Epidemiological characteristics of hyperuricemia in metabolic syndrome and its different components in the physical examination population
2024-01-19WUXuanxiaBUJuanZHANGYanminYeledanMahanZHOUMingmingMAYingyingLUHuanhuanZHANGXiaolingZHOULing
WU Xuan-xia, BU Juan, ZHANG Yan-min, Yeledan Mahan, ZHOU Ming-ming, MA Yingying, LU Huan-huan, ZHANG Xiao-ling, ZHOU Ling✉
1. Graduate School of Xinjiang Medical University, Urumqi 830011, China
2. Medical Research and Transformation Center, People’s Hospital of Xinjiang Uygur Autonomous Region, Urumqi 830001, China
3. Scientific Research and Education Center, People’s Hospital of Xinjiang Uygur Autonomous Region, Urumqi 830001, China
4. Health Management Center, People’s Hospital of Xinjiang Uygur Autonomous Region, Urumqi 830001, China
Keywords:
ABSTRACT Objective: To explore the epidemiological characteristics of hyperuricemia (HUA) in the metabolic syndrome (MS) and its different components in the physical examination population.Methods: Subjects who underwent medical check-ups at a hospital health management center from June 2021 to March 2023 were included in the study.To analyze the prevalence of HUA in MS and its different components, further, stratify the study population by gender and assess the serum uric acid (SUA) levels and prevalence of HUA in people with different numbers of MS components and the combination of MS components with the highest prevalence of HUA in both sexes.Logistic regression was used to analyze the risk of HUA in people with different numbers of MS components.Result: A total of 66,520 individuals were enrolled in the study.SUA levels (t= -82.947, P<0.001) and HUA prevalence (χ2 = 3421.632, P<0.001) were significantly higher in the MS group than in the Non-MS group.SUA levels and prevalence of HUA were significantly higher in abdominal obesity, hypertension, decreased HDL-C and evaluated TG than in normal subjects (P<0.001), while there were gender differences in SUA levels and HUA prevalence in diabetic patients, with significantly lower SUA levels and HUA prevalence in men with diabetes than in those with normal blood glucose, an opposite result in women.SUA levels and HUA prevalence gradually increased with the increasing number of MS components in women, whereas in men, such a trend was only observed in MS1-MS4.The combination of MS components with the highest prevalence of HUA was abdominal obesity+ hypertension + decreased HDL-C + evaluated TG (54.35%) in men and abdominal obesity+ hypertension + diabetes + decreased HDL-C + evaluated TG (41.46%) in women.Logistic regression analysis showed that after adjusting for gender, age and ethnicity, the risk of HUA increased with the number of MS components in women, while in men, the risk of HUA increased continuously from MS1-MS4.Further adjustment for BMI, elevated TC, elevated LDL-C, and coronary artery disease, the results remained consistent.Conclusion: MS and its components are risk factors for HUA in the physical examination population, with different combinations of MS components having different correlations with HUA, and the risk of developing HUA correlates with the number of abnormal MS components.
1.Introduction
Hyperuricemia is an increase in serum uric acid levels due to abnormalities in purine metabolism.In addition to being the pathological basis of gout, HUA is also an independent risk factor for chronic kidney disease, hypertension, coronary heart disease,and metabolic syndrome[1,2].Data from the National Health and Nutrition Examination Survey (NHANES) show that 20% of American adults suffer from HUA[3].In China, the prevalence of HUA among adults is 17.7%[4], and in some coastal cities, it has even exceeded 30%[5].With the rapid development of China’s economy,westernized dietary habits and an aging population, the prevalence of HUA is still on the rise, so the prevention and treatment of HUA has become a public health issue of great urgency.
Metabolic syndrome is a cluster of metabolic disorders including excessive accumulation of abdominal fat, hypertension,hyperglycemia, lowered high-density lipoprotein and hypertriglyceridemia[6], and the interactions between these MS components make the pathogenesis and pathways of MS complex.The epidemiological findings in recent years have shown that all components of MS, including obesity, hypertension, diabetes and dyslipidemia, are strongly associated with HUA[7-8].A stronger association of MS with HUA has been demonstrated, however,the association of MS and its components with HUA will also be variable due to factors such as age, gender, and ethnicity[9-12].Moreover, with the numerous numbers, diverse combinations and complex interactions of MS components, different combinations of MS components may result in different pathophysiological mechanisms, health effects and therapeutic choices, and thus the MS investigation as a whole may obscure the relationship assessment and risk prediction between MS and HUA.Currently, the reports on the relationship between MS components and their different combinations with the progression of HUA are limited and need to be further explored.Therefore, this study is designed to investigate and analyze the prevalence of HUA in populations with different combinations of MS components, and to explore the association between MS and HUA in-depth, to provide a theoretical basis for the prevention and treatment of HUA.
2.Materials and methods
2.1 Study subject
The subjects of this study were medical check-ups performed from June 2021 to March 2023 at a hospital health management center.Of these, 13,535 had repeated medical check-ups during that period,and we only included the results of their first medical check-up in this study.Excluding minors, pregnant women, severely impaired liver and renal function, blood biochemistry tests and physical examination data were missing, a total of 66,520 people were finally enrolled in this study, as shown in Figure 1.All study participants signed an informed consent form.This study was approved by the Ethics Committee of People’s Hospital of Xinjiang Uygur Autonomous Region (approval number: KY2023011801).

Fig 1 Flowchart for the selection of study subjects
2.2 Research content and methods
Standardized information collection was carried out by professionally trained medical staff, with general information including gender, age, ethnicity and past history (hypertension,diabetes mellitus, coronary heart disease).Physical examination included measurement of height, weight, waist circumference and blood pressure, with body mass index (BMI) = weight (kg)/height(m)2.All subjects were fasted after 22:00 on the day before blood collection, and blood was collected from the median vein of the elbow on the following day.Total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol(LDL-C), low-density lipoprotein cholesterol (LDL-C) and serum uric acid (SUA) were measured using an automatic biochemical analyzer.
2.3 Diagnostic criteria and related definitions
Diagnostic criteria for HUA: male SUA 420 μmol/L, female SUA 360 μmol/L[13].According to the Chinese Guidelines for the Prevention and Control of Type 2 Diabetes(2017 edition): (1)abdominal obesity: waist circumference 90cm in men and 85cm in women; (2) hypertension: systolic blood pressure 135 mmHg and/or diastolic blood pressure 85mmHg and/or previous diagnosis of hypertension; (3) diabetes: fasting blood glucose level 6.1mmol/L and/or previous diagnosis of diabetes; (4) decreased HDL-C: HDL-C<1.04 mmol/L; (5) elevated TG: TG 1.7 mmol/L.The diagnosis of MS was made if 3 of the above items were met[14].TC 6.22 mmol/L was defined as elevated TC and LDL-C 4.14 mmol/L was defined as elevated LDL-C[15].
2.4 Definition of the number of metabolic syndrome components
0 abnormality in the MS diagnostic criteria is defined as MS0;1 abnormality in the MS diagnostic criteria is defined as MS1; 2 abnormalities in the MS diagnostic criteria are defined as MS2; 3 abnormalities in the MS diagnostic criteria are defined as MS3; 4 abnormalities in the MS diagnostic criteria are defined as MS4; 5 abnormalities in the MS diagnostic criteria are defined as MS5.
2.5 Statistical analysis
SPSS 26.0 was used for data processing and analysis.Normally distributed continuous variables were expressed as mean ± standard deviation and count data were expressed as number of cases and percentage.One-way analysis of variance (ANOVA) was used to compare the differences in continuous variables.When comparing categorical data, the chi-square test was used.Logistic regression was used to analyze the risk factors for hyperuricemia.P<0.05 was considered statistically significant.
3.Result
3.1 Baseline characteristics of the study population
A total of 66,520 study subjects were included in this study,including 37,712 (56.59%) males and 28,808 (43.31%) females, with a mean age of (43.58±13.70) years.Age composition of the study population: the main age groups were 30~39 years (28.85%), 40~49 years (21.18%), and 50~59 years (20.66%).Ethnic composition:The study population is characterized by a multi-ethnic composition,with Han accounting for 77.35%, Uygur 11.81%, Hui 5.31%, Kazak 2.50%, and Mongolian 0.91%, and the remaining 31 ethnic groups were combined as other due to a smaller sample size, accounting for 2.13%.The mean BMI of the study population was 25.15, which was an overall overweight status.According to the blood biochemistry results, the incidence of elevated TC decreased HDL-C, elevated TG and elevated LDL-C was 9.17% 20.86%, 34.60% and 8.76%respectively.Comorbidity profile: In this population, 44.18%suffered from abdominal obesity, 43.06% from hypertension, 9.92%from diabetes, and 5.54% from coronary artery disease, while the prevalence of MS and HUA were both 25.47%.For details, refer to Table 1.
3.2 Serum uric acid levels and prevalence of hyperuricemia in populations with the metabolic syndrome and its different components
The prevalence of HUA and SUA levels were significantly higher in the MS group than in the non-MS group, both in the overall, males and females.MS consisted of five components: abdominal obesity,hypertension, diabetes, decreased HDL-C and elevated TG.Overall,SUA levels and prevalence of HUA were significantly higher in the abdominal obesity, hypertension, diabetes, decreased HDL-C and elevated TG groups than in the controls.Further stratified by gender,the abdominal obesity, hypertension, decreased HDL-C and elevated TG groups tended to have higher SUA levels and prevalence of HUA compared to the control group, both in males and females.It was also found that across genders, men with diabetes had lower SUA levels and HUA prevalence compared to those with normal blood glucose levels, while the opposite was found in women.The results are shown in Table 2 and Table 3.
3.3 Serum uric acid levels and prevalence of hyperuricemia in populations with different numbers of metabolic syndrome components
Overall, from MS1 to MS4, SUA levels and the prevalence of HUA increased gradually with the increasing number of MS components.At MS5, SUA levels and HUA prevalence decreased (390.02 ± 96.10 μmol/L; 37.90%).When analyzed by gender subgroups, SUA levelswere higher in males than in females in the corresponding number of MS components, and the prevalence of HUA was higher than in females at MS1-MS4 and lower than in females at MS5 (37.40%vs.41.46%).In both males and females, from MS0 to MS4, SUA levels and the prevalence of HUA increased with increasing number of components, whereas at MS5, SUA levels and HUA prevalence decreased in males (396.41±95.34 μmol/L; 37.40%), while females still showed an increasing trend (344.89±89.49 μmol/L; 41.46%), as detailed in Figure 2-3.
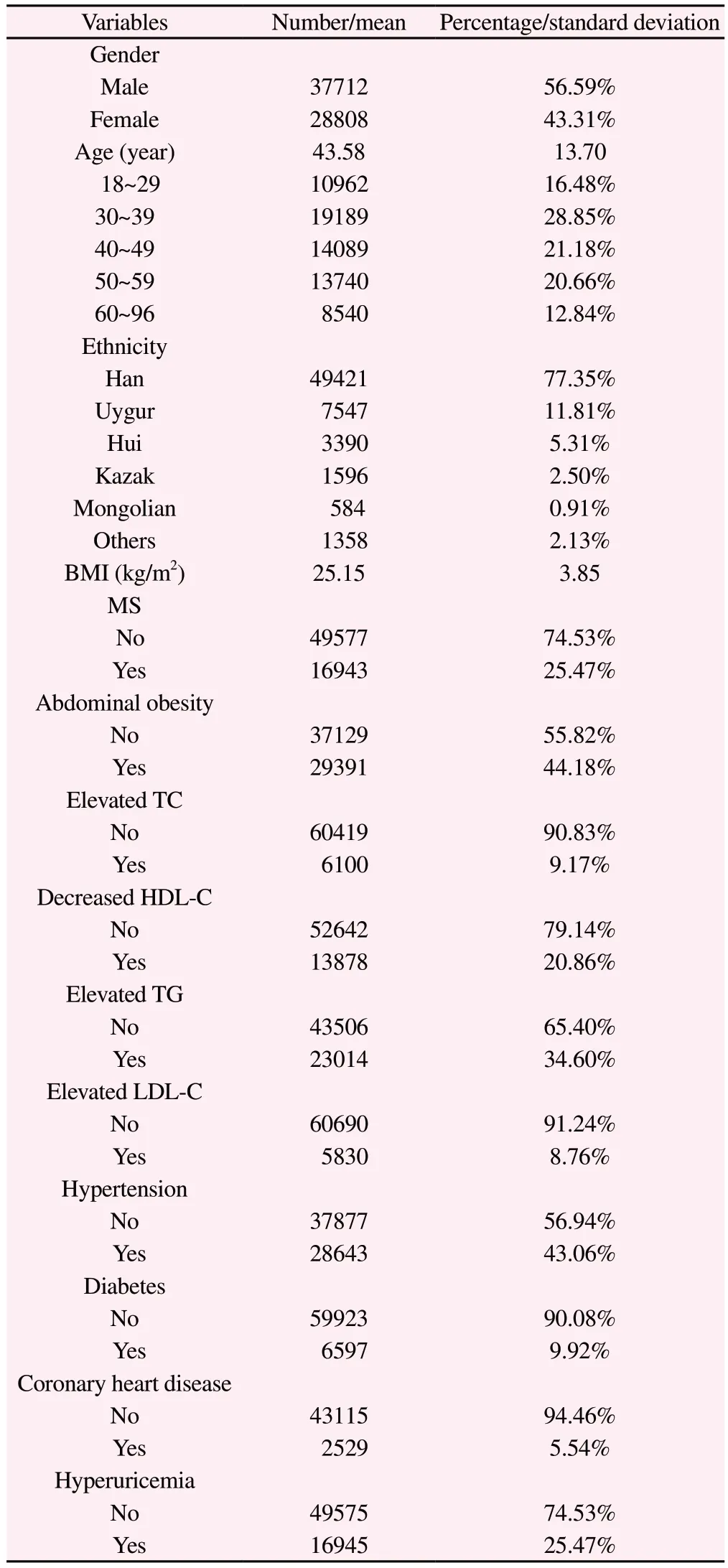
Tab 1 Baseline characterization of the study population
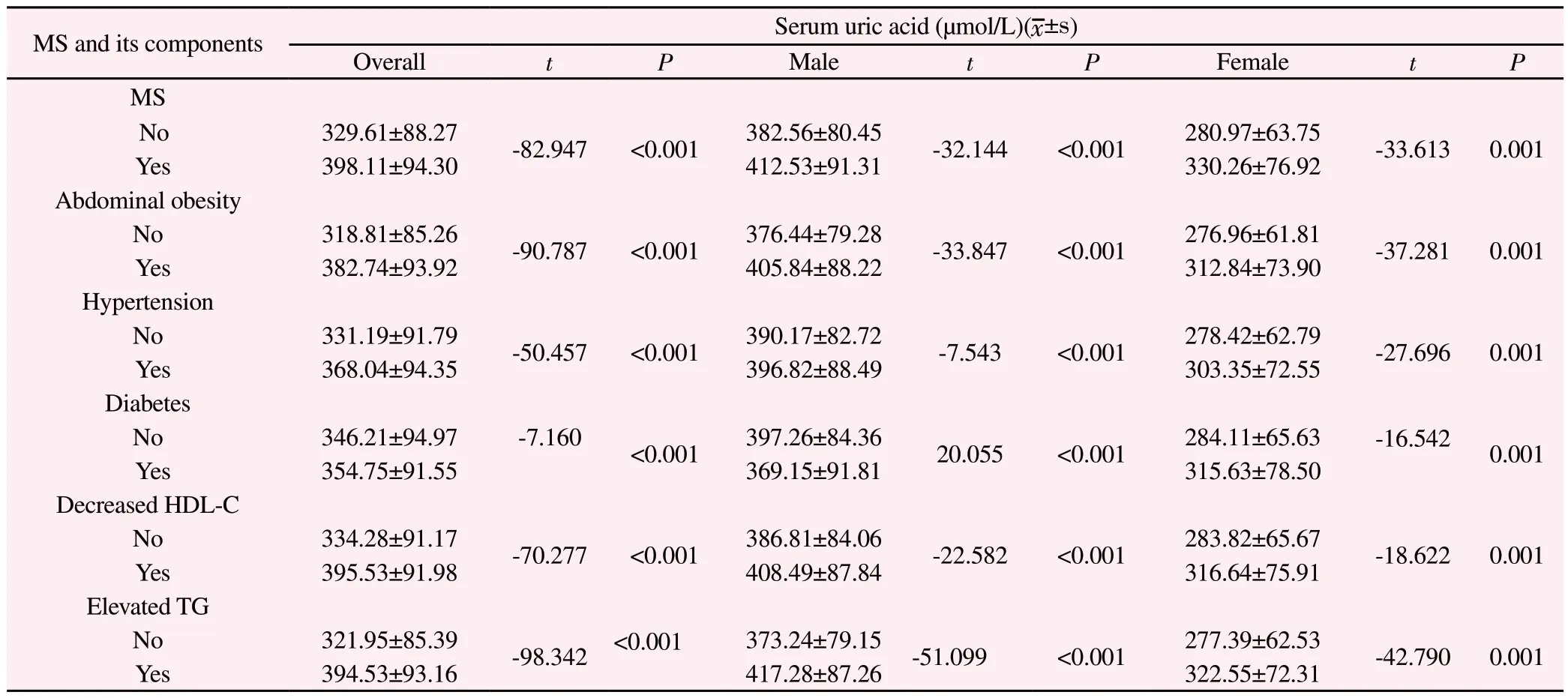
Tab 2 Serum uric acid levels in people with metabolic syndrome and its different components

Tab 3 Prevalence of hyperuricemia in people with metabolic syndrome and its different components
3.4 Prevalence of hyperuricemia in population with different combinations of metabolic syndrome components
To further investigate the comprehensive effects of MS components on HUA, the five components of MS were arbitrarily combined in this study, and the five MS component combinations with the highest prevalence of HUA were analyzed.Overall, the combination of abdominal obesity + hypertension + reduced HDL-C + evaluated TG had the highest prevalence of HUA at 53.11%.In males, this combination had the highest prevalence of 54.35%, while in females,the combination of abdominal obesity + hypertension + diabetes +reduced HDL-C + elevated TG had the highest prevalence of HUA at 41.46%.Detailed results are shown in Figure 4.
3.5 Risk factor analysis of hyperuricemia
As shown in Table 4, after adjusting for gender, age, and ethnicity,the higher the number of MS component abnormalities in MS1-MS4, the higher the risk of HUA in both males and females, whereas the risk of HUA in MS5 varied by gender, with a decrease in the risk of HUA in MS5 in males as compared to that in MS4, whereas females still showed an increasing trend.After further adjusting for BMI, elevated TC, elevated LDL-C, and coronary heart disease, in men, compared to MS0, the risk of HUA prevalence was increased by 0.379-fold, 0.808-fold, 1.483-fold, 1.478-fold, and 0.994-fold for MS1, MS2, MS3, M4, and MS5, respectively(all P<0.001), whereas,in women, The higher number of MS components, The higher risk of developing HUA, with ORs of 1.799, 2.532, 3.486, 4.530, and 5.988 for MS1, MS2, MS3, MS4, and MS5, respectively (all P<0.001).

Fig 2 Serum uric acid levels in people with different numbers of metabolic syndrome components

Fig 3 Prevalence of hyperuricemia in people with different numbers of metabolic syndrome components
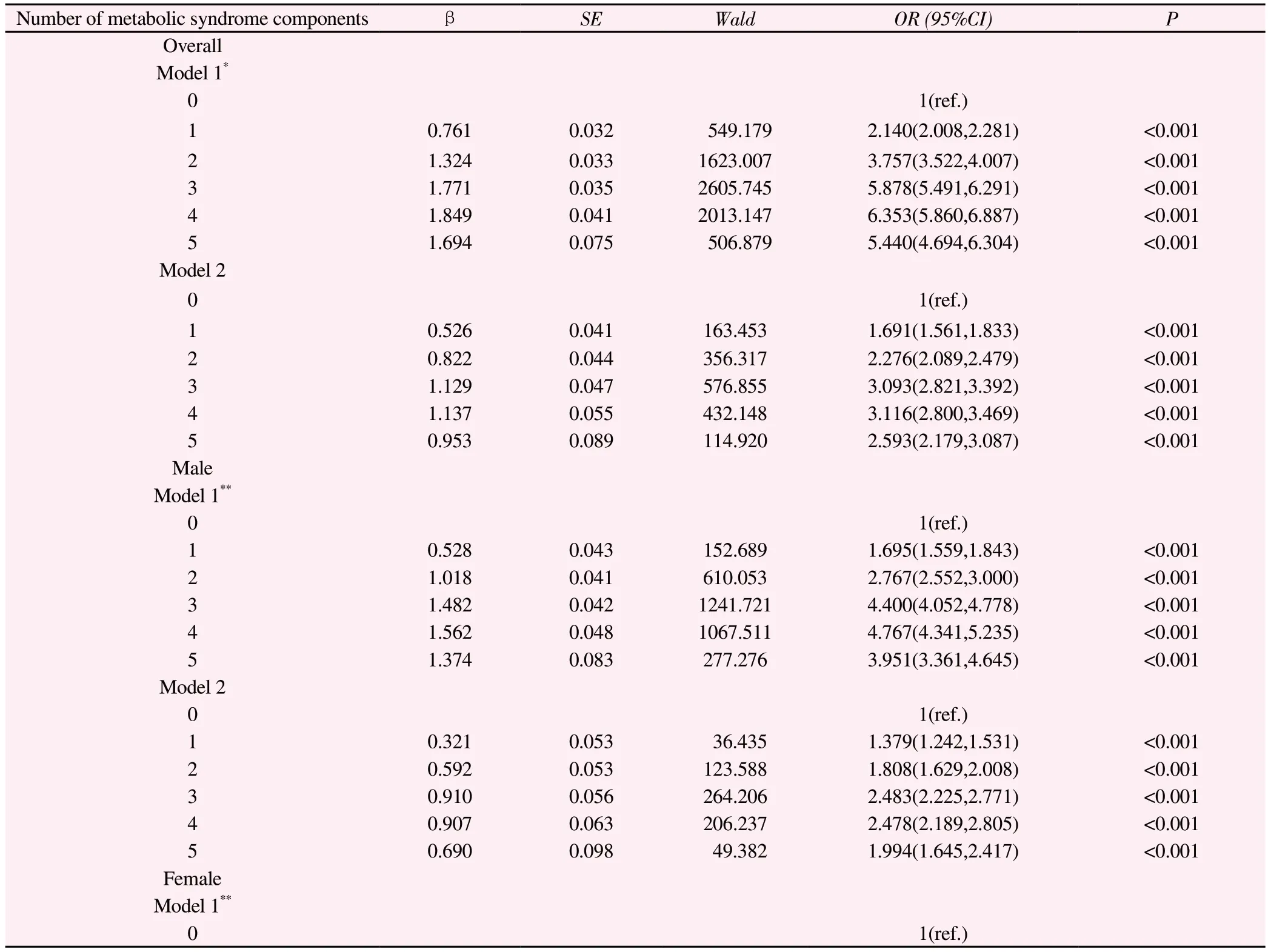
Tab 4 Logistic analysis of the number of metabolic syndrome components and hyperuricemia

Model 1*:Adjustment for gender, age (continuous variable) and ethnicityModel 1**:Adjustment for age (continuous variable) and ethnicityModel 2:Adjustment for BMI (continuous variable), increased TC, increased LDL-C, and coronary artery disease based on model 1.

Fig 4 Top five prevalence of hyperuricemia for metabolic syndrome component combinations
4.Discussion
This study was conducted to assess and determine the relationship between MS and HUA by analyzing the biochemical examination and physical examination data of 66,520 medical examiners from a hospital health management center.The results of this study showed that the levels of SUA and the prevalence of HUA in MS and its components were significantly higher than those in the control group,both in the overall, males and females, which is consistent with the results of previous studies[16—18].It has been shown that abdominal obesity is strongly associated with the development of HUA [19 20]and that higher waist circumference correlates with insulin resistance and leptin production, both of which can lead to a reduction in renal uric acid excretion [21].In patients with abdominal obesity,visceral fat accumulates and free fatty acids flow into the liver via the portal vein, where excess fatty acids stimulate TG synthesis,which ultimately leads to increased uric acid synthesis through activation of the purine de novo synthesis pathway[8,22].The relationship between hypertension and hyperuricemia is complex and often interacts with each other.Tian et al[23] found that either higher baseline SUA levels or increasing SUA levels with time could predict the progression from prehypertension to hypertension.In the present study, we also found that hypertensive patients had a higher SUA and HUA prevalence compared with normotensive patients, the mechanism of which may be that the renal microvascular damage produced by long-term hypertension leads to an increase in lactic acid production, which in turn competitively inhibits uric acid excretion, ultimately leading to an increase in SUA[24].
The results of the present study revealed gender differences in diabetes.In men, diabetic patients had lower SUA levels and prevalence of HUA compared to those with normal blood glucose levels, whereas in women the results were the opposite.A cohort study with 7 years of follow-up of HUA patients found that higher SUA levels during follow-up were associated with the development of diabetes only in women with hyperuricemia[25].Another cohort study found that individuals who developed diabetes during follow-up tended to have lower SUA levels, but this outcome was not observed in postmenopausal women [26].This supports our findings.A study from Sweden found that SUA levels increased with increasing blood glucose levels and that after blood glucose levels reached 7.0 mmol/L in men and 9.0 mmol/L in women, the increase in blood glucose was accompanied by a decrease in SUA levels[27].Therefore, we analyzed that gender differences in the relationship between diabetes and HUA may be attributed to genderspecific differences in the physiological effects of hyperuricemia and differences in the inflection point of the relationship between blood glucose and uric acid between males and females.The relationship between HUA and diabetes is controversial.Some studies have found no correlation between HUA and diabetes[28,29], while others have shown that SUA levels are only negatively correlated with blood glucose levels in men with diabetes.The mechanism for this lies in the fact that the reabsorption of uric acid and glucose in the proximal tubules of the kidneys goes through the same carriers, and that elevated blood glucose levels compete to inhibit the reabsorption of uric acid, which leads to a decrease in the level of SUA[16].Therefore, the relationship between uric acid and diabetes mellitus still needs more studies to be further proved.
We stratified the study population according to gender and found that in male MS1-MS4, SUA levels and HUA prevalence increased with an increasing number of components while decreasing in MS5.In contrast, in females, a higher number of MS components was associated with higher SUA levels and HUA prevalence.Whereas previous studies have reported that both SUA levels and HUA prevalence are increased with the increasing number of MS components in both males and females [30—33], We analyzed the reasons for this difference and found that there were five combinations of any combination of MS4 in men, and only the component without diabetes in the combination(abdominal obesity+ hypertension + reduced HDL-C + increased TG) was higher than the prevalence in MS5(abdominal obesity + hypertension + diabetes mellitus + reduced HDL-C + increased TG), (54.35% vs.37.40%),suggesting that diabetes may be negatively associated with HUA in men, as found in previous studies, and that diabetes has a greater contribution in reducing the risk of HUA in men.
The association of a single component of MS with HUA is limited,and studying MS as a whole also obscures the relationship evaluation and risk assessment of MS for HUA.Therefore, this study combined the components of MS to investigate the combined effects of the components on HUA and the differences in prevalence produced by the different combinations.Our findings revealed that abdominal obesity + hypertension + reduced HDL-C + evaluated TG had the highest prevalence of HUA in men (54.35%), while abdominal obesity + hypertension + diabetes+ reduced HDL-C + evaluated TG had the highest prevalence of HUA in women (41.46%).Therefore,the combination of the above MS components in both men and women should be the focus of attention and intervention to prevent and slow down the development of HUA-induced cardiovascular disease.
The results of logistic regression in this study found that among women, adjusting for age and ethnicity, the risk of HUA was increasing with the number of components, The risk of HUA in women MS5 was 13.372 times higher than in MS0, on further adjustment for BMI, increased TC, increased LDL-C, and coronary heart disease, this risk remained.This is consistent with the results of previous studies [26].This suggests that MS5 women should be focused on while choosing suitable lifestyle changes and dietary interventions.Whereas a linear trend between the number of MS components and the prevalence of HUA was not observed in men,the risk of HUA prevalence was decreased in MS5 compared to MS4 (2.478 vs.1.994) and the relationship between MS and the risk of HUA prevalence was less significant than in women.In the prevention of HUA, early detection and treatment of the MS components are beneficial in avoiding the occurrence of HUA and subsequent cardiovascular events.
In summary, abnormalities of MS components and different combinations are closely related to HUA, and different combinations of MS components have different risks of HUA.In the prevention and treatment of HUA, in addition to dietary control and lifestyle interventions, MS and its component abnormalities should attract widespread attention, which is of great significance for the prevention of HUA and cardiovascular diseases.There are some limitations to this study, The study was a cross-sectional study and therefore it was not possible to determine the causal relationship between MS and HUA.Due to the lack of information on dietary habits, and lifestyle, it was not possible to better control for these confounding factors, and we will follow up with these issues to further validate our results.
Authors’ Contribution
Xuanxia Wu was responsible for the data analysis and article writing of this paper; Juan Bu, Yanmin Zhang, Yeledan Mahan, Mingming Zhou, Yingying Ma, Huanhuan Lu, and Xiaoling Zhang collected and organized the data; and Ling Zhou proposed, designed, and implemented the study, and supervised the writing of the article.
The authors of this article declare that there are no conflicts of interest related to this manuscript.
杂志排行
Journal of Hainan Medical College的其它文章
- The prevention of high-fat diet-induced non-alcoholic fatty liver disease in mice by Fucoidan
- Mechanism of Qishen Decoction inhibition of macrophage M1 type polarization by targeting TGR5-mediated NLRP3 inflammasome
- Analysis of E2F3 gene variants, expression and clinical significance in melanoma based on multiple databases
- Meta analysis and data mining of the method of yishenhuoxue in the treatment of nonproliferative diabetic retinopathy
- Evaluation of the diagnostic efficacy of noninvasive diagnosis in patients with chronic viral hepatitis B complicated with nonalcoholic fatty liver disease and significant liver fibrosis
- Discover the key genes for glomerular inflammation in patients with type II diabetic nephropathy based on bioinformatics and network pharmacology
