依折麦布片与阿托伐他汀钙片联合治疗对动脉粥样硬化性脑梗死患者血脂水平及神经功能的影响
2025-02-07丁猛猛解力杨静童琳吴翠翠方兰韩晓云李永安

【摘要】 目的:探讨依折麦布片与阿托伐他汀钙片联合治疗对动脉粥样硬化性脑梗死患者血脂水平及神经功能的影响。方法:选取2020年10月—2023年3月苏州市相城人民医院收治的80例急性动脉粥样硬化性脑梗死患者作为研究对象,通过随机数字表法将患者分为两组,各40例。对照组给予常规治疗+阿托伐他汀钙片;观察组给予常规治疗+阿托伐他汀钙片+依折麦布片。两组连续治疗12周。比较两组血脂水平、低密度脂蛋白胆固醇(LDL-C)达标率、神经功能及不良反应。结果:治疗后,两组总胆固醇(TC)、LDL-C、甘油三酯(TG)水平均低于治疗前,且观察组治疗后的TC、LDL-C、TG水平分别为(2.51±0.93)、(1.94±0.44)、(1.72±0.30)mmol/L,均低于对照组(Plt;0.05);治疗后,观察组HDL-C水平均高于治疗前与对照组,差异均有统计学意义(Plt;0.05)。治疗后,观察组LDL-C达标率为50.0%,高于对照组的25.0%(Plt;0.05)。治疗后,两组美国国立卫生研究院卒中量表(NIHSS)评分、改良Rankin量表(mRS)评分均低于治疗前,且观察组评分分别为(3.48±1.41)、(1.53±0.60)分,均低于对照组,差异均有统计学意义(Plt;0.05)。结论:联合应用依折麦布片与阿托伐他汀钙片对动脉粥样硬化性脑梗死的治疗,可以实现良好的降脂效果,有效降低TC、LDL-C、TG水平,并提高LDL-C达标率。
【关键词】 脑梗死 动脉粥样硬化 依折麦布片 阿托伐他汀钙片 血脂
Effect of Combined Treatment of Ezetimibe Tablets and Atorvastatin Calcium Tablets on Blood Lipid Level and Nerve Function in Patients with Atherosclerotic Cerebral Infarction/DING Mengmeng, XIE Li, YANG Jing, TONG Lin, WU Cuicui, FANG Lan, HAN Xiaoyun, LI Yong’an. //Medical Innovation of China, 2025, 22(03): -142
[Abstract] Objective: To investigate the effect of combined treatment of Ezetimibe Tablets and Atorvastatin Calcium Tablets on blood lipid level and nerve function in patients with atherosclerotic cerebral infarction. Method: Eighty patients with acute atherosclerotic cerebral infarction treated at Suzhou Xiangcheng People's Hospital from October 2020 to March 2023 were selected as the study subjects. According to the random number table method, the patients were divided into two groups, 40 cases in each group. The control group received standard treatment+Atorvastatin Calcium Tablets; the observation group was treated with standard therapy+Atorvastatin Calcium Tablets+Ezetimibe Tablets. Both groups were treated for 12 weeks. Blood lipid level, low density lipoprotein cholesterol (LDL-C) compliance rate, nerve function and adverse reactions were compared between the two groups. Result: After treatment, the levels of total cholesterol (TC), LDL-C and triglyceride (TG) in both groups were lower than those before treatment, and the levels of TC, LDL-C and TG in the observation group after treatment were (2.51±0.93), (1.94±0.44) and (1.72±0.30) mmol/L, respectively, which were lower than those in the control group (Plt;0.05). After treatment, HDL-C level in observation group was higher than that before treatment and control group, the differences were statistically significant (Plt;0.05). After treatment, the LDL-C compliance rate in the observation group was 50.0%, which was higher than 25.0% in control group (Plt;0.05). After treatment, the national institutes of health stroke scale (NIHSS) scores and modified Rankin scale (mRS) scores in both groups were lower than those before treatment, and the scores in the observation group were (3.48±1.41) and (1.53±0.60) scores, respectively, which were lower than those in the control group, with statistical significance (Plt;0.05). Conclusion: The combination of Ezetimibe Tablets and Atorvastatin Calcium Tablets in the treatment of atherosclerotic cerebral infarction can achieve a good lipid-lowering effect, effectively reduce the levels of TC, LDL-C and TG, increase the rate of LDL-C compliance.
[Key words] Cerebral infarction Atherosclerosis Ezetimibe Tablets Atorvastatin Calcium Tablets Blood lipid
First-author's address: Department of Neurology, Suzhou Xiangcheng People's Hospital, Suzhou 215100, China
doi:10.3969/j.issn.1674-4985.2025.03.032
急性缺血性脑卒中(acute ischemic stroke,AIS)约占我国脑卒中的70%[1],是危害公众健康的主要慢性疾病。面对我国动脉粥样硬化性血管疾病负担不断上升的趋势,血脂管理已刻不容缓。流行病学、遗传学和临床干预研究证据充分证实,低密度脂蛋白胆固醇(LDL-C)会对心血管疾病(ASCVD)产生重要影响[2]。同样也有研究证实LDL-C升高是急性脑梗死发生的独立危险因素[3],因此,LDL-C是心脑血管疾病二级预防血脂管理的重要目标。他汀类药物是血脂干预的基石,然而由于个体差异性,单用他汀已无法达到指南推荐的降脂目标。依折麦布作为一种新型的调脂药物,两者联用可以发挥优势互补的作用,达到强化降脂的目的。本研究通过评估依折麦布片与阿托伐他汀钙片联合治疗在动脉粥样硬化性脑梗死患者中的效果,旨在为临床提供更多依据和支持。
1 资料与方法
1.1 一般资料
研究对象为苏州市相城人民医院2020年10月—2023年3月收治的80例急性动脉粥样硬化性脑梗死患者,纳入标准:(1)符合文献[1]《中国急性缺血性脑卒中诊治指南2018》中急性动脉粥样硬化性脑梗死的诊断标准;(2)发病时间不超过72 h,且美国国立卫生研究院卒中量表(NIHSS)评分为5~20分;(3)TOAST病因分型为大动脉粥样硬化型;(4)年龄40~85岁;(5)无他汀治疗禁忌证;(6)临床资料完整。排除标准:(1)无神经功能缺损症状的脑梗死;(2)进行静脉溶栓;(3)有严重肝肾、免疫功能疾病;(4)过敏体质;(5)服用雌激素史。通过随机数字表法分为对照组和观察组,各40例。患者知情同意并签署知情同意书,本研究获得医院医学伦理委员会审核批准。
1.2 方法
给予对照组吸氧、心电监护、控制血压、控制血糖、营养脑细胞等常规治疗,并服用阿托伐他汀钙片(生产厂家:乐普制药科技有限公司,批准文号:国药准字H20163270,规格:20 mg/片),阿托伐他汀钙片起始剂量为10 mg,1次/d,剂量调整时间间隔至少4周,最大剂量为80 mg,1次/d。观察组在对照组的基础上联合应用依折麦布片(生产厂家:杭州默沙东制药有限公司,批准文号:国药准字J20171023,规格:10 mg/片)。依折麦布片的剂量为10 mg,1次/d。两组均治疗12周。
1.3 观察指标及评价标准
(1)血脂水平:采用全自动生化分析仪,检测总胆固醇(TC)、甘油三酯(TG)、高密度脂蛋白胆固醇(HDL-C)、LDL-C;(2)NIHSS与改良Rankin量表(mRS)评分。NIHSS:0~42分,分数越高神经功能缺损程度越严重。mRS:评分范围从0分(无残疾)到6分(死亡);(3)LDL-C达标率:LDL-Clt;1.8 mmol/L或降脂幅度50%视为降脂达标[4-5];(4)不良反应发生情况,包括胃肠道反应、药物性肝肾损伤、肌肉酸痛等。
1.4 统计学处理
运用SPSS 28.0处理数据,计数资料表示为率(%),进行字2检验;计量资料表示为(x±s),符合正态分布,组内比较采用配对样本t检验,组间比较采用独立样本t检验。Plt;0.05说明差异有统计学意义。
2 结果
2.1 两组基线资料比较
两组基线资料比较,差异均无统计学意义(Pgt;0.05),具有可比性,见表1。
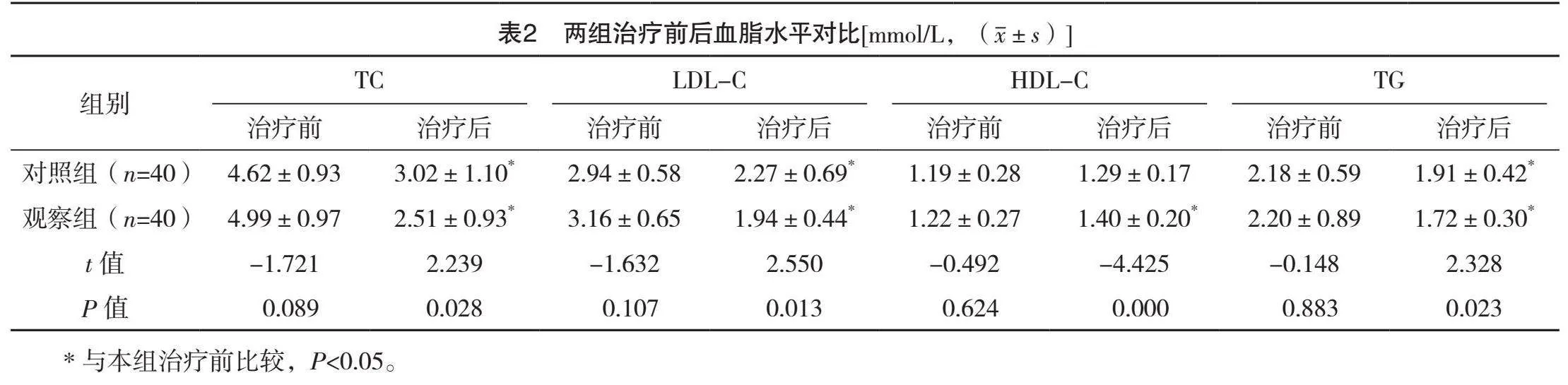
2.2 两组治疗前后血脂水平比较
治疗前,两组TC、LDL-C、HDL-C、TG比较,差异均无统计学意义(Pgt;0.05);治疗后,两组TC、LDL-C、TG均低于治疗前,观察组HDL-C水平高于治疗前(Plt;0.05);治疗后,观察组TC、LDL-C、TG均较对照组低,HDL-C水平高于对照组,差异均有统计学意义(Plt;0.05)。见表2。
2.3 两组LDL-C达标率比较
治疗后,观察组和对照组的LDL-C达标率分别为50.0%(20/40)和25.0%(10/40),观察组较对照组高,差异有统计学意义(字2=5.333,P=0.021)。
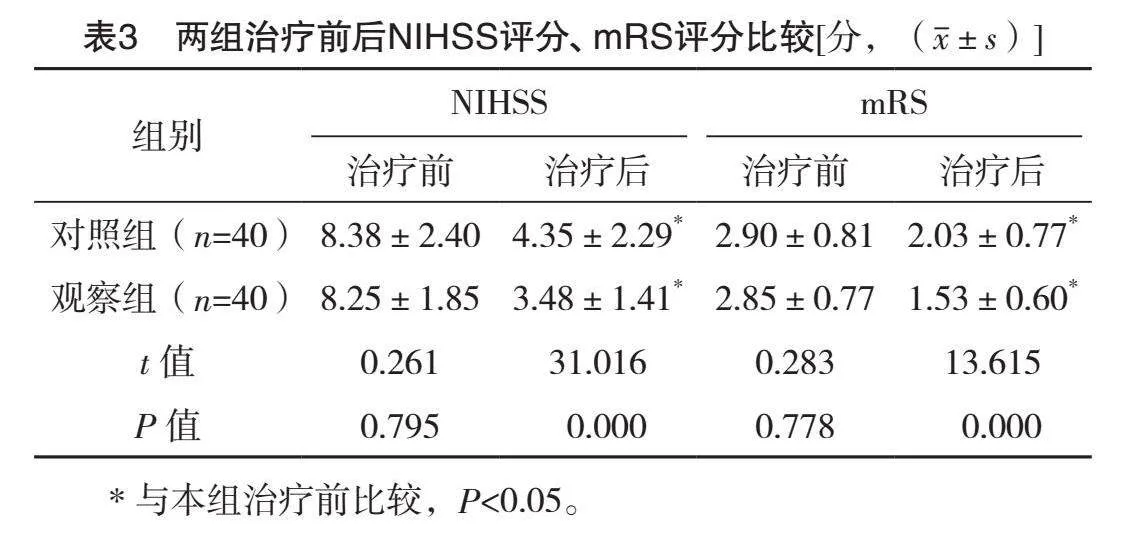
2.4 两组治疗前后NIHSS、mRS评分比较
两组治疗前的NIHSS、mRS评分比较,差异均无统计学意义(Pgt;0.05);治疗后,两组NIHSS、mRS评分均低于治疗前,且观察组均低于对照组,差异均有统计学意义(Plt;0.05)。见表3。
2.5 两组不良反应发生情况
对照组中有1例患者显示丙氨酸氨基转移酶轻微升高,但是未超过临床正常值的上限3倍以上,因此无停药指征,治疗完成后复查恢复正常范围。研究组中有1例患者显示丙氨酸氨基转移酶轻微升高,治疗完成后复查均恢复正常范围。所有患者均未出现严重的胃肠道反应、药物性肝肾损伤、肌肉酸痛等不良反应。
3 讨论
急性脑梗死(acute cerebral infarction,ACI)是因脑动脉血流中断导致的相应脑供血区域神经功能障碍[6-7]。动脉粥样硬化斑块是脂质沉积、炎症变化、细胞迁移和动脉壁损伤等复杂相互作用的结果,其形成是动脉粥样硬化性心脑血管疾病的病理生理驱动因素。因此,抑制斑块生成和稳定现有斑块是减少心脑血管事件发生的重要治疗措施。颈动脉是动脉粥样硬化斑块形成最常受累的血管,颈动脉斑块的稳定性直接影响着ACI的发生及转归。血脂代谢异常是动脉粥样硬化形成的重要危险因素,因此血脂管理应引起临床医生的重点关注。他汀类药物是脑卒中二级预防的一线药物,有研究表明,动脉粥样硬化患者经过他汀类药物治疗后,LDL-C和TG水平均降低,死亡风险下降,并改善临床预后[8-9]。既往研究证实LDL-C升高是脑梗死发生的一项独立危险因素[3],可以显著增加脑梗死的发病风险[10],因而LDL-C是降低脑卒中风险的主要脂质治疗靶点。Meta分析发现,随着LDL-C降低到较低的水平,卒中风险也随之降低[11-12]。JAMA子刊上的一项Meta分析显示在强化降低LDL-C上,高强度他汀类药物治疗在降低复发性卒中风险和临床获益方面优于低强度的他汀类药物[13]。在临床实践中,临床医生常遇到脑卒中患者长期口服他汀而LDL-C仍未达标的情况,易再发卒中[14],以及遇到许多高危或极高危风险的患者其LDL-C未能达标,无法获得理想的降脂效果。由此,联合治疗可作为强化降低LDL-C的补充方案。依折麦布可作用于小肠上皮细胞刷状缘,抑制食物中胆固醇跨小肠转运吸收。而他汀类药物通过抑制胆固醇合成的关键酶活性,降低肝细胞中胆固醇的生成,并加速血中LDL-C的分解。他汀类药物和依折麦布作用于胆固醇代谢的内源性和外源性2个不同途径,两者联用可产生良好的协同作用,达到更强的、更综合的降脂效果。Kim等[15]发现依折麦布联用瑞舒伐他汀在降低LDL-C、TC和TG水平方面明显优于单用瑞舒伐他汀。Ballantyne等[16]报道辛伐他汀联用依折麦布可明显降低LDL-C,其疗效相当于单用高剂量辛伐他汀。联合降脂不仅降低TC的合成、抑制TC的吸收,加快LDL-C分解和清除,快速达到降脂的目的,还可以减轻血管内皮功能损伤,提高血管斑块稳定性,抑制引起动脉粥样硬化的炎症反应。国内动物实验发现依折麦布在大鼠中通过激活AMPK/Nrf2/TXNIP途径来降低氧化应激及神经炎症反应,指出依折麦布可能是缺血性卒中患者的潜在治疗方法[17]。近年来在冠心病研究中发现,依折麦布联合他汀可用于冠状动脉粥样硬化斑块的稳定和预防[18]。此外,已有研究证实,近期发生过动脉粥样硬化性血管意外的患者,联合降脂可以明显降低LDL-C水平,显著降低卒中的风险[19-20]。近期患有脑梗死疾病的患者,瑞舒伐他汀联合依折麦布治疗的疗效优于单用瑞舒伐他汀,显著降低LDL-C[21]。本研究发现观察组患者LDL-C降低,优于对照组,与国内外报道相一致。在临床预后方面,谭忠兵等[22]发现,联合依折麦布后,急性脑梗死患者的神经功能也好于单独的他汀类药物治疗。本研究结果显示,观察组神经功能在治疗后比对照组提高,其自理能力及生活质量有所提高,与谭忠兵等[22]报道一致。在安全性上,国内罗昕等[23]也曾报道依折麦布联用他汀在改善脑梗死患者神经功能的同时,不会增加患者的不良反应。也有研究指出,他汀类药物联合依折麦布治疗ASCVD其3年结局并不劣于高强度他汀类药物单药治疗,LDL-C低于1.8 mmol/L的患者比例更高,不良反应发生率较低[24]。本研究结果显示,观察组治疗后的神经功能改善较对照组明显,且观察组与对照组不良反应发生率无显著性差异,与罗昕等[23]报道类似。同时,最新发布的2023年血脂管理指南也指出联合使用降脂药物是治疗血脂异常的常见策略。治疗过程中应定期监测疗效和副作用,并根据情况调整治疗计划,以确保长期达到治疗目标[25]。因此,在脑卒中高危人群及LDL-C未达标人群中,依折麦布联用他汀类药物可以显著降低LDL-C,提高LDL-C的达标率,改善神经功能。
本研究创新点是在基药集采下,依折麦布片联用阿托伐他汀钙片治疗ACI,通过减少TC及TG的吸收、强化降低LDL-C、升高HDL-C,来抑制颈动脉粥样硬化斑块的发展、稳定颈动脉粥样硬化斑块,减少神经功能恶化的发生,以达到降低致残率、减少复发率的目的。本项研究旨在探讨血脂异常和LDL-C控制不佳及缺血性脑卒中再发的关系,通过结合依折麦布片和阿托伐他汀钙片各自的作用机制,并利用二者的协同效应,制定更安全有效的预防和治疗方案。本研究的局限在于样本量较小和随访期较短。未来需要通过扩大多中心研究和延长随访期来进一步验证结果。
因此,依折麦布片与阿托伐他汀钙片联合治疗动脉粥样硬化性脑梗死,可以实现良好的降脂效果,有效降低TC、LDL-C、TG水平,提高LDL-C达标率,有助于改善神经功能,降低致残风险,尤其对脑卒中高危人群及LDL-C未达标人群。
参考文献
[1]中华医学会神经病学分会,中华医学会神经病学分会脑血管病学组.中国急性缺血性脑卒中诊治指南2018[J].中华神经科杂志,2018,51(9):666-682.
[2] FERENCE B A,GINSBERG H N,GRAHAM I,et al.Low-density lipoproteins cause atherosclerotic cardiovascular disease.1.Evidence from genetic,epidemiologic,and clinical studies.A consensus statement from the European atherosclerosis society consensus panel[J].Eur Heart J,2017,38(32):2459-2472.
[3] YUAN H W,YANG Y N,CHEN H F,et al.Rise in low-density lipoprotein cholesterol during hospitalization is related with poor outcome at discharge in patients with acute ischemic stroke[J].Cerebrovasc Dis,2020,49(1):88-96.
[4] RIDKER P M,MORA S,ROSE L,et al.Percent reduction in LDL cholesterol following high-intensity statin therapy:potential implications for guidelines and for the prescription of emerging lipid-lowering agents[J].Eur Heart J,2016,37(17):1373-1379.
[5] BANGALORE S,FAYYAD R,KASTELEIN J J,et al.2013 Cholesterol guidelines revisited:percent LDL cholesterol reduction or attained LDL cholesterol level or both for prognosis?[J].Am J Med,2016,129(4):384-391.
[6] SU X T,WANG L,MA S M,et al.Mechanisms of acupuncture in the regulation of oxidative stress in treating ischemic stroke[J].Oxid Med Cell Longev,2020:7875396.
[7] MAIDA C D,NORRITO R L,DAIDONE M,et al.
Neuroinflammatory mechanisms in ischemic stroke:focus on cardioembolic stroke,background,and therapeutic approaches[J].Int J Mol Sci,2020,21(18):6454.
[8] WANG Y C,HSIEH T C,CHOU C L,et al.Risks of adverse events following coprescription of statins and calcium channel blockers:a nationwide population-based study[J/OL].Medicine(Baltimore),2016,95(2):e2487[2024-05-16].https://pubmed.ncbi.nlm.nih.gov/26765458/.DOI: 10.1097/MD.0000000000002487.
[9] WHITEHORN J,NGUYEN C V V,KHANH L P,et al.
Lovastatin for the treatment of adult patients with dengue:a randomized,double-blind,placebo-controlled trial[J].Clin Infect Dis,2016,62(4):468-476.
[10] BYRNE P,DEMASI C,JONES M,et al.Evaluating the association between low-density lipoprotein cholesterol reduction and relative and absolute effects of statin treatment:a systematic review and meta-analysis[J].JAMA Intern Med,2022,182(5):474-481.
[11] SHIN J,CHUNG J W,JANG H S,et al.Achieved low-density lipoprotein cholesterol level and stroke risk:a meta-analysis of 23 randomised trials[J].Eur J Prev Cardiol,2021,28(8):905-916.
[12] AMARENCO P,KIM J S,LABREUCHE J,et al.Treat stroke to target trial design:first trial comparing two LDL targets in patients with atherothrombotic strokes[J].Eur Stroke J,2019,4(3):271-280.
[13] LEE M,CHENG C Y,WU Y L,et al.Association between intensity of low-density lipoprotein cholesterol reduction with statin-based therapies and secondary stroke prevention:a meta-analysis of randomized clinical trials[J].JAMA Neurol,2022,79(4):349-358.
[14] AMARENCO P,HOBEANU C,LABREUCHE J,et al.Carotid atherosclerosis evolution when targeting a low-density lipoprotein cholesterol concentrationlt;70 mg/dL after an ischemic stroke of atherosclerotic origin[J].Circulation,2020,142(8):748-757.
[15] KIM K J,KIM S H,YOON Y W,et al.Effect of fixed-dose combinations of Ezetimibe plus Rosuvastatin in patients with primary hypercholesterolemia:MRS-ROZE(multicenter randomized study of Rosuvastatin and Ezetimibe)[J].Cardiovasc Ther,2016,34(5):371-382.
[16] BALLANTYNE C M,ABATE N,YUAN Z,et al.Dose-comparison study of the combination of Ezetimibe and Simvastatin(Vytorin)versus Atorvastatin in patients with hypercholesterolemia:the Vytorin Versus Atorvastatin(VYVA)study[J].Am Heart J,2005,149(3):464-473.
[17] YU J,WANG W N,MATEI N,et al.Ezetimibe attenuates oxidative stress and neuroinflammation via the AMPK/Nrf2/TXNIP pathway after MCAO in rats[J].Oxid Med Cell Longev,2020,2020:1-14.
[18] FUJISUE K,YAMANAGA K,NAGAMATSU S,et al.Effects of statin plus Ezetimibe on coronary plaques in acute coronary syndrome patients with diabetes mellitus:sub-analysis of PRECISE-IVUS trial[J].J Atheroscler Thromb,2021,28(2):181-193.
[19] BOHULA E A,WIVIOTT S D,GIUGLIANO R P,et al.
Prevention of stroke with the addition of Ezetimibe to statin therapy in patients with acute coronary syndrome in IMPROVE-IT(improved reduction of outcomes:Vytorin efficacy international trial)[J].Circulation,2017,136(25):2440-2450.
[20] BROOKS D C,SCHINDLER J L.Management of hyperlipidemia after stroke[J].Curr Treat Options Cardiovasc Med,2019,21(12):93.
[21] HONG K S,BANG O Y,PARK J H,et al.Moderate-intensity Rosuvastatin plus Ezetimibe versus high-intensity Rosuvastatin for target low-density lipoprotein cholesterol goal achievement in patients with recent ischemic stroke:a randomized controlled trial[J].J Stroke,2023,25(2):242-250.
[22]谭忠兵,夏乐,管义祥,等.依折麦布联合洛伐他汀对急性脑梗死的疗效及颈动脉内膜中层厚度等的影响[J].西北药学杂志,2021,36(1):135-139.
[23]罗昕,欧阳歆怡,翁燕红,等.不同调脂方案治疗他汀不耐受动脉粥样硬化性脑梗死患者的临床疗效[J].医学研究与战创伤救治,2023,36(5):473-478.
[24] KIM B K,HONG S J,LEE Y J,et al.Long-term efficacy and safety of moderate-intensity statin with Ezetimibe combination therapy versus high-intensity statin monotherapy in patients with atherosclerotic cardiovascular disease(RACING):a randomised,open-label,non-inferiority trial[J].Lancet,2022,400(10349):380-390.
[25]中国血脂管理指南修订联合专家委员会,李建军,赵水平,等.中国血脂管理指南(2023年)[J].中国循环杂志,2023,38(3):237-271.
(收稿日期:2024-06-05) (本文编辑:田婧)
