HiIar inflammatory pseudotumor mimicking hiIar choIangiocarcinoma
2010-06-29FeiTaoDengYanXuLiLunYeLingTongXiuPingYangandXinQunChai
Fei-Tao Deng, Yan-Xu Li, Lun Ye, Ling Tong, Xiu-Ping Yang and Xin-Qun Chai
Wuhan, China
HiIar inflammatory pseudotumor mimicking hiIar choIangiocarcinoma
Fei-Tao Deng, Yan-Xu Li, Lun Ye, Ling Tong, Xiu-Ping Yang and Xin-Qun Chai
Wuhan, China
BACKGROUND:Inflammatory pseudotumor of the biliary tract is a benign disease, and is extremely rare. Its diagnosis often depends on pathological examination after operation. The histopathological examination shows inflammatory lesions with a polymorphous infiltration and variable amounts of fibrous tissue. This study was undertaken to elucidate that an inflammatory pseudotumor in the right hepatic duct is especially difficult to distinguish from hilar cholangiocarcinoma.
METHOD:The clinical data of one patient with inflammatory pseudotumor of the right hepatic duct were analyzed.
RESULTS:An occupying lesion of the right hepatic duct was revealed by abdominal ultrasound and magnetic resonance cholangiopancreatography. The right hepatic duct inflammatory pseudotumor was not identified during the operation but was confirmed by postoperative histopathological analysis. The patient recovered well without any serious complication.
CONCLUSIONS:The preoperative evaluation for optimizing surgical management is important to the diagnosis of hepatobiliary occupying lesions. The evaluation involves clinical manifestations, imaging appearance and tumor markers. Malignant tumors and possible benign lesions should be considered to avoid aggressive surgical treatment.
(Hepatobiliary Pancreat Dis Int 2010; 9: 219-221)
inflammatory pseudotumor; cholangiocarcinoma; hepatic duct
Introduction
Inflammatory pseudotumor (IPT) arises most commonly from the lungs, but also from the stomach, intestinal mesenteries, and liver.[1-3]It is generally defined as a localized mass consisting of proliferating fibrovascular tissue infiltrated by inflammatory cells.[2-4]Biliary tumors located at the porta hepatis complicated with obstructive jaundice are mostly malignant hilar cholangiocarcinomas and require radical resection if possible. A few cases of benign inflammatory pseudotumor in the porta hepatis have been reported recently. The clinical manifestations and imaging appearance of the tumor are similar to those of a malignant neoplasm of the biliary tract. Hence the diagnosis of the tumor often depends on pathological examination after operation. In order to avoid aggressive surgical treatment, differential diagnosis of benign and malignant tumors should be made during the operation. We present a case of IPT located at the porta hepatis, mimicking cholangiocarcinoma. Surgical result was good, but if the preoperative evaluation had been more accurate and more comprehensive, this would have provided better instructive optimization for surgical management.
Case report
A 60-year-old man with diabetes was referred to the Department of Endocrinology, then transferred to our department after detection of a small lesion in the porta hepatis. On admission, he was free from symptoms and in good general health, without jaundice. The liver and spleen were not palpated and there was no sign of any abdominal mass.
Abnormal laboratory findings included total bilirubin 20.5 μmol/L, direct bilirubin 6.6 μmol/L, ALT 331 U/L, AST 147 U/L, alkaline phosphatase 189 U/L, α-fetoprotein (AFP) 4.9 μg/L, carcinoembryonic antigen 1.8 μg/L, and carbohydrate antigen 19-9 (CA19-9) 31.8 μg/L. Hepatitis serology for HBsAg and anti-HCV was negative.

Fig. 1. Mass-like lesions in the right hepatic bile duct.

Fig. 2. Magnetic resonance cholangiopancreatography image showing dilatation of the right hepatic intralobular bile duct associated with biliary obstruction at the right hepatic bile duct.
Abdominal ultrasound demonstrated a slight dilation in the right liver, and the right hepatic duct seemed to be obstructed.
The magnetic resonance imaging (Fig. 1) and magnetic resonance cholangiopancreatography (Fig. 2) showed abnormal signal re flection in the right liver near the porta hepatis. This abnormality together with the mild extension of the right hepatic intralobular bile duct, indicated a cholangiocarcinoma initially.
The patient underwent excision of the biliary ducts of the hepatic hilum and quadratic lobe, and Roux-en-Y cholangiojejunostomy. During the operation, we found that the common bile duct was not extended and a firm mass was palpated in the right hepatic duct. The left hepatic duct was unobstructed. A lymphoid node was found by the side of the common bile duct.
Macroscopically, the cut surface of the resected specimen demonstrated a yellowish-white tumor measuring 20×35 mm. Histologically, the tumor revealed granuloma tissue with lymphocyte in filtration, mainly by plasma cells, and a central band of myo fibroblastic proliferation (Fig. 3). These histological findings conif rmed a diagnosis of hepatic IPT of the plasma cell type. The patient recovered well after surgery.
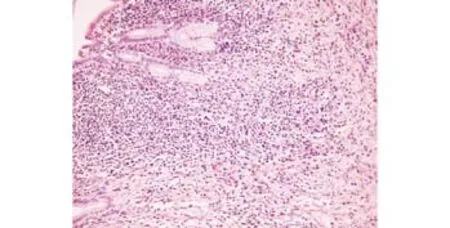
Fig. 3. Histopathological photomicrograph showing mixed inflammatory cell infiltrate of lymphocytes and eosinophils with a central band of myofibroblastic proliferation. These histological findings were consistent with a diagnosis of hepatic IPT (HE, original magnification ×100).
Discussion
Since the first case report by Pack and Baker in 1953,[4]more than 200 cases of hepatic IPT have been documented.[5]Hepatic IPT accounts for 0.4% of all focal liver lesions treated by hepatectomy.[6]IPT is a non-specific chronic inflammatory lesion of uncertain histogenesis. Some cases were reported to have Epstein-Barr virus positive inflammatory follicular dendritic cell tumors.[7-9]Hepatic IPT may result from recurrent cholangitis and be secondary to portal venous infection, and an inflammatory mass may be produced gradually together with obliterating phlebitis.[10,11]The clinical manifestations and imaging appearance of the tumor are similar to those of a neoplasm, but tumor differs from the malignant one in benign biological behavior and the property of spontaneous regression.[12,13]Macroscopically, the tumor is a firm, well-defined, white, grey or brownish-yellow, and non-encapsulated nodule. Microscopically patients with dense fibrous tissue is found with chronic inflammatory cells.[14]
Patients with IPT of the hepatic hilar biliary duct present with fever, jaundice, and manifestations indistinguishable from those of cholangiocarcinoma.[15-17]Tublin et al[18]analyzed the images of IPT from 7 cases, and found that the images of hepatic hilar biliary pseudotumor were also indistinguishable from those of cholangiocarcinoma. Venkataraman et al[19]reported the magnetic resonance images of hepatobiliary pseudotumor in 4 cases, and IPT was shown as a single or multiple focal mass lesion and an area of periportal soft-tissue infiltration either associated with or in the absence of focal lesions. They found that it was difficult to make a differentiation because there were considerable similarities between IPT and cholangiocarcinoma or lymphoma. Another paper reported an attempt tofind evidence by hepatic specific magnetic resonance imaging; however, no contrast medium entered IPT for the lack of hepatic cells in IPT tissue.[20]
As to tumor markers, the serum AFP level is within the normal range in patients with hepatic IPT[21]despite it is elevated in many patients with hepatocellular carcinoma. Thus, the serum AFP level could be helpful in differentiating hepatic IPT from hepatocellular carcinoma. Our patient showed a normal serum AFP level and a slightly elevated serum CA19-9 level. Since the increase of serum CA19-9 level is occasionally observed in patients with benign diseases of the hepatobiliary tract,[22]we suggest that CA19-9 is unsuitable for diagnosis of IPT.
Though hepatobiliary IPT is rare, hepatobiliary surgeons should know the disease well. Surgical resection of IPT can ensure a satisfactory prognosis. Patients with recurrent attacks of the disease and obstructive jaundice can receive good results after the resection. The extent of the resection depends on the intraoperative findings. The indicator of benign disease is the negative margin shown by fast frozen section analysis. Thus we recommend intraoperative examination of fast frozen section during IPT surgery.
Funding:None.
Ethical approval:Not needed.
Contributors:DFT, LYX and YL wrote the paper. DFT and CXQ analyzed the clinical data. TL and YXP performed the histological examination. CXQ is the guarantor.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Bahadori M, Liebow AA. Plasma cell granulomas of the lung. Cancer 1973;31:191-208.
2 Coffin CM, Watterson J, Priest JR, Dehner LP. Extrapulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor). A clinicopathologic and immunohistochemical study of 84 cases. Am J Surg Pathol 1995;19:859-872.
3 Chen KT. Inflammatory pseudotumor of the liver. Hum Pathol 1984;15:694-696.
4 Pack GT, Baker HW. Total right hepatic lobectomy; report of a case. Ann Surg 1953;138:253-258.
5 Gluszek S, Kot M, Czerwaty M. Inflammatory pseudotumor of the liver treated surgically. Hepatogastroenterology 1999;46: 2959-2960.
6 Torzilli G, Inoue K, Midorikawa Y, Hui AM, Takayama T, Makuuchi M. Inflammatory pseudotumors of the liver: prevalence and clinical impact in surgical patients. Hepatogastroenterology 2001;48:1118-1123.
7 Oz Puyan F, Bilgi S, Unlu E, Yalcin O, Altaner S, Demir M, et al.Inflammatory pseudotumor of the spleen with EBV positivity: report of a case. Eur J Haematol 2004;72:285-291.
8 Arber DA, Weiss LM, Chang KL. Detection of Epstein-Barr Virus in inflammatory pseudotumor. Semin Diagn Pathol 1998;15:155-160.
9 Lewis JT, Gaffney RL, Casey MB, Farrell MA, Morice WG, Macon WR. Inflammatory pseudotumor of the spleen associated with a clonal Epstein-Barr virus genome. Case report and review of the literature. Am J Clin Pathol 2003;120: 56-61.
10 Yoon KH, Ha HK, Lee JS, Suh JH, Kim MH, Kim PN, et al. Inflammatory pseudotumor of the liver in patients with recurrent pyogenic cholangitis: CT-histopathologic correlation. Radiology 1999;211:373-379.
11 Someren A. "Inflammatory pseudotumor" of liver with occlusive phlebitis: report of a case in a child and review of the literature. Am J Clin Pathol 1978;69:176-181.
12 Wick MR, Ritter JH. Pseudoneoplastic lesions: An Overview. In: Pathology of pseudoneoplastic lesions. Lippincott Raven Publishers; 1997:1-24.
13 Koide H, Sato K, Fukusato T, Kashiwabara K, Sunaga N, Tsuchiya T, et al. Spontaneous regression of hepatic inflammatory pseudotumor with primary biliary cirrhosis: case report and literature review. World J Gastroenterol 2006; 12:1645-1648.
14 Constantino Gde T, Sasaki F, Tavares RA, Voegels RL, Butugan O. Inflammatory pseudotumors of the paranasal sinuses. Braz J Otorhinolaryngol 2008;74:297-302.
15 Nonomura A, Minato H, Shimizu K, Kadoya M, Matsui O. Hepatic hilar inflammatory pseudotumor mimicking cholangiocarcinoma with cholangitis and phlebitis--a variant of primary sclerosing cholangitis? Pathol Res Pract 1997;193: 519-526.
16 Gohy S, Hubert C, Deprez P, Van Beers BE, Annet L, Lhommel R, et al. Benign biliary inflammatory pseudotumor mimicking a Klatskin tumor. Hepatogastroenterology 2007;54:1348-1352.
17 Saint-Paul MC, Hastier P, Baldini E, Chevallier A, Chevallier P, Gigante M, et al. Inflammatory pseudotumor of the intrahepatic biliary tract. Gastroenterol Clin Biol 1999;23:581-584.
18 Tublin ME, Moser AJ, Marsh JW, Gamblin TC. Biliary inflammatory pseudotumor: imaging features in seven patients. AJR Am J Roentgenol 2007;188:W44-48.
19 Venkataraman S, Semelka RC, Braga L, Danet IM, Woosley JT. Inflammatory myofibroblastic tumor of the hepatobiliary system: report of MR imaging appearance in four patients. Radiology 2003;227:758-763.
20 Mortelé KJ, Wiesner W, de Hemptinne B, Elewaut A, Praet M, Ros PR. Multifocal inflammatory pseudotumor of the liver: dynamic gadolinium-enhanced, ferumoxides-enhanced, and mangafodipir trisodium-enhanced MR imaging findings. Eur Radiol 2002;12:304-308.
21 White JE, Chase CW, Kelley JE, Brock WB, Clark MO. Inflammatory pseudotumor of the liver associated with extrahepatic infection. South Med J 1997;90:23-29.
22 Ogawa T, Yokoi H, Kawarada Y. A case of inflammatory pseudotumor of the liver causing elevated serum CA19-9 levels. Am J Gastroenterol 1998;93:2551-2555.
July 15, 2009
Accepted after revision December 3, 2009
Author Affiliations: Department of Hepatobiliary Surgery (Deng FT, Li YX, Yeland Chai XQ), and Department of Pathology (Tongland Yang XP), Union Hospital, Tongji Medical College, Huazhong Science and Technology University, Wuhan 430022, China
Xin-Qun Chai, MD, Department of Hepatobiliary Surgery, Union Hospital, Tongji Medical College, Huazhong Science and Technology University, Wuhan 430022, China (Tel: 86-27-85351623; Email: xinqunc@hotmail.com)
© 2010, Hepatobiliary Pancreat Dis Int. All rights reserved.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Protective effects of MCP-1 inhibitor on a rat model of severe acute pancreatitis
- Extrahepatic right hepatic duct diverticulum:a rare entity
- MRI shows clodronate-liposomes attenuating liver injury in rats with severe acute pancreatitis
- Preoperative assessment of hilar cholangiocarcinoma: combination of cholangiography and CT angiography
- Surgical therapy and prognosis of sarcomatoid carcinoma of the gallbladder
- Small-duct primary sclerosing cholangitis with hepatocellular carcinoma requiring liver transplantation
