Single-port versus multi-port cholecystectomy for patients with acute cholecystitis: a retrospective comparative analysis
2011-07-03DietmarJacobandRolandRaakow
Dietmar Jacob and Roland Raakow
Berlin, Germany
Original Article / Biliary
Single-port versus multi-port cholecystectomy for patients with acute cholecystitis: a retrospective comparative analysis
Dietmar Jacob and Roland Raakow
Berlin, Germany
BACKGROUND:Trans-umbilical single-port laparoscopic cholecystectomy for chronic gallbladder disease is becoming increasingly accepted worldwide. But so far, no reports exist about the challenging single-port surgery for acute cholecystitis. The objective of this study was to describe our experience with single-port cholecystectomy in comparison to the conventional laparoscopic technique.
METHODS:Between August 2008 and March 2010, 73 patients with symptomatic gallbladder disease and histopathological signs of acute cholecystitis underwent laparoscopic cholecystectomy at our institution. Thirty-six patients were operated on with the single-port technique (SP group) and the data were compared with a control group of 37 patients who were treated with the multi-port technique (MP group).
RESULTS:The mean age in the SP group was 61.5 (range 21-81) years and in the MP group was 60 (range 21-94) (P=0.712). Gender, ASA status and BMI were not significantly different. The number of white blood cells was different before [SP: 9.2 (range 2.8-78.4); MP: 13.2 (range 4.4-28.6);P=0.001] and after the operation [SP: 7.8 (range 3.5-184.8); MP: 11.1 (range 5-20.8);P=0.002]. Mean operating time was 88 (range 34-174) minutes in the SP group vs 94 (range 39-209) minutes in the MP group (P=0.147). Four patients (5%) required conversion to an open procedure (SP: 1; MP: 3;P=0.320). During the followup period of 332 (range 29-570) days in the SP group and 428 (range 111-619) days in the MP group (P=0.044), eleven (15%) patients developed postoperative complications (P=0.745) and two patients in the SP group required reoperation (P=0.154).
CONCLUSIONS:Trans-umbilical single-port cholecystectomy for beginning acute cholecystitis is feasible and the complicationrate is comparable with the standard multi-port operation. In spite of our good results, these operations are difficult to perform and should only be done in high-volume centers for laparoscopic surgery with experience in single-port surgery.
(Hepatobiliary Pancreat Dis Int 2011; 10: 521-525)
laparoscopic surgery; single-port; cholecystectomy; acute cholecystitis
Introduction
The standard operation for gallbladder diseases worldwide is laparoscopic cholecystectomy with three or four ports. Because of visible scars in the upper abdominal wall, innovative methods such as natural orifice trans-luminal endoscopic surgery (NOTES) were introduced and the first results showed the technical feasibility of this operation.[1-4]An alternative approach for the treatment of laparoscopic cholecystectomy is by trans-umbilical access, which is described in the literature among others as laparoscopic single-site surgery (LESS).[5,6]Besides the positive cosmetic effect of the trans-umbilical incision, less pain has been reported recently.[7]So far, this procedure is becoming widely established as a potential new standard operation for gallbladder diseases and several reports have been published in the last two years on elective cholecystectomy.[8-12]Compared with the standard laparoscopic multi-port operation, single-port surgery shows similar results regarding conversion and complication rates. But most reports did not include many patients with clinical and histopathological signs of acute cholecystitis. This clinical condition is difficult to operate with the single-port technique, especially at a higher grade of inflammation. Diffuse bleeding and the complexity of hilar structures are limiting factors. Therefore, we performed a retrospective analysis of patients with a laparoscopic cholecystectomy using thesingle-port technique and compared our results with those from patients who underwent standard three-port cholecystectomy at our institution.
Methods
Patients
Between August 2008 and March 2010, 36 consecutive laparoscopic single-port cholecystectomies (single-port group; SP) were performed in patients with clinical and histopathological signs of acute cholecystitis within 48 hours after hospital admission. Collected prospective data were retrospective compared to a control group of 37 patients (multi-port group; MP) who underwent laparoscopic cholecystectomy during the same time with three trocars. Patients with signs of gallbladder perforation diagnosed by ultrasound or CT scan or with severe peritonitis were excluded from the study. Sixtyif ve patients were hospitalized as emergencies. Patients who were selected for the single-port procedure were completely informed about the technique and had the opportunity to choose the standard three-port procedure.
Surgical technique
Operating and assisting surgeons both stood on the left side of the patient. Both arms were rolled out and the monitor was placed opposite the surgeons near the right shoulder. The operation began with a longitudinal incision directly through the umbilicus between both umbilical edges (-1.5 to 2 cm). For a clear and safe closure of the linea alba at the end of the operation, the umbilicus had to be disconnected from the ground with scissors. After good exposure of the linea alba with small hooks, the linea alba was cut carefully with a scalpel at a length of -15 to 20 mm. After dissolving adhesions with the fingers, a Langenbeck's hook was used to retract the inferior part of the incision and the single port (TriPort, Olympus, Germany) was safely brought into the abdominal cavity with the TriPort injector introducer. After establishing the pneumoperitoneum up to 14 mmHg with CO2, a 30° 5- or 10-mm laparoscope was used for initial inspection of the abdominal cavity. We used conventional straight 5-mm graspers and a 5-mm hook electrocautery device as instruments. The right hand held the gallbladder with a grasper and the hilum was prepared with a hook electrocautery device to expose the cystic duct and cystic artery. Both structures were clipped with a 5-mm endoscopic clip applier (Ligamax 5 M/L, Ethicon Endo-surgery, OH, USA) and divided with scissors. After dissection of the gallbladder from the fossa, the bladder was removed through the TriPort system without an endobag. The fascial incision was closed with a non-absorbable 0 suture (Prolene®, Ethicon, Germany). Finally, skin closure was done with an absorbable 4/0 suture (Monocryl®, Ethicon, Germany).
In the control (MP) group, the operation was started with the same longitudinal incision directly through the umbilicus between both umbilical edges (-2 cm). A Veress needle was introduced into the abdominal cavity and a pneumoperitoneum up to 14 mmHg with CO2was established. One 10-mm optic trocar and two working trocars (5 and 10 mm) were inserted. At the end of the operation, the gallbladder was removed with an endobag.
Statistical analysis
All data were collected in a database (Microsoft Access 2.0; Microsoft, Seattle, WA, USA). Patient variables were: "American Society of Anesthesiologists" (ASA) status, hospital stay, age, body mass index (BMI), leukocytes, C-reactive protein, aspartate aminotransferase (AST) and γ-glutamyltransferase before and after operation, operation time, abscess formation, gallbladder perforation, local peritonitis, wound drainage, complications during the operation, grade of gallbladder inflammation (low, moderate, severe), chronic inflammation, and postoperative complications. The Mann-Whitney U test was used for analysis of continuous variables and the chisquare test for categorical variables by SPSS statistical software (SPSS 18.0, Chicago, IL, USA). Values for results of statistical analysis are expressed as means with range. A P value of less than 0.05 was considered statistically significant.
Results
Demographic data
The SP group included 19 (52%) male and 17 (48%) female patients with a median age of 61.5 (range 21-81) years, whereas 15 (40%) male and 22 (60%) female patients formed the MP group with a median age of 60 (range 21-94) years. Comparison of these groups did not show a significant difference in gender (P=0.298) and age (P=0.712). The condition of the patients before the operation was similar in both groups. The median ASA classification status was 2 (range 1-3) in the two groups (P=0.397). A detailed examination of the ASA classification in both groups showed that 8 patients (22%) had status 1, 22 (61%) status 2, and 6 (17%) status 3 in the SP group; while in the MP group 9 (24%) had status 1, 16 (43%) status 2, and 12 (33%) status 3. The median BMI in the SP group was 27.8 (range 19-40) and in the MP group was 27.4 (range 21-52) (P=0.313). Themedian hospital stay was 6 (range 4-20) days in the SP group and 6 (3-20) days in the MP group (P=0.596). Comparison of leukocytes and C-reactive protein before and after operation showed significantly increased levels in the MP group (Table 1). Six patients (17%) presented preoperatively with bile duct stones in the SP group and 10 (27%) in the MP group (P=0.288). In all 16 patients, endoscopic retrograde cholangiography (ERC) was performed. Five patients (14%) in the SP group had clinical signs of biliary pancreatitis in the medical history and 4 (11%) in the MP group. These results were not significantly different (P=0.691).
Operative details and complications
All patients received the same prophylactic antibiotic treatment with 2 g cefotaxim and 0.5 g metronidazol as an initial treatment. The operation times did not differ significantly and were 88 (range 34-174) minutes in the SP group and 94 (39-209) minutes in the MP group. During the operation there were no complications in either group. Previously performed abdominal surgery was noted in three patients (8%) in the SP group. One patient received a distal stomach resection, one had an open appendectomy, and one had an operation for an umbilical hernia. In contrast, eight patients (22%) in the MP group had a previous operation. Two patients had a partial resection of the intestine, one had a rightsided hemi-colectomy, two had appendectomies, one had suture of the stomach because of perforation, one had a hysterectomy, and one had a tumor debulking operationfor ovarian carcinoma. However, there was no significant difference in these patients (P=0.115). Ten patients (28%) in the SP group and three (8%) in the MP group had, as an incidental finding, a small umbilical hernia of between 5 and 15 mm. The difference was significant (P=0.029) and the umbilical hernia was sufficiently repaired within the standard procedure with a non-absorbable suture (Prolene 0, Ethicon, USA) after single-port surgery. One patient (3%) required conversion to the three-port technique because of a very large gallbladder with a deeply positioned hilus. An exact identification of the structures in the hilus via the single port was not possible. An open procedure was performed in one patient (3%) in the SP group because of a preoperatively unknown cholecystoduodenal fistula. This operation could not have been performed with the laparoscopic technique. In contrast, three patients (8%) in the MP group required a switch to open cholecystectomy. In two patients the hilus was not precisely identified and one patient developed permanent diffuse bleeding. Wound drainage was positioned at the end of the operation in four patients (11%) in the SP group and 25 (67%) in the MP group (P=0.001).

Table 1. Demographic data
During the follow-up, medical complications, wound infection, incisional hernia, new hospitalization and re-operation were noted. The rate of postoperative complications (P=0.745) and the number of reoperations (P=0.154) were not different between the two groups (Table 2). However, in the SP group two reoperations were performed. One patient had a fascial dehiscence, whichwas a technical fault. Wound closure was performed without any problems. The other patient developed ischemia of the bile duct as a major complication and received a bilioenteric anastomosis. He had Mirizzi's syndrome and we hypothesized that the pressure of the stone resulted in ischemia of the bile duct, because the lesion was at the anterior wall and surgery was not performed in this area.
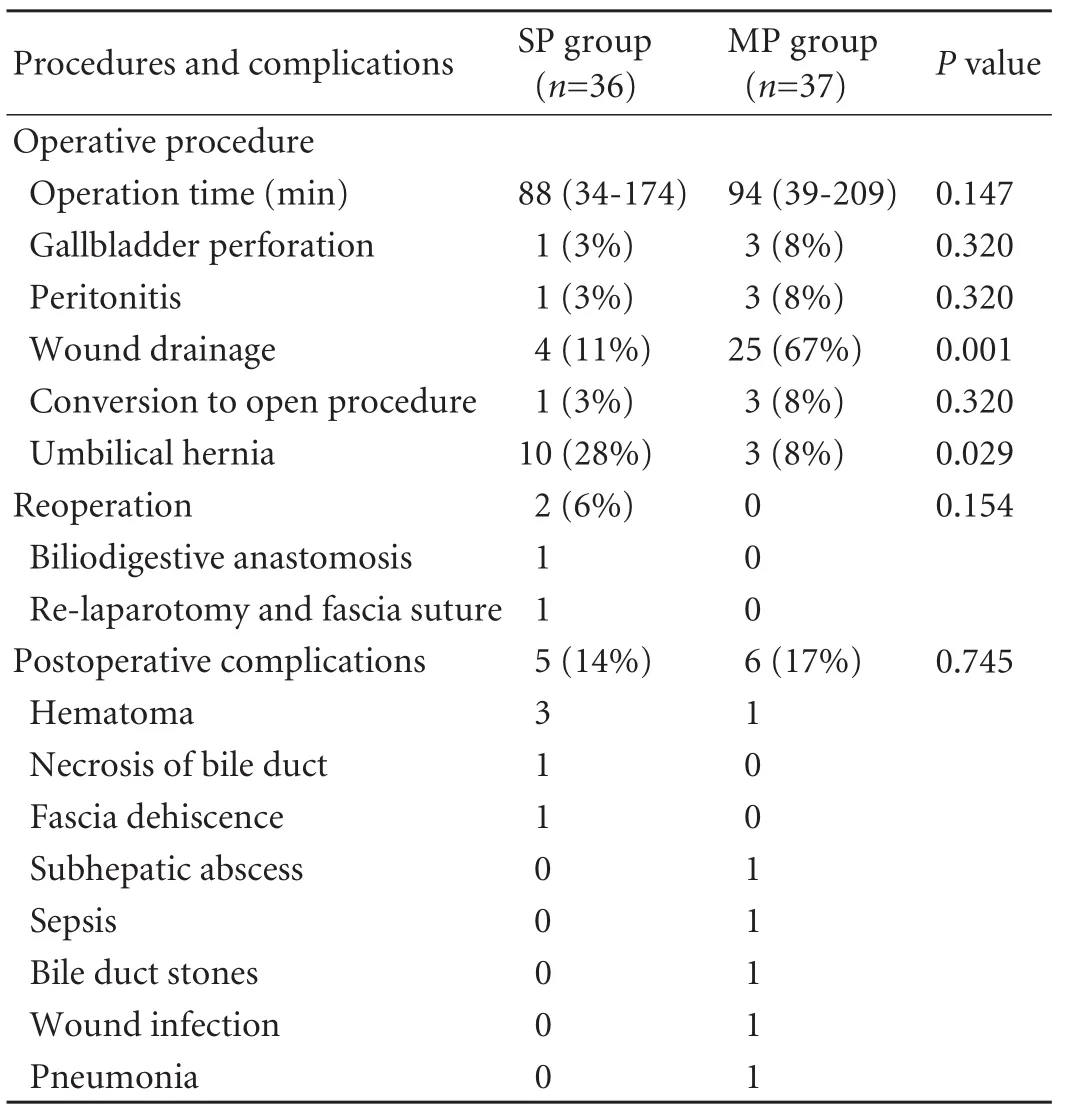
Table 2. Operative details and complications

Table 3. Pathological data
Pathology
Two experienced pathologists analyzed all specimens. The specimens showed an acute inflammation of the gallbladder. Classification of inflammation revealed a mild inflammation in no patients. Moderate inflammation was only diagnosed in four patients (11%) in the MP group, whereas severe inflammation was seen in all patients (100%) of the SP group and 33 in the MP group (P=0.044) (Table 3).
Discussion
Recently published literature[8-12]about single-port or single-incision cholecystectomy includes in most cases only patients with chronic gallbladder disease. Up to now, a large series of more than 100 patients in a singlecenter does not exist. In spite of the rapidly-growing development and application of single-incision surgery, this technique is still not the new standard. This might be the reason why surgeons do not operate on patients with acute cholecystitis via a single incision. Experience is lacking. We introduced the single-port technique as the new standard in October 2008 and because of our rapidly-growing knowledge and number of cases, we were not afraid of operating on the first patients with acute inflammation of the gallbladder. In most cases, the limited view is acceptable without risk for the patient.
For the correct comparison between both groups we included only patients with a histological diagnosis of moderate or severe acute inflammation. A review of our demographic data such as gender, age and ASA status showed a difference from recently published studies.[9,10,13-15]Our patients were considerably older and sicker than those reported by others. We had a median age of 61 years in the SP group and that of 60 years in the MP group. In addition, both groups were in inferior condition as measured by an average ASA status of 2. In contrast, most patients in other studies had a mean age of 33 to 47 years and, if known, the ASA status was 1.[8-12,15]Comparison of the two groups regarding these data did not show a significant difference. The results of operative details and especially complication rates were similar to studies on the MP technique with large patient numbers.[16-18]The conversion rate to an additional port or the multi-port technique was between 0% and 33% in former studies and 3% in our population.[11,12,15]One additional trocar was placed in a single-port operation because of a limited view of the hilus, which was hidden by a large left liver lobe. All in all, an open procedure was necessary in four patients. One patient in the SP group revealed a preoperatively unknown cholecystoduodenal fistula, which could not have been satisfactorily operated on with the laparoscopic technique. In comparison, three patients in the MP group were converted to a laparotomy. Two had a spontaneous perforation of the gallbladder at operation because of initial necrosis and the structures of the hilus were not visible. The other patient was in a reduced condition and developed diffuse bleeding. The view was too poor for laparoscopic surgery. Even although the conversion rate of three patients (8%) seems very high, it is notable that these patients had preoperatively known severe cholecystitis and most surgeons would not have started the operation using a laparoscopic technique. The conversion rate to an open procedure for single-port surgery is quite low in the literature, at 0 to 2%.[11,12,15,19]However, most patients are selected and in good condition. Therefore, these results are not significant and cannot be used for comparison with a standard procedure. A review of the complication rates after single-site surgery in the literature shows percentages between 0 and 5%.[8,13-15,20]Most complications are hematomas or seromas and can be treated conservatively. Major complications such as bile duct or vessel injuries are very rare and below 1%. In comparison, none of the patients in the MP group underwent operative revision of a complication. Up to now, there is only one report on a patient who received a second surgery because of an incisional hernia.[19]Podolsky et al[21]reported a two-year follow-up after single-incision surgery without any problems. However,the study only included 15 patients and the single-incision technique might not have the same risk for developing incisional hernia as the single-port technique with a 2-cm cut of the fascia.
In addition, we identified ten patients (28%) with an incidental umbilical hernia in the SP group versus three (8%) in the MP group. These values were significantly different. These hernias were safely repaired within the standard closure of the fascia using a non-absorbable suture. The operation time was not significantly different between the two groups. The reason might be the laparoscopic training of the participating surgeons. All of them were used to laparoscopic cholecystectomy with only three trocars as the standard procedure. Therefore, the learning curve for single-port cholecystectomy was much shorter for us than for surgeons who need four trocars.
In conclusion, we demonstrated that laparoscopic single-port cholecystectomy for acute cholecystitis is feasible and safe compared with the standard multi-port technique. But it is a challenging operation and should only be performed by surgeons with skills in single-port surgery. In addition, the best treatment option for each patient with acute inflammation should be individually discussed. Whether single-incision or single-port surgery is the new standard for cholecystectomy is still questionable. Therefore, we urgently need prospective randomized studies for acute and chronic gallbladder diseases.
Funding:None.
Ethical approval:Not needed.
Contributors:JD and RR performed the surgery and analyzed the data. JD wrote the manuscript. Both authors contributed to the design and interpretation of the study and to further drafts. JD is the guarantor.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Forgione A, Maggioni D, Sansonna F, Ferrari C, Di Lernia S, Citterio D, et al. Transvaginal endoscopic cholecystectomy in human beings: preliminary results. J Laparoendosc Adv Surg Tech A 2008;18:345-351.
2 Zorron R, Maggioni LC, Pombo L, Oliveira AL, Carvalho GL, Filgueiras M. NOTES transvaginal cholecystectomy: preliminary clinical application. Surg Endosc 2008;22:542-547.
3 Swain P. Nephrectomy and natural orifice translumenal endoscopy (NOTES): transvaginal, transgastric, transrectal, and transvesical approaches. J Endourol 2008;22:811-818.
4 Rattner D. Introduction to NOTES White Paper. Surg Endosc 2006;20:185.
5 Merchant AM, Cook MW, White BC, Davis SS, Sweeney JF, Lin E. Transumbilical Gelport access technique for performing single incision laparoscopic surgery (SILS). J Gastrointest Surg 2009;13:159-162.
6 Piskun G, Rajpal S. Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech A 1999;9:361-364.
7 Tsimoyiannis EC, Tsimogiannis KE, Pappas-Gogos G, Farantos C, Benetatos N, Mavridou P, et al. Different pain scores in single transumbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc 2010;24:1842-1848.
8 Hernandez JM, Morton CA, Ross S, Albrink M, Rosemurgy AS. Laparoendoscopic single site cholecystectomy: the first 100 patients. Am Surg 2009;75:681-686.
9 Kuon Lee S, You YK, Park JH, Kim HJ, Lee KK, Kim DG. Single-port transumbilical laparoscopic cholecystectomy: a preliminary study in 37 patients with gallbladder disease. J Laparoendosc Adv Surg Tech A 2009;19:495-499.
10 Rivas H, Varela E, Scott D. Single-incision laparoscopic cholecystectomy: initial evaluation of a large series of patients. Surg Endosc 2010;24:1403-1412.
11 Roberts KE, Solomon D, Duffy AJ, Bell RL. Single-incision laparoscopic cholecystectomy: a surgeon's initial experience with 56 consecutive cases and a review of the literature. J Gastrointest Surg 2010;14:506-510.
12 Vidal O, Valentini M, Espert JJ, Ginesta C, Jimeno J, Martinez A, et al. Laparoendoscopic single-site cholecystectomy: a safe and reproducible alternative. J Laparoendosc Adv Surg Tech A 2009;19:599-602.
13 Curcillo PG 2nd, Wu AS, Podolsky ER, Graybeal C, Katkhouda N, Saenz A, et al. Single-port-access (SPA) cholecystectomy: a multi-institutional report of the first 297 cases. Surg Endosc 2010;24:1854-1860.
14 Edwards C, Bradshaw A, Ahearne P, Dematos P, Humble T, Johnson R, et al. Single-incision laparoscopic cholecystectomy is feasible: initial experience with 80 cases. Surg Endosc 2010;24:2241-2247.
15 Solomon D, Bell RL, Duffy AJ, Roberts KE. Single-port cholecystectomy: small scar, short learning curve. Surg Endosc 2010;24:2954-2957.
16 Marakis GN, Pavlidis TE, Ballas K, Aimoniotou E, Psarras K, Karvounaris D, et al. Major complications during laparoscopic cholecystectomy. Int Surg 2007;92:142-146.
17 Duca S, Bala O, Al-Hajjar N, Lancu C, Puia IC, Munteanu D, et al. Laparoscopic cholecystectomy: incidents and complications. A retrospective analysis of 9542 consecutive laparoscopic operations. HPB (Oxford) 2003;5:152-158.
18 Herve J, Simoens Ch, Smets D, Ngongang Ch, Mendes da Costa P. Laparoscopic cholecystectomy; a retrospective 10-year study. Hepatogastroenterology 2007;54:1326-1330.
19 Romanelli JR, Roshek TB 3rd, Lynn DC, Earle DB. Singleport laparoscopic cholecystectomy: initial experience. Surg Endosc 2010;24:1374-1379.
20 Roy P, De A. Transumbilical multiple-port laparoscopic cholecystectomy (TUMP-LC): a prospective analysis of 50 initial patients. J Laparoendosc Adv Surg Tech A 2010;20: 211-217.
21 Podolsky ER, Rottman SJ, Curcillo PG 2nd. Single port access (SPA) cholecystectomy: two year follow-up. JSLS 2009;13:528-535.
Received May 12, 2011
Accepted after revision July 11, 2011
Author Affiliations: Department of Surgery, Center for Minimally Invasive Surgery, Vivantes Hospital Spandau, Neue Bergstrasse 6, 13585 Berlin, Germany (Jacob D); Department of Surgery, Vivantes Klinikum Am Urban, Dieffenbachstrasse 1, 10967 Berlin, Germany (Raakow R)
Dietmar Jacob, MD, Department of Surgery, Center for Minimally Invasive Surgery, Vivantes Hospital Spandau, Neue Bergstrasse 6, 13585 Berlin, Germany (Tel: 0049-30-130-13-2159; Fax: 0049-30-130-13-2154; Email: dietmar.jacob@vivantes.de)
© 2011, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(11)60088-X
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Hepatobiliary & Pancreatic Diseases International (HBPD INT)
- Protective effect of clodronate-containing liposomes on intestinal mucosal injury in rats with severe acute pancreatitis
- Collagen proportionate area of liver tissue determined by digital image analysis in patients with HBV-related decompensated cirrhosis
- Evaluation outcomes of donors in living donor liver transplantation: a single-center analysis of 132 donors
- Salvianolic acid B modulates the expression of drug-metabolizing enzymes in HepG2 cells
- Protective effect of probiotics on intestinal barrier function in malnourished rats after liver transplantation