Predictive value and main determinants of abnormal features of intraoperative cholangiography during cholecystectomy
2011-07-03ShahramYousefpourAzaryHeshmatKalbasiAliSetayeshMirhadiMousaviAsadHashemiMahsaKhodadoostanMohammadRezaZaliandAmirHoushangMohammadAlizadeh
Shahram Yousefpour Azary, Heshmat Kalbasi, Ali Setayesh, Mirhadi Mousavi, Asad Hashemi, Mahsa Khodadoostan, Mohammad Reza Zali and Amir Houshang Mohammad Alizadeh
Tehran, Iran
Original Article / Biliary
Predictive value and main determinants of abnormal features of intraoperative cholangiography during cholecystectomy
Shahram Yousefpour Azary, Heshmat Kalbasi, Ali Setayesh, Mirhadi Mousavi, Asad Hashemi, Mahsa Khodadoostan, Mohammad Reza Zali and Amir Houshang Mohammad Alizadeh
Tehran, Iran
BACKGROUND:The major issue with intraoperative cholangiography (IOC) is whether its diagnostic accuracy for common bile duct (CBD) stones matches that of other diagnostic procedures, and thus, whether it will become a routine diagnostic procedure. The current study aimed to address the main determinants of CBD stone diagnosis in IOC among an Iranian population.
METHODS:In a retrospective review database-based study conducted in Taleghani Hospital in Tehran between 2006 and 2008, baseline data and perioperative information of 2060 patients (male to female ratio 542∶1518, mean age 53.7 years) who were candidates for cholecystectomy and underwent concomitant IOC for confirming CBD stones were reviewed. The predictive power of this procedure for diagnosis of abnormal biliary ducts with the focus on biliary stones was determined.
RESULTS:Overall mortality and morbidity following cholecystectomy in the study population were 0.6% and 2.6%, respectively. Both early mortality and morbidity due to cholecystectomy were higher in male than female. The prevalence of CBD stones in IOC was 3.4% (5.2% in male and 2.8% in female,P=0.008). Among those without gallstones, 8.7% had CBD stones and only 3.1% had concomitant gallstones and CBD stones. The main predictors of stone appearance as an abnormal feature of IOC during cholecystectomy were: advanced age (OR=1.022,P=0.001), male gender (OR=1.498,P=0.050), history of abdominal surgery (OR=1.543,P=0.040) and preoperative endoscopic retrograde cholangiopancreatography (OR=5.400,P<0.001).
CONCLUSIONS:IOC is a safe and accurate method for the assessment of bile duct anatomy and stones. Therefore, the routine use of IOC within cholecystectomy seems reasonable and is recommended.
(Hepatobiliary Pancreat Dis Int 2011; 10: 308-312)
intraoperative cholangiography; common bile duct stone; cholecystectomy; predictive value; diagnostic accuracy
Introduction
The presence of common bile duct (CBD) stones in patients undergoing cholecystectomy is a common problem, with a reported incidence of 5% to 15%.[1]In patients with suspected CBD stones, their identification before open or laparoscopic cholecystectomy plays an important role in extrahepatic biliary tree surgery. Unsuspected stones lying in the CBD that later in the hospital stay may necessitate common duct exploration remain the nemesis of the biliary tract surgeon. Studies of patients undergoing cholecystectomies demonstrate an incidence of choledolithiasis at the operating table of 7%-18%.[2-5]There are numerous options for preoperative or intraoperative diagnosis of suspected CBD stones, including conventional ultrasonography, liver function test (LFT), magnetic resonance cholangiography, endoscopic retrograde cholangiopancreatography (ERCP), and intraoperative cholangiography (IOC).[6-9]The optimal method for investigating suspected CBD stones has not yet been determined. IOC is an acceptable method for imaging the biliary tract. Routine IOC is a technique that can quickly and safely identify the bile duct anatomy and the presence or absence of bile duct stones. Although the method has been widely applied, there have been few large prospective evaluations of itsreliability in detecting CBD stones. Most studies have either been small, retrospective, or based on selected groups of patients. To our knowledge, no prospective population-based investigations have been carried out to determine the actual frequency of false-positive or false-negative findings on IOC and therefore its predictive value. Furthermore, predictors of the presence of CBD stones in IOC features have not been clearly determined. The current study aimed to address the main determinants of CBD stone diagnosis in IOC among an Iranian population.
Methods
From the database in Taleghani Hospital in Tehran between 2006 and 2008, we retrospectively reviewed the baseline data and perioperative information of 2060 patients (a male to female ratio of 542∶1518; mean age 53.7 years) who were candidates for cholecystectomy and underwent concomitant IOC for confirming bile duct stones. Exclusion criteria were other hepatobiliary disorders, incidental cholecystectomies performed concomitant with other major procedures, pregnancy, mental disability, and refusal to participate.
We reviewed the clinical data, laboratory data, and ultrasonographic findings. Variables studied included age, sex, type of surgery, duration of surgery, pathological features, characteristics of stone, and surgically-related mortality and morbidity. Preoperative evaluation included abdominal ultrasonography, routine lab tests, and LFTs. The indications for performing IOC were: history of jaundice, cholangitis or pancreatitis, abnormal LFTs, ultrasonographic evidence of CBD stone or dilatation, and obscure anatomy during cholecystectomy.
An abnormal cholangiogram was defined as any of the following: (1) CBD diameter >12 mm; (2) filling defect(s) in the CBD; (3) inadequate visualization of the lower end of the CBD; and/or (4) no contrast seen in the duodenum.
Statistical analysis
All statistical analyses were performed using SPSS version 16.0 for Windows (SPSS Inc., Chicago, IL, USA). Results were expressed as mean±standard deviation (SD) for quantitative variables and percentages for categorical variables. Categorical variables were compared using the chi-square test or Fisher's exact test. Continuous variables were compared by the independent samples t test or ANOVA. Multivariate analysis was carried out by binary logistic regression to determine the independent predictors for abnormal IOC diagnosis. P values ≤0.05 were considered statistically significant.
Results
The age of most patients ranged between 50 and 59 years. Regarding age distribution, male were older than female (Fig. 1). The overall prevalence of diabetes mellitus was similar in the two genders. Male were more likely to be addicts; however, a history of abdominal surgery was more common in female (Table 1). Abnormal parameters of white blood count, erythrocyte sedimentation rate and LFT were more frequent in male than female. Emergency surgery was performed more often in male than female. Furthermore, the time of surgery was longer in male. The prevalence of CBD stones in IOC was 3.4% (5.2% in male and 2.8% in female, P=0.008) (Table 2). No significant differences were found in the size and number of stones between the genders.
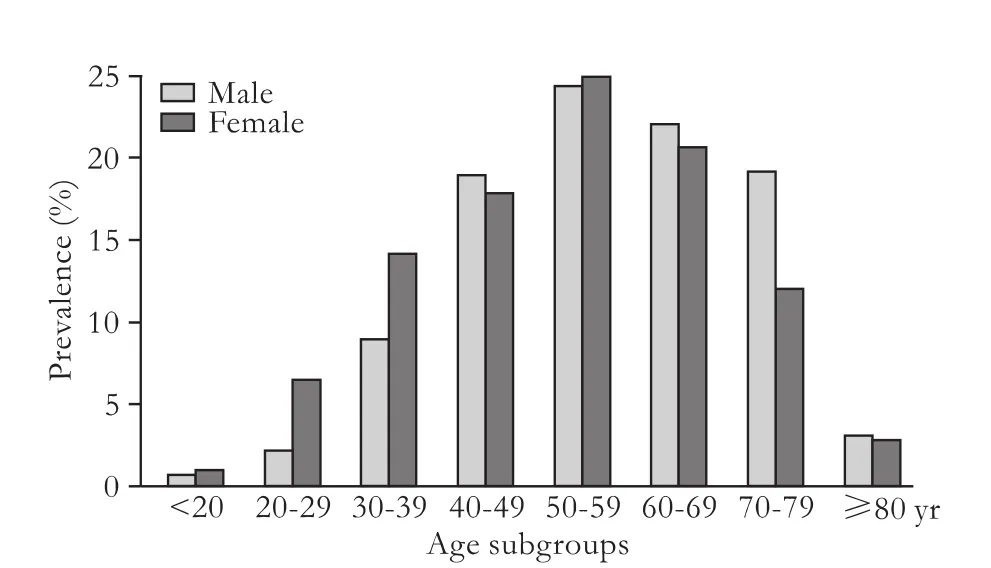
Fig. Age distribution of study patients.

Table 1. Medical history and chemical biomarkers (n, %)
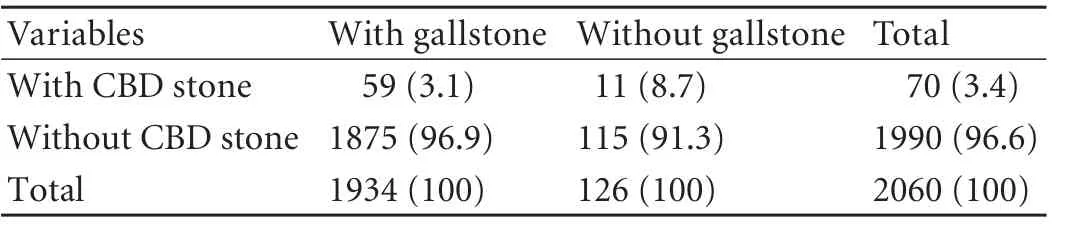
Table 2. Characteristics of biliary stones in IOC view in male and female (n, %)

Table 3. Early mortality and morbidity due to cholecystectomy in study male and female (n, %)
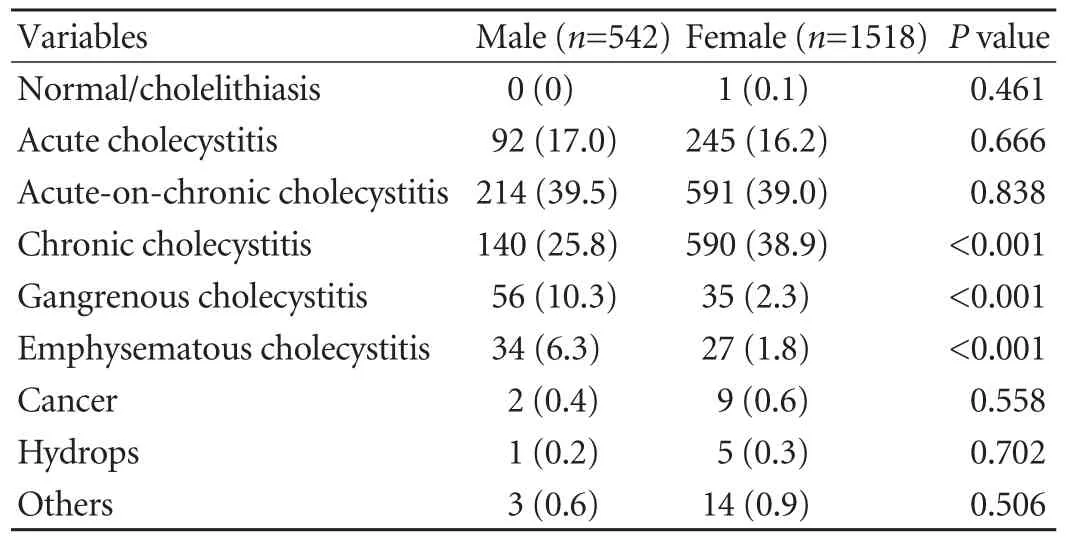
Table 4. Pathological findings following cholecystectomy in male and female (n, %)
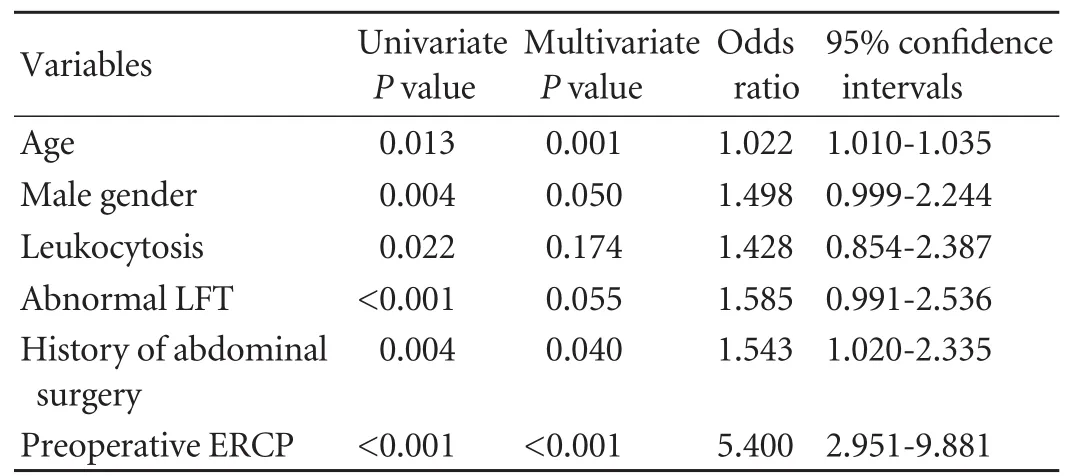
Table 5. Predictors of abnormal IOC due to diagnosis of stone in candidates for IOC during cholecystectomy in the presence of confounders
Overall mortality and morbidity following cholecystectomy in the study population were 0.6% and 2.6%, respectively. Both early mortality and morbidity due to cholecystectomy were higher in male than in female (Table 3). Regarding common pathological findings in those with hepatobiliary symptoms, the most common results were related to chronic cholecystitis in both genders. Chronic cholelithiasis occurred more frequently in female, whereas gangrenous cholecystitis and emphysematous cholecystitis were more common in male. Other findings were similar between them (Table 4).
Among those without gallstones, 8.7% had CBD stones and only 3.1% had concomitant gallstones and CBD stones. Regarding biomarker abnormalities and the appearance of CBD stones, there were no significant differences in the incidence of leukocytosis and erythrocyte sedimentation rate elevation between the patients with and without CBD stones. But LFT abnormalities were more prevalent in those with CBD stones than in the group without a diagnosis of CBD stones (58.6% versus 12.4%, P<0.001).
With respect to the relationship between the size of the cystic duct and the appearance of CBD stones, patients with a final diagnosis of CBD stones had a more dilated cystic duct than those without evidence of CBD stones (6.2±1.4 mm versus 5.3±1.4 mm, P<0.001).
The main predictors of stone appearance as abnormal features of IOC during cholecystectomy were advanced age (OR=1.022, P=0.001), male gender (OR=1.498, P=0.050), history of abdominal surgery (OR=1.543, P=0.040) and preoperative ERCP (OR=5.400, P<0.001) (Table 5).
Discussion
IOC continues to be an effective means of identifying CBD stones at the time of surgery. Recently, considerable discussion has focused on the role of IOC in the performance of cholecystectomy. The arguments in favor of routine IOC are many. The most important application remains its use for the selection of patients who have clinical indications for choledochotomy, yet may not be harboring stones at the time of surgery.[10]IOC is suggested by some to be a prerequisite to exploring the CBD. IOC which demonstrates a stone is usually helpful to confirm clinical impressions, whereas a normal cholangiogram in this series is always accurate.[11]
Despite the reported use of IOC in preventing transection of the CBD, its routine use has been, and remains, a matter of surgeon preference. Those surgeons who use IOC selectively (or not at all) suggest it is unnecessary to visualize the biliary system during every operation because prudent surgeons can avoid CBD injury without using it.[12]Selective IOC users believe it changes management in relatively few cases and apply it only in situations where choledocholithiasis is considered likely or among those they describe as a "high risk" for CBD injury.[13]Selective users highlight the added cost of IOC and a relatively small group of patients who benefit from either its protective effect or detection of small CBD stones (1.1% to 11.4% of patients might have stones, but their clinical significance is unknown). Routine IOC users argue it is impossible to predict who is at a highest risk for injury, making routine IOC the safer method.[14]
In the current survey, we evaluated the accuracy of IOC during cholecystectomy and tried to determine the predictive power of this procedure to detect bile ductabnormalities, especially biliary stones. Furthermore, we assessed the main determinants of abnormal IOC during cholecystectomy. At the first level, routine cholangiography on 2060 patients revealed a 3.4% incidence of suspected bile duct stones. In other similar studies by Levine[12]and Corbitt,[15]unsuspected stones were reported in 2.3% and 5.0% of participants, respectively. Review of the IOC literature revealed that the yield of unsuspected stones ranges from 0.9% to 10%, with most authors reporting values of 3% to 7%.[16-21]The ability to identify these stones or the lack of them remains the greatest technical success, defined as the ability to obtain a cholangiogram of sufficient quality to allow interpretation, which appears to be over 90% in most hands. According to our results, the use of IOC has a high sensitivity of 93.9%, a specificity of 89.7%, and positive and negative predictive values of 98.7% and 97.6%, respectively, in the detection of ductal stones. In a similar study by Videhult et al,[22]this procedure was successfully performed in 1117 patients (95%). In 154 (13%) of the patients, the IOC results were pathologic. CBD stones were common in 134 patients (11%). In 7 of the 134 patients in whom IOC indicated CBD stones, no stones could be verified at subsequent investigations (5% false-positive cholangiography). The reported incidence of false-positive cholangiograms still ranges from 2% to 16%. These results have also been reported elsewhere.[23]It is necessary to note that if IOC is to be performed selectively on the basis of specific criteria, these asymptomatic stones will be missed. However, most of these stones will not cause symptoms, and if they do, the surgeon can refer the patient for ERCP.[24]The point is that the statistically significantly higher negative predictive value for IOC in the detection of ductal stones means that a normal cholangiogram almost always implies a clear duct. It has been suggested that IOC can cause ductal complications. In our series, the complications attributable to the performance of IOC were minor and only caused IOC failure (a morbidity rate of 2.6%). One can hypothesize that IOC increases the possibility of postoperative pancreatitis. However, a 5-year study conducted by Traverso[25]showed that in their center, where the routine performance of IOC is a policy during cholecystectomy, postoperative pancreatitis is rare, as in our institution, and has no statistical relevance to the performance of IOC.
In conclusion, IOC is a safe, accurate, quick, and cost-effective method for the assessment of bile duct anatomy and stones. A highly disciplined performance of IOC, especially in the hands of an experienced laparoscopic surgeon, can well minimize the potentially debilitating and hazardous complications of bile duct injury. A normal cholangiogram, routinely performed, almost always means a clear bile duct and can prevent unnecessary postoperative ERCP and its potential complications for the symptoms that can be attributed to retained ductal stones. Also, the routine use of IOC seems to be reasonable and recommended. Bile duct stones are detected more frequently when IOC is used routinely rather than selectively. It seems that anticipatory management of these stones, which are often small and asymptomatic, is safe and cost-effective.
Funding:None.
Ethical approval: Not needed.
Contributors: YAS proposed the study, analyzed the data and wrote the first draft. All authors contributed to the design and interpretation of the study and to further drafts. ZMR is the guarantor.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Diagnosis and treatment of common bile duct stones (CBDS). Results of a consensus development conference. Scientific Committee of the European Association for Endoscopic Surgery (E.A.E.S.). Surg Endosc 1998;12:856-864.
2 Rábago LR, Vicente C, Soler F, Delgado M, Moral I, Guerra I, et al. Two-stage treatment with preoperative endoscopic retrograde cholangiopancreatography (ERCP) compared with singlestage treatment with intraoperative ERCP for patients with symptomatic cholelithiasis with possible choledocholithiasis. Endoscopy 2006;38:779-786.
3 Kuster GG, Gilroy SB. Intraoperative trans-gallbladder cholangiography intended to delineate bile duct anatomy. J Laparoendosc Surg 1995;5:377-384.
4 Glenn F. Common duct exploration for stones. Surg Gynecol Obstet 1952;95:431-438.
5 Hicken NF, Mallister AJ, Call DW. Residual choledochal stones; etiology and complications in one hundred ten cases. AMA Arch Surg 1954;68:643-656.
6 Barkum JS, Barkum A. Common presenting problem. 16 Jaundice, ACS book. 2004;256.
7 Nathanson LK, O'Rourke NA, Martin IJ, Fielding GA, Cowen AE, Roberts RK, et al. Postoperative ERCP versus laparoscopic choledochotomy for clearance of selected bile duct calculi: a randomized trial. Ann Surg 2005;242:188-192.
8 Dalton SJ, Balupuri S, Guest J. Routine magnetic resonance cholangiopancreatography and intra-operative cholangiogram in the evaluation of common bile duct stones. Ann R Coll Surg Engl 2005;87:469-470.
9 Basile L, Pezzoto C, Roubicek D, Tempra A, Laborda Molteni J. Magnetic resonance cholangiopancreatography: comparative study with direct cholangiography. Acta Gastroenterol Latinoam 2000;30:487-490.
10 Holmin T, Jönsson B, Lingren B, Olson SA, Petersson BG, Sörbris R, et al. Selective or routine intraoperative cholangiography: a cost-effectiveness analysis. World J Surg1980;4:315-322.
11 Livingston EH. Intraoperative cholangiography and risk of common bile duct injury. JAMA 2003;290:459-460.
12 Levine SB, Lerner HJ, Leifer ED, Lindheim SR. Intraoperative cholangiography. A review of indications and analysis of agesex groups. Ann Surg 1983;198:692-697.
13 Nies C, Bauknecht F, Groth C, Clerici T, Bartsch D, Lange J, et al. Intraoperative cholangiography as a routine method? A prospective, controlled, randomized study. Chirurg 1997;68: 892-897.
14 Singh G, Gupta PC, Sridar G, Katariya RN. Role of selective intra-operative cholangiography during cholecystectomy. Aust N Z J Surg 2000;70:106-109.
15 Corbitt JD Jr, Leonetti LA. One thousand and six consecutive laparoscopic intraoperative cholangiograms. JSLS 1997;1:13-16.
16 Hauer-Jensen M, Karesen R, Nygaard K, Solheim K, Amlie EJ, Havig O, et al. Prospective randomized study of routine intraoperative cholangiography during open cholecystectomy: long-term follow-up and multivariate analysis of predictors of choledocholithiasis. Surgery 1993;113:318-323.
17 Snow LL, Weinstein LS, Hannon JK, Lane DR. Evaluation of operative cholangiography in 2043 patients undergoing laparoscopic cholecystectomy: a case for the selective operative cholangiogram. Surg Endosc 2001;15:14-20.
18 Phillips EH, Berci G, Carroll B, Daykhovsky L, Sackier J, Paz-Partlow M. The importance of intraoperative cholangiography during laparoscopic cholecystectomy. Am Surg 1990;56:792-795.
19 Vezakis A, Davides D, Ammori BJ, Martin IG, Larvin M, McMahon MJ. Intraoperative cholangiography during laparoscopic cholecystectomy. Surg Endosc 2000;14:1118-1122.
20 Clair DG, Carr-Locke DL, Becker JM, Brooks DC. Routine cholangiography is not warranted during laparoscopic cholecystectomy. Arch Surg 1993;128:551-555.
21 Morgan S, Traverso LW. Intraoperative cholangiography and postoperative pancreatitis. Surg Endosc 2000;14:264-266.
22 Videhult P, Sandblom G, Rasmussen IC. How reliable is intraoperative cholangiography as a method for detecting common bile duct stones? A prospective population-based study on 1171 patients. Surg Endosc 2009;23:304-312.
23 Doyle PJ, Ward-McQuaid JN, Smith AM. The value of routine peroperative cholangiography--a report of 4000 cholecystectomies. Br J Surg 1982;69:617-619.
24 White TT, Hart MJ. Cholangiography and small duct injury. Am J Surg 1985;149:640-643.
25 Traverso LW. Intraoperative cholangiography lowers the risk of bile duct injury during cholecystectomy. Surg Endosc 2006;20:1659-1661.
Received May 4, 2010
Accepted after revision April 19, 2011
Author Affiliations: Research Center for Gastroenterology and Liver Diseases, Shahid Beheshti University of Medical Sciences, Taleghani Hospital, Tehran, Iran (Yousefpour Azary S, Mousavi M, Hashemi A, Khodadoostan M, Zali MR, Mohammad Alizadeh AH); and Arad General Hospital, Tehran, Iran (Kalbasi H and Setayesh A)
Amir Houshang Mohammad Alizadeh, Shahid Beheshti University of Medical Sciences, Taleghani Hospital, Parvaneh Ave., Tabnak St., Evin, Tehran, Iran 19857 (Tel: 0098-21-22432521; Fax: 0098-21-22432517; Email: ahmaliver@yahoo.com)
© 2011, Hepatobiliary Pancreat Dis Int. All rights reserved.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Hepatobiliary & Pancreatic Diseases International (HBPD INT)
- Iron overload and HFE gene mutations in Polish patients with liver cirrhosis
- Cytokine and apoptosis gene polymorphisms influence the outcome of hepatitis C virus infection
- Emergency re-routing of anterior sector venous outflow for right lobe living donor liver transplantation including the middle hepatic vein
- Long-term survival of a patient after resection of a gastrointestinal stromal tumor arising from the pancreas
- Persistent port-site sinus in a patient after laparoscopic cholecystectomy: watch out for gallbladder tuberculosis
