单中心经导管主动脉瓣置换术的疗效及安全性分析
2024-11-29苏亚民耿海华李晓飞范勐慷陆晓晨黄荣曹翔刘琨薛群尤庆生于小红盛红专
[摘" "要]" "目的:回顾南通大学附属医院心脏瓣膜中心经导管主动脉瓣置换术(transcatheter aortic valve replacement, TAVR)的临床数据,总结手术相关经验。方法:2020年10月—2023年6月在本中心接受TAVR手术患者28例,收集患者的病史、实验室检验以及辅助检查等临床资料,对手术成功率、并发症、院内结果以及6个月随访结果进行回顾性分析。结果:28例患者中男女各14例,平均年龄(75.54±6.08)岁,其中重度主动脉瓣狭窄22例,重度单纯主动脉瓣反流6例,美国胸外科医师协会平均积分为(4.05±3.48)分,手术成功率为96.43%,因Ⅲ度房室传导阻滞植入永久起搏器5例(17.86%);术中中度瓣周漏3例(10.71%),其中采用球囊后扩张1例,采用“瓣中瓣”技术2例使瓣膜反流显著减轻;发生瓣膜跳脱1例(3.57%),植入第2个瓣膜使其锚定于升主动脉;术中心包填塞3例(10.71%),2例予心包置管、鱼精蛋白中和肝素后出血终止;另1侧发生瓣环撕脱转行开胸手术后死亡;半年随访期间1例患者因重度贫血再次入院,所有患者生活质量显著提高。结论:TAVR治疗重度主动脉瓣狭窄或反流具有良好的有效性和安全性。
[关键词]" "经导管主动脉瓣置换术;主动脉瓣狭窄;主动脉瓣反流;手术安全性;手术有效性
[中图分类号]" "R541.4" " " " " " " "[文献标志码]" "A" " " " " " " "[文章编号]" "1674-7887(2024)02-0117-05
Analysis of the efficacy and safety regarding transcatheter aortic valve replacement from
a single clinical center*
SU Yamin1**, GENG Haihua1, LI Xiaofei1, FAN Mengkang1, LU Xiaochen1, HUANG Rong1, CAO Xiang2, LIU Kun2, XUE Qun2, YOU Qingsheng2, YU Xiaohong1, SHENG Hongzhuan1***" " " " (1Department of Cardiology, 2Department of Cardiac Surgery, the Affiliated Hospital of Nantong University, Jiangsu 226001)
[Abstract]" "Objective: To sum up the procedural experience through analyzing the clinical data regarding transcatheter aortic valve replacement(TAVR) in our center. Methods: From October 2020 to June 2023, 28 patients were treated by TAVR procedure in the Valvular Heart Disease Center, the Affiliated Hospital of Nantong University. The clinical data such as medical history, laboratory tests and auxiliary examinations were collected. The procedural success rate, procedural complications, in-hospital results and 6-month follow-up results were retrospectively analyzed. Results: The mean age of the 28 patients with 14 females and 14 males respectively was (75.54±6.08) years, including 22 patients with severe aortic stenosis and 6 patients with pure severe aortic regurgitation. The Society of Thoracic Surgeons average score was 4.05±3.48, and the procedural success rate was 96.43%. There were 5 patients(17.86%) implanted permanent pacemaker implantation due to degree Ⅲ atrioventricular block. Moderate para-valvular leakage occurred in 3 patients(10.71%) during the operation, in which 1 case underwent post-balloon dilation and 2 cases underwent \"valve-in-valve\" technique to significantly reduce valve regurgitation. 1 patient(3.57%) suffered from the valve jumping, and the second valve was implanted to fix the first one at the ascending aorta. Pericardial tamponade occurred in 3 patients(10.71%), in which 2 patients survived because that the hemorrhage was terminated after pericardial catheterization and protamine neutralization of heparin, while the third one left suffered from the aorticannulus avulsion and died after conversion to thoracotomy. During the 6 months follow-up, 1 patient was re-hospitalized due to the severe anemia. The life quality of all patients was significantly improved. Conclusion: TAVR processes favourable efficacy and safety in the treatment of severe aortic valve stenosis or regurgitation.
[Key words]" "transcatheter aortic valve replacement; aortic stenosis; aortic regurgitation; procedural safety; procedural efficacy
随着人口老龄化进程的加剧,主动脉瓣疾病患者越来越多。既往外科主动脉瓣置换术(surgical aortic valve replacement, SAVR)是根治严重主动脉瓣疾病患者的唯一选择。2002年,A.CRIBIER等[1]完成首例人体经导管主动脉瓣置换术(transcatheter aortic valve replacement, TAVR),开启了治疗严重主动脉瓣狭窄(aortic stenosis, AS)的新篇章。最初,TAVR主要应用于不适合SAVR治疗的高危严重AS患者[2],随着20余年来器械的更新迭代及循证医学数据的积累,TAVR已成为老年严重AS患者的一线治疗方法[3]以及严重主动脉瓣反流(aortic regurgitation, AR)的新选择[4-5]。然而,TAVR技术难度大,并发症发生率相对较高,适时回顾本中心数据,分析TAVR手术的疗效及安全性,总结临床实践中的经验和不足,将有助于进一步提高TAVR手术的治疗效果。
1" "对象与方法
1.1" "研究对象" "2020年10月—2023年6月选择在南通大学附属医院心脏瓣膜中心行TAVR治疗的患者28例。重度AS的入选标准:(1)症状性重度AS;(2)平均跨瓣压差>40 mmHg;(3)有效瓣口面积<1.0 cm2;(4)瓣口前向最大血流速度≥4 m/s[3]。重度AR的入选标准:(1)临床症状明显;(2)术前超声心动图提示重度AR,缩流颈宽度≥6 mm,压差半降时间(pressure half time, PHT)<200 ms,有效反流口面积(effective regurgitant orifice area, EROA)≥30 mm2,反流量≥60 mL/次[3]。排除标准:(1)发热或合并未控制的感染性疾病;(2)合并肥厚型梗阻性心肌病;(3)左心室内血栓形成;(4)1个月内发生急性心肌梗死;(5)严重出血倾向,不能耐受抗血小板药物治疗;(6)多排螺旋CT血管造影(computed tomography angiography, CTA)显示主动脉根部结构不宜TAVR手术。所有入选患者均经过优化药物治疗,同时完善血常规、肝肾功能、凝血功能、超声心动图、CT等检查。所有患者术前均签署手术知情同意书。
1.2" "手术方法" "所有患者术前均行主动脉、冠状动脉及心脏多排螺旋CTA,评估患者的心脏、主动脉根部、冠状动脉、主动脉及股动脉等解剖情况,作为患者筛选、瓣膜型号选择及血管入路评估的主要依据。术中采用静脉复合麻醉,常规放置食管超声导管,Seldinger′s技术穿刺股动脉、股静脉,主入路股动脉预埋两枚交叉垂直的Proglide血管缝合器,猪尾导管经辅入路股动脉完成主动脉根部造影,如需冠脉保护则穿刺桡动脉,经桡动脉放置冠脉指引导管,预埋冠脉导丝及支架。X线透视下将临时起搏电极送至右室心尖部,Amplatz左冠导管辅助直头导丝跨越主动脉瓣,猪尾导管辅助下置换为塑形超硬导丝,沿超硬导丝送入瓣膜输送系统,如通过困难可予Snare圈套器辅助,快速起搏下(120~180次/min)释放瓣膜至工作区,造影确认瓣膜位置合适后完全释放瓣膜。术中肝素初始计量100 U/kg,手术每延长1 h追加肝素1 000 U,监测活化凝血时间,使其维持在250~350 s。术后常规口服阿司匹林(100 mg,1次/d)和P2Y12受体抑制物(氯吡格雷75 mg,1次/d)。根据病情给予他汀类、血管紧张素转换酶抑制剂、β受体阻滞剂、口服抗凝药、硝酸酯类等药物。
1.3" "研究终点及相关定义" "主要研究终点是手术成功率,根据瓣膜学术研究联盟(valve academic research consortium, VARC)-3[6]的标准,手术成功定义为患者离开手术室时无死亡,器械进入及输送成功,传输系统回收成功,人工瓣膜正确定位至合适的解剖位置,无需因器械、主要血管、入路或心脏结构并发症进行手术或介入干预。次要终点是记录患者心肌梗死和冠脉阻塞、急性脑卒中、中度以上瓣膜反流、永久起搏器植入、大出血、心包填塞等相关信息。完成患者TAVR术后6个月随访。
1.4" "统计学方法" "采用SPSS 27.0统计软件进行分析。计数资料采用频数和百分比(%)描述,连续变量以■±s表示。手术前后资料若符合正态分布,采用配对t检验,否则采用非参数检验,分类数据采用χ2检验。P<0.05表示差异有统计学意义。
2" "结" " " 果
2.1" "基线临床资料" "28例患者均为退行性主动脉瓣病变,男女各14例,年龄63~86岁,平均(75.54±6.08)岁,平均体质量(60.36±12.58) kg,平均身高(162.46±7.12) cm,其中重度AS 22例,重度单纯AR 6例。28例患者中既往高血压病史19例(67.86%),合并糖尿病6例(21.43%),冠状动脉粥样硬化性心脏病(以下简称冠心病)9例(32.14%),心房颤动7例(25.00%),4例(14.29%)为二叶式主动脉瓣。美国胸外科医师协会(Society of Thoracic Surgeons, STS)评分平均为(4.05±3.48)分;欧洲心血管手术危险评分(European System for Cardiac Operative Risk EvaluationⅡ, EuroSCOREⅡ)平均为(4.00±3.39)分;纽约心脏病学会(New York Heart Association, NYHA)心功能分级Ⅱ级5例(17.86%),Ⅲ级17例(60.71%),Ⅳ级6例(21.43%)。
2.2" "TAVR手术情况" "28例患者均经股动脉途径植入瓣膜,失败1例,手术成功率96.43%。28例患者共植入31枚人工瓣膜,选用国产自膨式瓣膜26例,包含启明VenusA瓣膜13枚,沛嘉TaurusOne瓣膜15枚,微创VitaFlow瓣膜1枚;选用球囊扩张式瓣膜2例,为科凯KOKAVAVLE瓣膜。28例患者选择23 mm瓣膜9例,24 mm瓣膜1例,26 mm瓣膜12例,29 mm瓣膜3例,31 mm瓣膜2例,32 mm瓣膜1例。冠脉保护2例;术中出现中度瓣周漏3例(10.71%),采用球囊后扩张1例,置入第2枚瓣膜(“瓣中瓣”技术)2例,瓣膜反流均显著减轻。1例(3.57%)患者瓣膜跳脱至升主动脉,置入第2枚瓣膜同时将滑脱瓣膜固定。5例患者(17.86%)出现Ⅲ度房室传导阻滞(术中1例,术后4例),均置入永久起搏器。出现心包填塞3例(10.71%),立即予心包置管、自体血液回输、鱼精蛋白中和肝素,2例抽出约300 mL血液后出血终止,考虑与心室内超硬导丝相关,1例诊断为主动脉瓣环撕裂,心包内出血量大,中转行开胸手术后死亡。
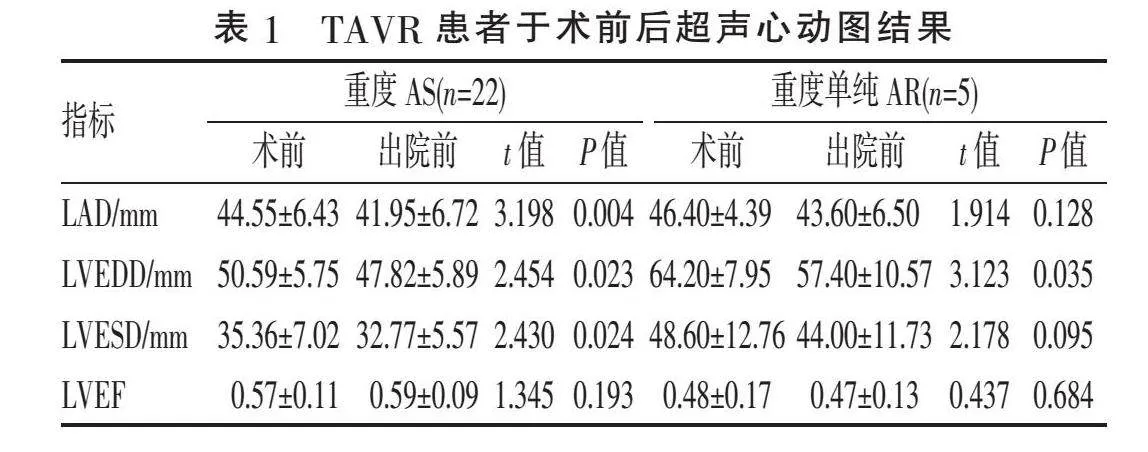
2.3" "院内及随访结果" "28例患者住院期间死亡1例,其余临床症状均明显改善。22例重度AS患者术毕即刻主动脉瓣跨瓣压差明显下降[(86.14±24.42) mmHg vs (14.91±17.31) mmHg, P<0.001],出院前经胸复查超声心动图,左心房直径(left atrial diameter, LAD)、左心室舒张末期内径(left ventricular end diastolic diameter, LVEDD)、左心室收缩末期内径(left ventricular end systolic diameter, LVESD)较术前明显减小(P<0.05),左心室射血分数(left ventricular ejection fraction, LVEF)较术前有增加趋势,但差异无统计学意义(P>0.05)。排除1例死亡,5例重度单纯AR患者术后AR降至轻度,出院前LVEDD较术前明显减小(P<0.05),LAD、LVESD呈减小趋势,但差异无统计学意义(P>0.05)。LVEF呈减少趋势,因反流明显减轻,患者心力衰竭症状明显改善,见表1。半年随访期间,1例患者因重度贫血再次入院,治疗后好转,所有患者心功能明显改善,生活质量显著提高。
3" "讨" " " 论
AS是全球最常见的瓣膜疾病之一,严重AS(主动脉瓣口面积<1.0 cm2)的发病率在75岁及以上人群中高达2%~4%[7]。内皮受损引发炎症反应和脂质浸润是AS发病的关键因素,一旦发病机制被激活,几乎所有患者的瓣叶将发生组织钙化,终末期导致严重的AS。钙化性瓣膜病与年龄、男性、血清低密度脂蛋白胆固醇、高血压、吸烟以及糖尿病等存在关联,二叶式主动脉瓣是AS常见的解剖危险因素。本中心TAVR患者中4例为二叶式主动脉瓣,大部分患者有高血压病史,往往合并冠心病、糖尿病、血脂异常等代谢性疾病,提示控制心血管危险因素,改善生活方式,有助于预防和延缓主动脉瓣疾病进展。
TAVR首先被应用于不适合SAVR治疗的高危AS患者。此后,随机对照研究[8-9]证明在手术风险较低的症状性AS患者中,TAVR的疗效亦不劣于SAVR。目前指南[10]推荐,年龄>80岁的重度AS患者,TAVR优于SAVR;对年龄65~80岁症状性严重AS患者,不管外科手术风险级别,TAVR仍被认可为Ⅰ类推荐。本中心TAVR手术患者平均年龄为(75.54±6.08)岁,STS平均分数为(4.05±3.48)分,手术成功率96.43%,半年随访显示TAVR手术效果良好,对于年龄<65岁、STS分数<8分的年轻非高危重度AS患者,仍优先推荐SAVR手术,合理选择治疗策略将为AS患者带来更优的临床预后。
中重度AR人群患病率约0.5%[11],其中部分患者因禁忌或高风险而丧失外科手术机会,仅接受抗心力衰竭药物治疗。TAVR有望降低该类患者的死亡率,提高其生活质量。然而,中重度AR患者往往主动脉瓣环增大,缺乏钙化锚定点,为了增加径向支撑力,瓣膜往往需oversize 15%~20%,这增加了瓣膜脱位、瓣环破裂的风险,本中心1例死亡患者即为重度单纯AR患者,瓣膜释放时发生瓣环破裂、心包填塞。因此,建议尽可能选择带有裙边的TAVR瓣膜,以增加瓣膜与主动脉瓣环锚定区的摩擦力,同时应在窦管交界区及升主动脉寻找额外锚定平面。目前,新一代设备,尤其是带有定位件的器械,提高了TAVR治疗AR的安全性和可行性[12-13]。
TAVR围术期并发症风险较高,须谨慎对待。心包填塞是TAVR术中常见的灾难性事件之一,常与临时起搏电极导致右心穿孔、加硬导丝穿破左心室、主动脉瓣环及根部破裂等相关。本中心发生心包填塞3例,其中2例考虑与心室壁薄及加硬导丝张力过大相关,经心包置管、鱼精蛋白中和肝素及自体血液回输等治疗后出血停止,预后良好;另1例患者为瓣环破裂,出血量大,中转行开胸手术后死亡。TAVR术中一旦发生循环崩溃,应立即行心脏超声检查,发现心包填塞后仔细分析原因,尽快心包置管引流,予鱼精蛋白中和肝素及自体血液回输,小穿孔多可缓解,如出血量大,循环血流动力学不稳定,建议先予循环支持,再行外科开胸手术。冠脉阻塞极其凶险,病死率极高,预判及预处理最为重要,术前须充分评估。对冠脉开口下缘至瓣环平面的垂直距离<10 mm、瓣叶长度gt;冠脉开口水平患者行冠状动脉保护(预埋导丝、球囊或支架,必要时放置“烟囱”支架)[14]。冠脉阻塞风险高的患者应适度减小瓣膜直径,允许一定程度的瓣周漏、跨瓣压差。中重度瓣周漏对患者远期预后存在不利影响,术前应仔细评估主动脉根部解剖,包括主动脉瓣环形态、钙化程度及分布等。本中心3例患者出现中度瓣周漏,1例瓣膜未完全膨胀,采用球囊后扩张,2例瓣膜裙边进入心腔,血液通过支架网孔反流,采用“瓣中瓣”技术植入第2枚瓣膜后反流显著减轻。此外,瓣膜定位不佳可予抓捕器牵拉调整,处理效果不佳的中重度瓣周漏可选择外科手术[15-16]。房室传导阻滞多发生在TAVR术后1周内,预防措施包括避免瓣膜支架植入太深(>6 mm),避免选择直径过大的瓣膜,对已存在右束支传导阻滞的患者选用球囊扩张瓣膜等[17-18],新一代球囊扩张瓣膜起搏器植入比例明显降低[19]。总之,“防患于未然”仍是TAVR并发症防治最重要的策略,术者须谨慎对待,术前精细评估,周详规划,做好并发症处理的准备。
TAVR彻底改变了主动脉瓣疾病患者的治疗策略及管理,本中心数据显示了TAVR手术良好的安全性和有效性。及时分析手术结果,总结经验教训有助于促进技术进步,减少并发症,提高TAVR治疗效果。
[参考文献]
[1]" "CRIBIER A, ELTCHANINOFF H, BASH A, et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description[J]. Circulation, 2002, 106(24):3006-3008.
[2]" "NISHIMURA R A, OTTO C M, BONOW R O, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines[J]. Circulation, 2014, 129(23):2440-2492.
[3]" "VAHANIAN A, BEYERSDORF F, PRAZ F, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease[J]. Eur Heart J, 2022, 43(7):561-632.
[4]" "ZHU D, HU J, MENG W, et al. Successful transcatheter aortic valve implantation for pure aortic regurgitation using a new second generation self-expanding J-Valve(TM) system-the first in-man implantation[J]. Heart Lung Circ, 2015, 24(4):411-414.
[5]" "WEI L, LIU H, ZHU L M, et al. A new transcatheter aortic valve replacement system for predominant aortic regurgitation implantation of the J-valve and early outcome[J]. JACC Cardiovasc Interv, 2015, 8(14):1831-1841.
[6]" "VARC-3 WRITING COMMITTEE, G?魪N?魪REUX P, PIAZZA N, et al. Valve Academic Research Consortium 3: Updated endpoint definitions for aortic valve clinical research[J]. J Am Coll Cardiol, 2021, 77(21):2717-2746.
[7]" "NKOMO V T, GARDIN J M, SKELTON T N, et al. Burden of valvular heart diseases: a population-based study[J]. Lancet, 2006, 368(9540):1005-1011.
[8]" "MACK M J, LEON M B, THOURANI V H, et al. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients[J]. N Engl J Med, 2019, 380(18):1695-1705.
[9]" "POPMA J J, DEEB G M, YAKUBOV S J, et al. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients[J]. N Engl J Med, 2019, 380(18):1706-1715.
[10]" "OTTO C M, NISHIMURA R A, BONOW R O, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: executive summary: a report of the American college of cardiology/american heart association joint committee on clinical practice guidelines[J]. Circulation, 2021, 143(5):e35-e71.
[11]" "MAURER G. Aortic regurgitation[J]. Heart, 2006, 92(7):994-1000.
[12]" "SILASCHI M, CONRADI L, WENDLER O, et al. The JUPITER registry: one-year outcomes of transapical aortic valve implantation using a second generation transcatheter heart valve for aortic regurgitation[J]. Catheter Cardiovasc Interv, 2018, 91(7):1345-1351.
[13]" "LIU X P, TANG Y, LUO F L, et al. Transapical implantation of a self-expandable aortic valve prosthesis utilizing a novel designed positioning element[J]. Catheter Cardiovasc Interv, 2017, 89(1):E30-E37.
[14]" "FETAHOVIC T, HAYMAN S, COX S, et al. The prophylactic chimney snorkel technique for the prevention of acute coronary occlusion in high risk for coronary obstruction transcatheter aortic valve replacement/implantation cases[J]. Heart Lung Circ, 2019, 28(10):e126-e130.
[15]" "SINNING J M, VASA-NICOTERA M, CHIN D, et al. Evaluation and management of paravalvular aortic regurgitation after transcatheter aortic valve replacement[J]. J Am Coll Cardiol, 2013, 62(1):11-20.
[16]" "DVIR D, BARBASH I M, BEN-DOR I, et al. Paravalvular regurgitation after transcatheter aortic valve replacement: diagnosis, clinical outcome, preventive and therapeutic strategies[J]. Cardiovasc Revasc Med, 2013, 14(3):174-181.
[17]" "ROD?魪S-CABAU J, ELLENBOGEN K A, KRAHN A D, et al. Management of conduction disturbances associated with transcatheter aortic valve replacement: JACC Scientific Expert Panel[J]. J Am Coll Cardiol, 2019, 74(8):1086-1106.
[18]" "JILAIHAWI H, ZHAO Z, DU R, et al. Minimizing permanent pacemaker following repositionable self-expanding transcatheter aortic valve replacement[J]. JACC Cardiovasc Interv, 2019, 12(18):1796-1807.
[19]" "MAHAJAN S, GUPTA R, MALIK A H, et al. Predictors of permanent pacemaker insertion after TAVR: a systematic review and updated meta-analysis[J]. J Cardiovasc Electrophysiol, 2021, 32(5):1411-1420.
[收稿日期] 2023-11-24