Extrahepatic right hepatic duct diverticulum:a rare entity
2010-12-14EduardoSMFernandesRaquelBernardoMoacirFernandesRogrioMCArajoRenatoSebbeAsterioMonteJosCoelhoAntonioAPSouzaandJoaquimRibeiroFilho
Eduardo SM Fernandes, Raquel L Bernardo, Moacir M Fernandes, Rogério MC Araújo,Renato Sebbe, Asterio Monte, José F Coelho, Antonio AP Souza and Joaquim Ribeiro Filho
Rio de Janeiro, Brazil
Extrahepatic right hepatic duct diverticulum:a rare entity
Eduardo SM Fernandes, Raquel L Bernardo, Moacir M Fernandes, Rogério MC Araújo,Renato Sebbe, Asterio Monte, José F Coelho, Antonio AP Souza and Joaquim Ribeiro Filho
Rio de Janeiro, Brazil
(Hepatobiliary Pancreat Dis Int 2010; 9: 213-215)
choledochal cysts;hepatic duct diverticulum;Todani's classi fi cation;intrahepatic diverticulum
Introduction
Choledochal cyst (CC) was described by Douglas in 1852.[1]Alonzo-Lej proposed the classi fi cation of CCs 100 years later, and it was modi fi ed by Todani in 1977.[1]The last classi fi cation system remains used frequently.
Diverticulum arising from the hepatic duct is extremely rare, with only 4 cases reported so far.[2-11]Preoperative diverticular CC is diagnosed at laparotomy but this diagnosis is uncommon or dif fi cult to make.
We present a case of hepatic duct diverticulum,discuss its pathogenesis and positioning into Todani's classi fi cation, and review the relevant literature.
Case report
A 57-year-old woman came to our clinic with complaints of upper abdominal pain, nausea, and vomiting. She had no history of weight loss, jaundice, fever, diabetes,or arterial hypertension. An ultrasound scan showed multiple gallstones and normal hepatic ducts. She was referred to the Department of General Surgery for a laparoscopic cholecystectomy. During the procedure, a cystic structure was found in the upper part of Calot's triangle, diagnosed as right hepatic duct dilation by intraoperative cholangiography. She was referred to a hepatobiliary surgical unit after recovery. A right hepatic duct diverticulum was con fi rmed by MRI (Fig. 1).
Open laparotomy showed a 4-cm diverticulum containing biliary sludge arising from the extrahepatic portion of the right hepatic duct (Fig. 2), which was totally resected subsequently (Fig. 3). Intraoperative cholangioscopy did not show any abnormality involving the main hepatic duct, and the right hepatic duct was reconstructed with absorbable interrupted sutures. Pathological results were negative for dysplasia or carcinoma (Fig. 4).
There were no surgical complications, and thepatient was discharged on the 4th postoperative day. She was asymptomatic at her last follow-up visit 26 months after surgery.

Fig. 1. MRI cholangiography showing a right hepatic duct diverticulum.

Fig. 2. An open laparotomy showing a 4-cm diverticulum attached to the extrahepatic right duct.
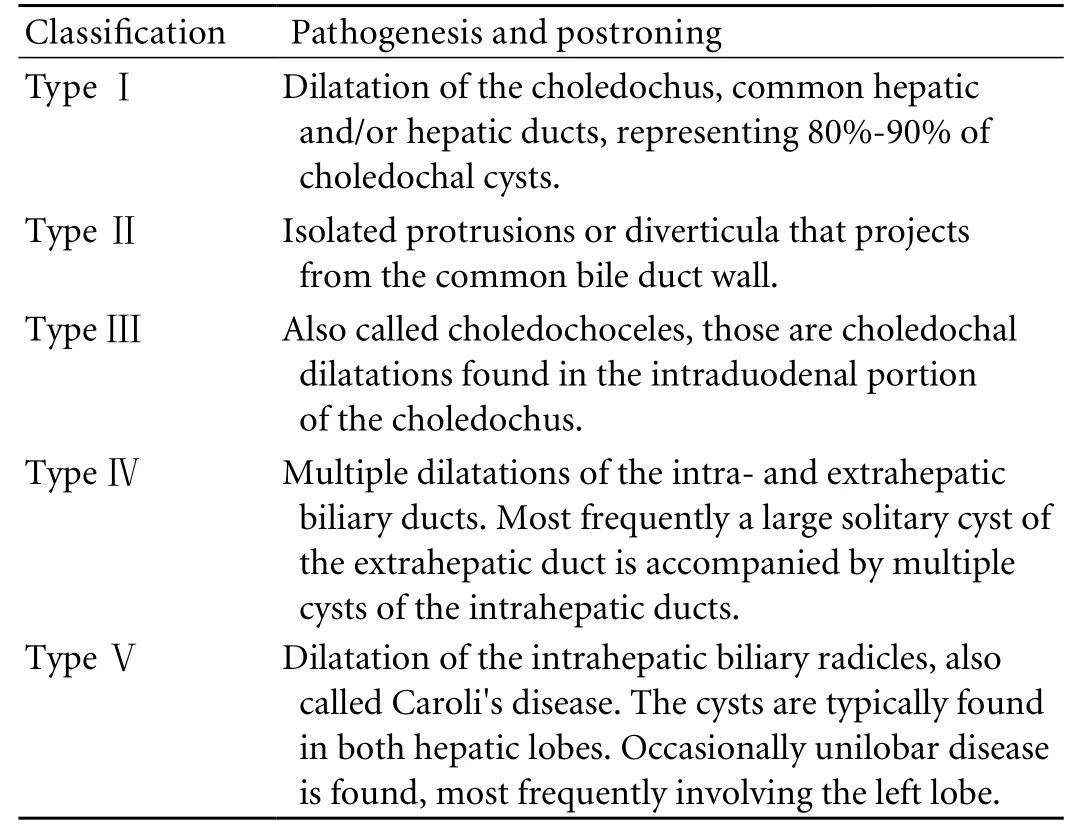
Table. Todani's classi fi cation for choledochal cysts
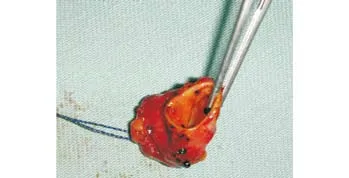
Fig. 3. The hepatic duct diverticulum after complete ressection.
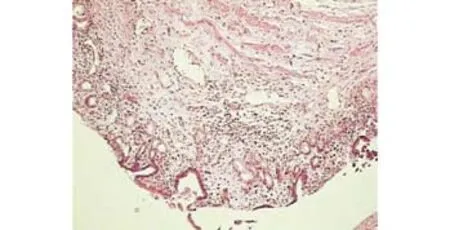
Fig. 4. The cyst wall showing fi brous tissue with mild lymphocytic inflammatory infiltrate, covered by glandular epithelium of the biliary type.
Discussion
The most accepted etiological theory for CC was described by Babbitt in 1969, based on anomalous relationships between the common bile duct and the pancreatic anlage.[1]Babbitt suggested that the anomalous junction between the main pancreatic duct and the choledochus creates a long common channel proximal to the entrance in the duodenal wall,predisposing to CC. The continuous re fl ux of pancreatic juice rich in lythic enzymes to the choledochus can cause its cystic dilation, with increased risks of cholangitis,cirrhosis, pancreatitis, and biliary tract cancer. This anatomic disposition was con fi rmed by other authors in 80%-90% of patients with CC[4-8]but the theory fails to explain CC in patients not presenting extra-duodenal pancreatobiliary duct junctions (10%-20%).
Todani's CC classi fi cation (Table) describes 5 anatomical variants, and is frequently used at present. Neither Todani's classi fi cation nor others include hepatic duct diverticulum.
The most effective imaging method for the diagnosis of bile duct diverticulum and anomalous pancreatobiliary duct junctions is endoscopic retrograde colangiography, but in some cases preoperative diagnosis remains uncertain and intraoperative cholangiography is essential.
Kaneyama et al[2]strongly recommend intraoperative cholangiography for the assessment of anatomical relationships and determination of surgical tactics.Total cyst excision is the ideal treatment because of the associated cancer risk, but the surgeon must decide whether the risk of neoplasia justi fi es the morbidity expected from total excision of the cyst in each individual patient. Based on the risk of cancer development we performed total excision on this case.
In conclusion, hepatic duct diverticulum is a rare condition, not included in the current classi fi cations for CC. A review of Todani's classi fi cation is necessary to include this type of cyst. The best imaging for preoperative diagnosis of CC and its best treatment must be determined. Further studies are required to answer these questions and to establish the ideal classi fi cation,diagnostic methodology, and treatment of hepatic duct diverticulum.
Funding: None.
Ethical approval: Not needed.
Contributors: FESM and BRL wrote the fi rst draft of this report.All authors contributed to the intellectual context and approved the fi nal version. FESM is the guarantor.
Competing interest: No bene fi ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Maksoud, JG. Cirurgia Pediátrica 1998 Ed. Revinter 879-888.
2 Kaneyama K, Yamataka A, Urao M, Kobayashi H, Lane GJ, Miyano T. An extremely rare case of symptomatic right hepatic duct diverticulum located outside the liver. Pediatr Surg Int 2005;21:1023-1026.
3 Hashimoto M, Umemura R, Okuda C, Matsuda M, Watanabe G. Hepatic duct diverticulum. Am J Surg 2007;193:219-220.
4 Jordan PH Jr, Goss JA Jr, Rosenberg WR, Woods KL. Some considerations for management of choledochal cysts. Am J Surg 2004;187:790-795.
5 Chijiiwa K, Koga A. Surgical management and long-term follow-up of patients with choledochal cysts. Am J Surg 1993;165:238-242.
6 Okada A, Nakamura T, Higaki J, Okumura K, Kamata S, Oguchi Y. Congenital dilatation of the bile duct in 100 instances and its relationship with anomalous junction. Surg Gynecol Obstet 1990;171:291-298.
7 Cheney M, Rustad DG, Lilly JR. Choledochal cyst. World J Surg 1985;9:244-249.
8 Komi N, Tamura T, Miyoshi Y, Kunitomo K, Udaka H,Takehara H. Nationwide survey of cases of choledochal cyst.Analysis of coexistent anomalies, complications and surgical treatment in 645 cases. Surg Gastroenterol 1984;3:69-73.
9 Jackson FC, Maxwell JW. Intrahepatic diverticulumcommon hepatic bile duct. Arch Surg 1964;89:706-708.
10 Meyers C, Reynes CJ, Freeark RJ. Diverticulum of the hepatic duct: a rare anomaly. Radiology 1976;119:38.
11 Flowers MB, Ho KJ. A rare common hepatic duct diverticulum causing fatal biliary obstruction and sepsis.Arch Pathol Lab Med 1998;122:197-198.
BACKGROUND: Douglas described choledochal cysts in 1852 and Todani proposed an anatomy-based classi fi cation in 1977.The classi fi cation is the most extensively used, but does not include some rare variations. We present a case of hepatic duct diverticulum, one of the variations, and discuss its diagnosis and treatment.
METHODS: A 57-year-old woman presented with upper abdominal pain and discomfort associated with nausea and vomiting. She was fi nally diagnosed with cholelithiasis and right hepatic duct diverticulum.
RESULT: The patient underwent resection of the hepatic duct diverticulum and cholecystectomy, and was asymptomatic 26 months after surgery.
CONCLUSIONS: Hepatic duct diverticulum is a rare form of choledochal cyst, not included in Todani's classi fi cation.Todani's classi fi cation including this and other uncommon variations of choledochal cysts must be reviewed. The best diagnostic imaging methods and treatment for choledochal cysts must be de fi ned.
Author Af fi liations: Department of General Surgery, Section of Hepatobiliary Surgery and Transplantation, Rio de Janeiro Federal University, Rio de Janeiro,Brazil (Fernandes ESM, Bernardo RL, Monte A, Coelho JF, Souza AAP and Ribeiro Filho J); Department of Digestive Surgery and Gastroenterology,Pio XII General Hospital, Sao Jose dos Campos, SP, Brazil (Fernandes ESM,Fernandes MM, Araújo RMC and Sebbe R)
Raquel L Bernardo, MD, Department of General Surgery, Section of Hepatobiliary Surgery and Transplantation, Rio de Janeiro Federal University, Rio de Janeiro, Brazil (Email: raq.lameira@gmail.com)
© 2010, Hepatobiliary Pancreat Dis Int. All rights reserved.
May 2, 2009
Accepted after revision February 13, 2010
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Delayed hepatocarcinogenesis through antiangiogenic intervention in the nuclear factor-kappa B activation pathway in rats
- Effect of blueberry on hepatic and immunological functions in mice
- Impact of human leukocyte antigen matching on hepatitis B virus recurrence after liver transplantation
- Prognostic models for acute liver failure
- Proteomic analysis of differentially expressed proteins involving in liver metastasis of human colorectal carcinoma
- Protective effects of MCP-1 inhibitor on a rat model of severe acute pancreatitis
