Letter to the Editor
2011-07-03
Letter to the Editor
The Editor welcomes submissions for possible publication inthe Letters to the Editor section.
Letters commenting on an article published in the Journal or other interesting pieces will be considered if they are received within 6 weeks of the time the article was published. Authors of the article being commented on will begiven an opportunity to offer a timely response to the letter.Authors of letters will be notified that the letter has been received. Unpublished letters cannot be returned.
Hepatitis E virus-related acute liver failure associated with pure red cell aplasia
To the Editor:
Acute virus E hepatitis is a disease which is spread via fecal-oral transmission as the major route. Despite its high incidence rate in Asia, symptoms of the patient are generally less severe. However, among specific groups such as the elderly or expectant women, cholestatic hepatitis may occur after they are infected with hepatitis E virus (HEV) with a tendency for aggravation, even leading to acute liver failure.[1]In the course of infection, acute virus E hepatitis may also be associated with pure red cell aplasia (PRCA).
A 63-year-old Chinese man without blood disorders and liver disease had been healthy in the past. But fatigue occurred with lowered appetite later on. His skin and urine turned to be yellowish. Physical examination one week ago demonstrated yellowish body skin and sclera but no petechia or ecchymosis. The heart and lungs were normal, and the liver and spleen were not enlarged. However, edema was found in the lower limbs. Laboratory tests showed white blood cells (WBC) 9.1×109/L, N 0.782, red blood cells (RBC) 3.23×1012/L, hemoglobin 116 g/L, platelet 166×109/L, prothrombin time (PT) 15.8 seconds, ALB 26 g/L, TBIL 496.9 μmol/L, DBIL 343.7 μmol/L, ALT 737 U/L, AST 587 U/L, ALP 170 U/L, GGT 43 U/L, and TBA 71 μmol/L (Table). Other laboratory results were as follows: anti-hepatitis E virus-IgM(+), HBsAg(-), anti-HCV(-), anti-HAV-IgM(-), anti-HIV(-), anti-EBV-IgM(-) and anti-CMV-IgM(-), and Parvovirus B19-IgM(-). Chest X-ray was normal. Abdominal CT showed boosted liver echo and multiple liver cysts. A diagnosis was made of HEV-related acute liver failure.
Patient's TBIL and ALT gradually decreased during hospitalization. On the 15th day, hepatic encephalopathy occurred, and was subsequently relieved one day after treatment. On the 16th day, RBCs and hemoglobin count decreased gradually to the lowest on the 30th day. Lips were cyanotic but fever, vomiting, bloody diarrhea, or hemoglobinuria were not observed. Laboratory test showed RBC 1.3×1012/L, hemoglobin 46 g/L, reticulocyte red blood cell percentage 0.2%, platelet 117×109/L, and negative result of direct coombos test. On the 33rd day, bone marrow puncture showed active bone marrow proliferation and a G/E (granulocyte/erythroid) ratio of 79.5 (Fig. 1). Erythroid proliferation was significantly inhibited. Normoblasts and basophilic normoblasts were predominant while polychromatophilic normoblasts and orthochromatic normoblasts were observed occasionally. Megakaryocytes were normal. The result was consistent with the diagnosis of PRCA. On the 44th day, abdominal ultrasound B revealed ascites. Thus, comprehensive treatment of liver disease was prescribed and eventually the liver function of the patient was improved significantly with general regression of ascites. Moreover, red blood cells and hemoglobin recovered gradually. On the 70th day, laboratory test showed WBC 4.5×109/L, N 0.451, RBC 2.25×1012/L, HGB 87 g/L, platelet150×109/L, reticulocyte red blood cell percentage 2.4%, ALB 30 g/L, TBIL 45.5 μmol/L, DBIL 30.3 μmol/L, ALT 14 U/L, AST 28 U/L, ALP 145 U/L, GGT 20 U/L, TBA 53 μmol/L, and PT 13.5 seconds (Table, Fig. 2). Blood routine test showed WBC 4.7×109/L, N 0.482, RBC 3.9× 1012/L, hemoglobin 128 g/L, and platelet 162×109/L in two months after the patient was discharged.
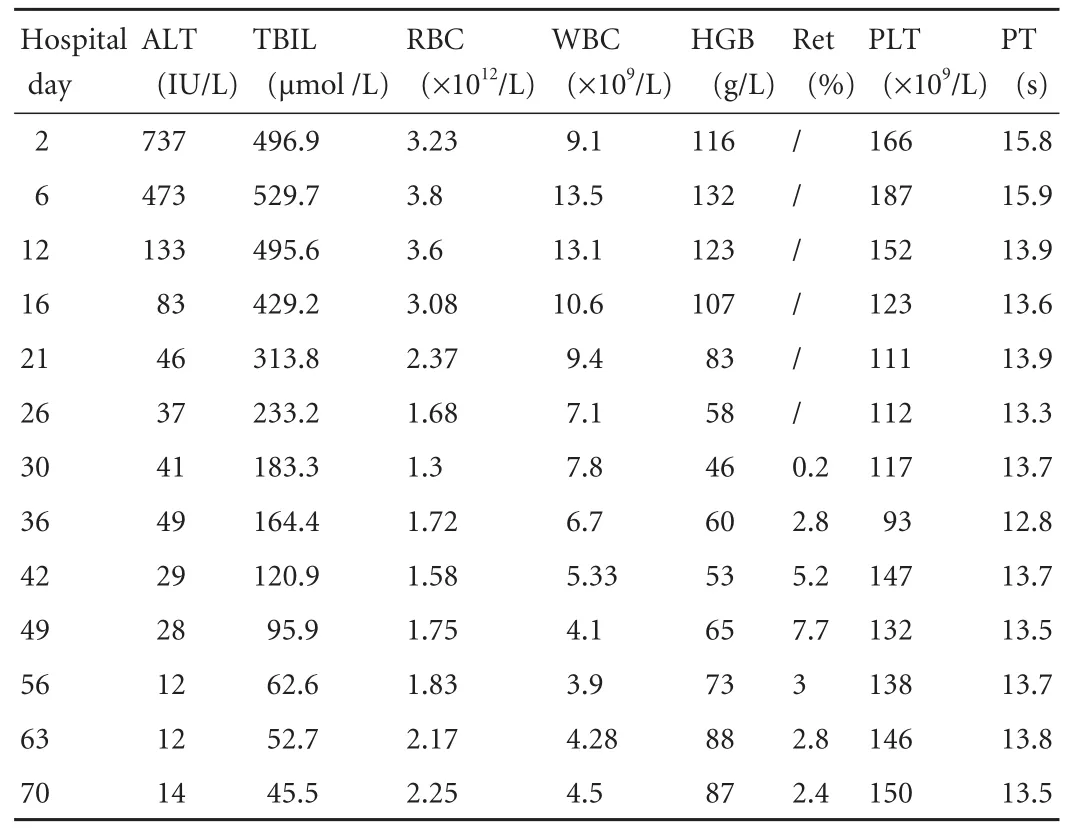
Table. The changes of ALT, TBIL, RBC, WBC, hemoglobin (HGB), reticulocyte red blood cell percentage (Ret), platelet (PLT), PT during hospitalization
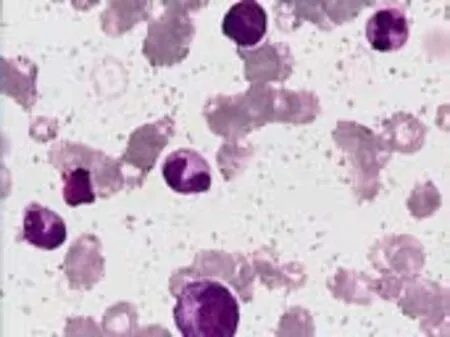
Fig. 1. Photomicrographs of bone marrow aspirate showing PRCA (original magnification ×100).
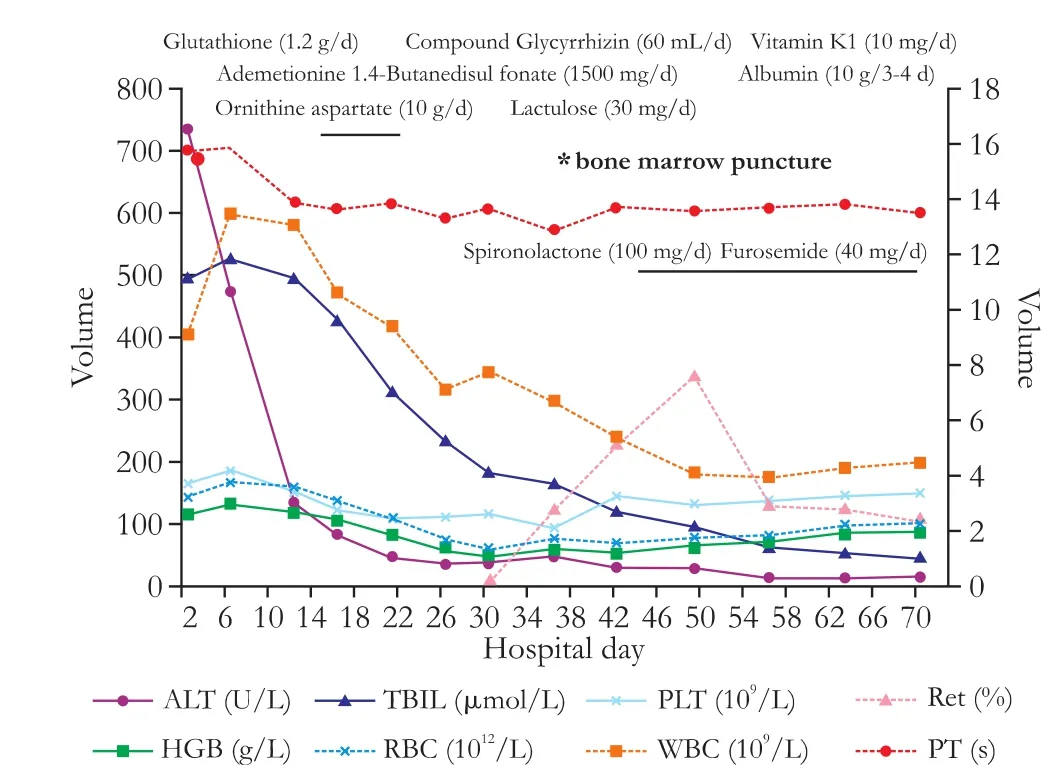
Fig. 2. The disease progress of the patient.
PRCA is a syndrome characterized by anemia, reticulocytopenia, and markedly reduced or absent erythroid progenitor cells in the bone marrow with preservation of the lymphoid and other hematopoietic lineages.[2]It may present as a primary hematological disorder in the absence of any other disease, or secondary to parvovirus infection, collagen vascular disease, leukemia, lymphoma, thymoma, solid tumors, treatment with recombinant human erythropoietin or other drugs, ABO-incompatible hematopoietic stem cell transplantation and pregnancy.[3]There are a few reports on viral hepatitis associated with PRCA, which mostly focus on patients infected with HAV or HCV associated with PRCA.[4,5]The present case is characterized by severe HEV infection in the elderly manifested by the stage of acute liver failure, and associated with PRCA during the course of HEV infection although PRCA is acute, self-limited, and eventually selfrelieved. Further investigation is needed to detect whether HEV infection is a direct factor leading to PRCA.
Chen Li and Hui-Fen Wang
Department of Liver Failure Treatment
and Research Center,
302 Hospital of PLA, Beijing, China
Tel: 86-10-66933012;
Fax: 86-10-66933434;
Email: wanghuifen302@126.com
1 Bernal W, Auzinger G, Dhawan A, Wendon J. Acute liver failure. Lancet 2010;376:190-201.
2 Charles RJ, Sabo KM, Kidd PG, Abkowitz JL. The pathophysiology of pure red cell aplasia: implications for therapy. Blood 1996;87: 4831-4838.
3 Sawada K, Fujishima N, Hirokawa M. Acquired pure red cell aplasia: updated review of treatment. Br J Haematol 2008;142: 505-514.
4 Schecter JM, Mears JG, Alobeid B, Gaglio PJ. Antierythropoietin antibody-mediated pure red cell aplasia in a living donor liver transplant recipient treated for hepatitis C virus. Liver Transpl 2007;13:1589-1592.
5 Chehal A, Sharara AI, Haidar HA, Haidar J, Bazarbachi A. Acute viral hepatitis A and parvovirus B19 infections complicated by pure red cell aplasia and autoimmune hemolytic anemia. J Hepatol 2002;37:163-165.
10.1016/S1499-3872(11)60096-9)
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Hepatobiliary & Pancreatic Diseases International (HBPD INT)
- Protective effect of clodronate-containing liposomes on intestinal mucosal injury in rats with severe acute pancreatitis
- Collagen proportionate area of liver tissue determined by digital image analysis in patients with HBV-related decompensated cirrhosis
- Evaluation outcomes of donors in living donor liver transplantation: a single-center analysis of 132 donors
- Salvianolic acid B modulates the expression of drug-metabolizing enzymes in HepG2 cells
- Protective effect of probiotics on intestinal barrier function in malnourished rats after liver transplantation