 41.75± 9.39 (P<0.0001 )a 46.84± 8.19 (P<0.0001 )a 0.63 KOOS 总分 46.85± 6.69 (P<0.0001 )a 39.26± 5.99 (P<0.0001 )a 0.16随访 12 个月疼痛 29.20±10.91 (P<0.0001 )b 24.55± 9.70 (P<0.0001 )b0.09运动和娱乐 53.16±12.78 (P=0.007 )b 54.10±14.03 (P<0.0001 )b 0.22日常活动 53.30±12.58 (P<0.0001 )b 57.65±13.91 (P<0.0001 )b 0.93 KOOS 总分 50.93± 8.84 (P=0.001 )b 50.77± 6.90 (P<0.0001 )b 0.95随访 24 个月疼痛 28.25±10.31 (P=0.17 )c 21.20± 9.16 (P=0.10 )c0.06运动和娱乐 54.90±14.80 (P=0.15 )c 56.20±17.36 (P=0.12 )c 0.18日常活动 55.71±17.17 (P=0.32 )c 57.10±17.82 (P=0.74 )c 0.79 KOOS 总分 52.98±13.31 (P=0.42 )c 53.45± 9.36 (P=0.31 )c 0.90
讨 论
在美国,每年有症状,且经影像学证实的膝关节骨关节炎患者约有 900 万例[5]。50 岁以上的人群中,半月板撕裂者高达 35%,其中三分之二都没有症状[6]。半月板损伤在患有骨关节炎的患者中患病率尤其高[7-8],临床通常都进行关节镜下的半月板部分切除。该手术方式主要通过休整撕裂的半月板,使其边缘变得稳定、平整。同样参照美国的数据,每年约有 46.5 万例接受这一手术[9]。既往 Kirkley等[10]和 Mosely 等[11]报道,关节镜手术治疗退行性骨关节炎,在给患者造成经济损失的同时并没有带来相应的临床疗效。而对于退行性半月板撕裂患者,是否具有关节镜手术指征以及术后疗效如何?尚有争议。
Jeffrey 等[1]在一项多中心随机对照研究中发现,年龄超过 45 岁伴有退行性半月板撕裂和轻中度半月板撕裂患者分别经关节镜手术+理疗和单纯理疗后 6、12 个月,患者膝关节功能和疼痛较治疗前明显改善,组间差异无统计学意义。尽管如此,他们还发现 35% 原先在的物理治疗组患者最终选择手术治疗,具体原因并未提及。另一项类似随机对照实验来自于 Herrlen 等[2],5 年随访结果,显示两组患者治疗后关节功能和疼痛改善情况有差异,但无统计学意义。本研究与上述两项研究所得出的结论保持一致。
由于半月板撕裂合并膝关节骨关节炎的患病率很高,并且两者都有可能没有任何症状,这对于临床决策来说是一个挑战,即使患者出现明显的临床症状,其症状是来自半月板撕裂,还是骨关节炎;或者两者兼有?排除术后功能恢复和疼痛改善的差异性,与手术+理疗相比,单纯理疗最明显的优势为减少手术带来的创伤和相关医疗费用。就 50 岁以上合并退行性半月板撕裂术后影像学评估,目前国内外尚无相关报道,后期我们将通过术后 MRI 检查随访患者半月板修复情况及其与疼痛和功能的相关性,进一步证实关节镜手术治疗退行性撕裂半月板的可行性及效价比。
通过以上研究,对于有临床症状且影像学证实退行性、非创伤性半月板撕裂伴或不伴有骨关节炎患者,关节镜手术和理疗在随访期间都能较好地改善功能、缓解疼痛。也就是说,对于这一类的患者,关节镜手术虽不是首选或者惟一的治疗选择,但仍是可行的治疗方案,尤其对于理疗等非手术治疗无效的患者。
[1]Katz JN, Brophy RH, Chaisson CE, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med, 2013, 368(18):1675-1684.
[2]Herrlin SV, Wange PO, Lapidus G, et al. Is arthroscopic surgery beneficial in treating non-traumatic, degenerative medial meniscal tears? A fve year follow-up. Knee Surg Sports Traumatol Arthrosc, 2013, 21(2):358-364.
[3]Roos EM, Roos HP, Ekdahl C, et al. Knee injury and osteoarthritis outcome score (KOOS)—validation of Swedish version. Scand J Med Sci Sports, 1998, 8:439-448.
[4]Herrlin S, Hållander M, Wange P, et al. Arthroscopic or conservative treatment of degenerative medial meniscal tears: a prospective randomisedtrial. KneeSurg Sports Traumatol Arthrosc, 2007, 15(4):393-401.
[5]Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Arthritis Rheum, 2008, 58:26-35.
[6]Englund M, Guermazi A, Gale D, et al. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med, 2008, 359:1108-1115.
[7]Bhattacharyya T, Gale D, Dewire P, et al. The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. J Bone Joint Surg Am, 2003, 85:4-9.
[8]Sowers M, Karvonen-Gutierrez CA, Jacobson JA, et al. Associations of anatomical measures from MRI with radiographically defined knee osteoarthritis score, pain, and physical functioning. J Bone Joint Surg Am, 2011, 93:241-251.
[9]Kim S, Bosque J, Meehan JP, et al. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am, 2011, 93:994-1000.
[10]Kirkley A, Birmingham T, Litchfield R, et al. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med, 2008, 359:1097-1107.
[11]Mosely JB, O’Malley K, Petersen N, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med, 2002, 2:81-88.
(本文编辑:李贵存 )
A prospective and comparative study of either physiotherapy along or accompanied arthroscopic surgery for degenerative meniscal tears
FU Dong, SHAN Lian-cheng, CAI Zheng-dong, LI Guo-dong. Department of Orthopaedics, Shanghai tenth People’s Hospital, Tongji University, Shanghai, 200072, PRC
ObjectiveTo evaluate whether physiotherapy along was superior to physical therapy accompanied by arthroscopic surgery in the treatment of degenerative meniscal tears. Methods A total of 40 patients of more than 50 years old were diagnosed as meniscal tears based on Magnetic Resonance Imaging (MRI ), and then were divided into2 treatment groups. The patients in the physical therapy accompanied by arthroscopic surgery group (n=20 ) received arthroscopic surgery and then postoperative physical therapy, and the patients in the physical therapy group (n=20 ) received physical therapy alone. The differences in the Knee Injury and Osteoarthritis Outcome Score (KOOS ) were compared between the2 groups at 6, 12 and 24 months after the treatment. Results At 6 months after the treatment, the pain, sports and entertainment, daily activities and KOOS scores both in the physical therapy accompanied by arthroscopic surgery group and in the physical therapy group were obviously improved when compared with the preoperative scores, and the differences between them were statistically signifcant. In the physical therapy group, the pain scores was improved from 46.35 points to 40.10 points (P<0.001 ), the sports and entertainment scores from 21.45 points to 42.60 points (P<0.0001 ), the scores of daily activities from 27.85 points to 41.75 points (P<0.0001 ) and the total KOOS from 26.12 points to 46.85 points (P<0.0001 ). In the physical therapy accompanied by arthroscopic surgery group, the pain scores was improved from 47.05 points to 33.25 points (P<0.0001 ), thesports and entertainment scores from 21.55 points to 38.10 points (P=0.002 ), the scores of daily activities from 26.00 points to 46.84 points (P<0.0001 ) and the total KOOS from 23.05 points to 39.26 points (P<0.0001 ). The clinical symptoms at 12 months after the treatment were further improved when compared with that at 6 months after the treatment, and the differences between them were statistically signifcant. In the physical therapy group, the pain scores was changed to 29.20 points (P<0.0001 ), the sports and entertainment scores to 53.16 points (P=0.007 ), the scores of daily activities to 53.10 points (P<0.0001 ) and the total KOOS to 50.90 points (P=0.001 ). In the physical therapy accompanied by arthroscopic surgery group, the pain scores was changed to 24.55 points (P<0.001 ), the sports and entertainment scores to 54.10 points (P<0.0001 ), the scores of daily activities to 57.65 points (P<0.0001 ) and the total KOOS to 50.77 points (P<0.0001 ). The scores of various items at 24 months after the treatment were almost equal to the scores at 12 months after the treatment. Although the overall scores in the physical therapy accompanied by arthroscopic surgery group were superior to that in the physical therapy group at different followup stages, the differences between them were not statistically signifcant (P>0.05 ).ConclusionsDuring the 2-year follow-up, no statistically signifcant differences are found in the functional improvement or pain relief between the2 groups. Physical therapy should be considered as the preferred treatment choice for degenerative meniscal tears.
Meniscus, tibia; Arthroscope; Knee injury; Prospective study; Rehabilitation; Knee joint
10.3969/j.issn.2095-252X.2014.06.006
R687.4
200072 上海,同济大学附属第十人民医院骨科 (付东,单连成,蔡郑,李国东 );200092 上海,同济大学生命科学与技术学院生物医学工程博士后流动站 (单连成 )
李国东,Email: tutumi89@126.com
2013-10-20 )