Evaluation of the diagnostic efficacy of noninvasive diagnosis in patients with chronic viral hepatitis B complicated with nonalcoholic fatty liver disease and significant liver fibrosis
2024-01-19DOUJingLITIFUAbulimitiWANGXiaozhong
DOU Jing, LITIFU Abulimiti, WANG Xiao-zhong✉
1. The Fourth Clinical College of Xinjiang Medical University, Urumqi 830000, China
2. Xinjiang Medical University Affiliated Hospital of Traditional Chinese Medicine, Urumqi 830000, China
Keywords:
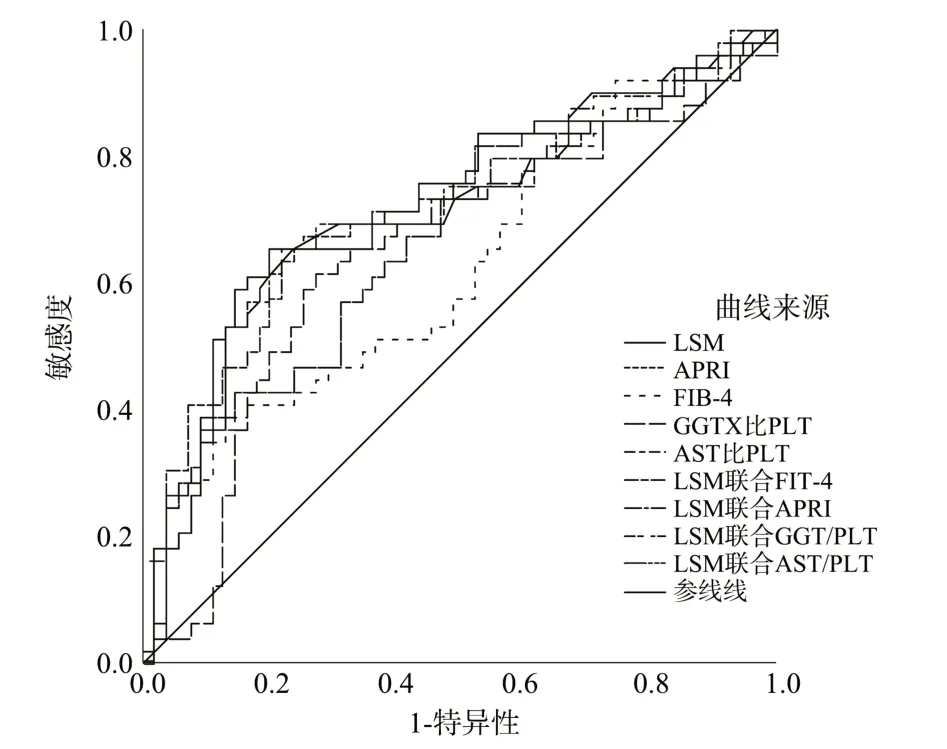
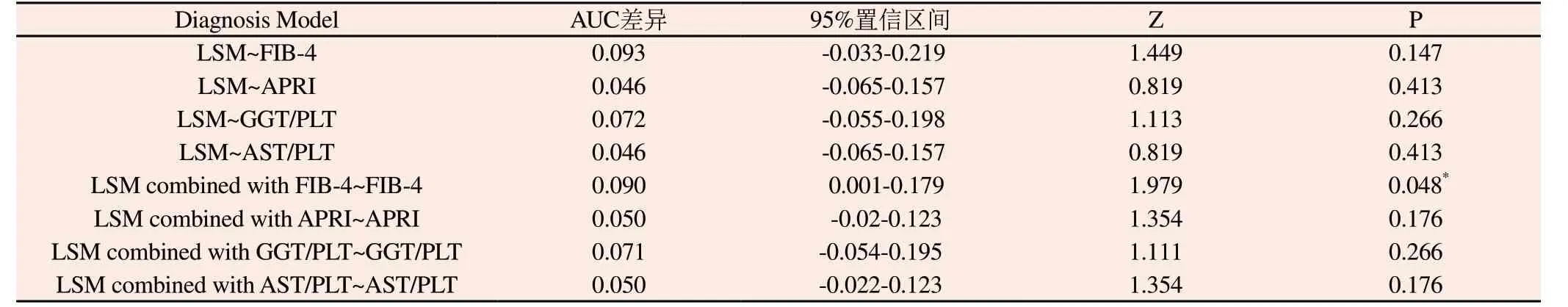
ABSTRACT Objective: To evaluate the diagnostic efficacy of chronic viral hepatitis B (CHB) with significant liver fibrosis ( S2) in patients with nonalcoholic fatty liver disease (NAFLD) by using noninvasive diagnosis and their combined models, and to explore their clinical features.Methods: A total of 104 inpatients with CHB diagnosed and complicated with NAFLD(hepatic steatosis suggested by liver biopsy) were retrospectively collected from January 2018 to January 2023 in the Affiliated Hospital of Traditional Chinese Medicine of Xinjiang Medical University.Liver biopsy was performed in all patients.General data, laboratory test results, liver hardness (LSM), FIB-4, APRI, GGT/PLT, AST/PLT and other results of patients were collected and grouped according to different fibrosis stages (S) to explore the clinical and pathological characteristics of patients with Hepatitis B virus (HBV) infection and nonalcoholic fatty liver disease (NAFLD) is a chronic liver disease (CLD) of the two important reasons, which can lead to cirrhosis and hepatocellular carcinoma (HCC).Although vaccination has largely reduced new HBV infections, WHO estimates that 3.5% of the global population(257 million people) still had chronic HBV infection in 2015[1-3].At present, there are some studies on chronic viral hepatitis B (CHB)combined with NAFLD.A Chinese study[4] analyzed 5680 CHB patients, and the results showed that 31.1% of CHB patients were complicated with NAFLD.Another study[5] included 4734 CHB patients, with NAFLD accounting for 26.9%.Other studies from Malaysia, Turkey and Thailand [6-9] showed that the prevalence of CHB combined with NAFLD was about 30%~50%.Although some studies[10-13] have shown that patients with NAFLD have a higher clearance rate of hepatitis B surface antigen (HBsAg) and may inhibit HBV replication.However, some relevant studies [13-15] have confirmed that NAFLD may aggravate the degree of liver fibrosis in patients with CHB.Therefore, early identification, monitoring,management and treatment of liver fibrosis in patients with CHB and NAFLD are essential.This study by using the method of noninvasive assessment of liver fibrosis, evaluate the significant liver fibrosis in patients with CHB with NAFLD (S2) or higher diagnostic value,in order to noninvasive diagnostic method in clinical use to provide more evidence. A total of 104 hospitalized patients diagnosed [16] with CHB and NAFLD (liver biopsy showed hepatic steatosis) in the Traditional Chinese Medicine Hospital Affiliated to Xinjiang Medical University from January 2018 to January 2023 were retrospectively collected.Inclusion criteria: (1) the age of 18 years old or more; (2) HBsAg positive more than 6 months, HBeAg negative or positive; (3) HBV- DNA can be detected; (4) Liver biopsy was performed; (5) patients with steatosis and liver fibrosis ( S2). Exclusion criteria: (1) Co-infection with HCV virus or other viral hepatitis, autoimmune liver disease, alcoholic liver disease,inherited metabolic liver disease, etc.(2) patients with liver cirrhosis confirmed by imaging or pathology; (3) patients with decompensated cirrhosis; (4) merger of malignant tumor patients. Collect all of the patients of liver biopsy pathology results, And general information, liver function [alanine aminotransferase (ALT),aspartate aminotransferase (AST), alkaline phosphatase (AKP),γ-glutamyl transpeptidase (GGT), serum albumin (Alb), blood routine [white blood cell (WBC), hemoglobin (HGB), platelet(PLT)], liver stiffness measurement (LSM), hepatitis B Hepatitis B surface antigen (HBsAg) was quantified, hepatitis Be antigen(HBeAg) was qualitative, and coagulation function [prothrombin time (PT), prothrombin activity (PTA), fibrinogen (FIB)] was calculated.Fib-4 index, APRI score, AST/PLT ratio and GGTPLT ratio were calculated.The clinical data of patients with stage S2 and stage S2 were compared.The receiver operating characteristic(ROC) curve was used to analyze the area under the curve (AUC),sensitivity (Se), specificity (Sp) of the three non-invasive diagnostic methods and their combined model of liver fibrosis, and the cut-off value (cut-off value) was calculated to compare the AUC values of each non-invasive method.Evaluate the noninvasive method of CHB patients with NAFLD with significant liver fibrosis significantly the diagnostic value of liver fibrosis. Rapid liver biopsy was performed, and the informed consent for liver biopsy was signed by the patients and their families.Blood routine, coagulation function, blood type and basic vital signs were examined before operation.Liver tissues were fixed in 10%formaldehyde solution, paraffin embedded sections, and routine HE staining was performed.Pathological diagnosis was performed by the Department of Pathology, Traditional Chinese Medicine Hospital Affiliated to Xinjiang Medical University.Diagnostic criteria for fibrosis degree (S) of liver histopathology[17] : S1: Enlarged fibers in the portal area, local sinusoid and lobular fibrosis; S2:fibrosis around the portal area, fibrous septum formation, lobular structure preservation; S3: fibrous septum formation, lobular structure disorder, no cirrhosis; S4: Early cirrhosis or definite cirrhosis.Inflammatory activity (G) : G1: portal inflammation,intralobular degeneration and a few necrotic foci; G2 showed mild fragmented necrosis in and around the portal area, intralobular degeneration, point or focal necrosis or eosinophilic bodies.G3:moderate fragmented necrosis in and around the portal area, severe degeneration, necrosis or bridging necrosis in the lobules; G4: Severe fragmented necrosis in and around the portal area, extensive bridging necrosis in the lobule, involving multiple lobules, and abnormal lobular structure. Formula of FIB-4: FIB-4=[age (years)×AST(U/L)]/[PLT(×109/L)×√ALT], APRI index calculation formula: APRI=[(AST/ULN)×100/PLT(×109/L)], GThe ratio of GGT to PLT: GGT/PLT, AST and PLT ratio: AST/PLT. Before liver biopsy, liver stiffness measurement (LSM) was measured and recorded using a liver transient elastography scanner(FibroTouch-B, Wuxi Hisikel Medical Technology Co., LTD, China)according to the user’s manual of FibroTouch. SPSS 23.0 was used for statistical analysis.The measurement data in line with normal distribution were expressed as mean ± standard deviation (±s), the comparison between groups was analyzed byttest, and the non-normal distribution was expressed as median(interquartile range) [M(P25-P75)].Mann-Whitney U test was used for comparison between groups, and the count data were expressed as the number of cases (percentage), and the chi-square test or Fisher test was used.Adopts the receiver-operating characteristic curve(ROC) and the area under the ROC curve (AUC) in the evaluation of noninvasive diagnostic method of advanced forecast value of liver fibrosis.The Youden index was used to determine the cut-off value,and MedCalc 19.3.0 was used to compare the AUC values of each non-invasive method.P<0.05 was considered statistically significant. There were 68 males and 36 females, with an average age of 46.19±9.14 years.There were 55 patients in S1 stage, 32 patients in S2 stage, 11 patients in S3 stage, and 6 patients in S4 stage. In patients with S1, S2, S3, and S4 stages, 92.73%, 96.88%,100%, and 100% of the patients had inflammation above G2 stage,respectively.There were significant differences in AST, Alb, PLT,PT, PTA, HBV DNA, inflammation stage, GGT/PLT, AST/PLT,LSM, FIB-4 and APRI among the groups (P<0.05).(Table 1) Among 104 patients, 55 patients were in The area under the ROC curve was used to evaluate the diagnostic value of each non-invasive diagnostic method and its combination method in CHB patients with NAFLD S2 stage.The AUC value of LSM was 0.716 (0.614-0.818), the sensitivity was 0.653, and the specificity was 0.764.The AUC of FIB-4 was 0.623, the sensitivity was 0.408, and the specificity was 0.836.The AUC of APRI was 0.669, the sensitivity was 0.816, and the specificity was 0.473.The AUC of GGT/PLT was 0.644, the sensitivity was 0.612 and thespecificity was 0.727.AST/PLT AUC 0.669, sensitivity of 0.816,a specific degree is 0.473.LSM joint FIB - 4 AUC is 0.712 (0.610 0.814), the sensitivity of 0.653, 0.236.The AUC of LSM combined with APRI was 0.719 (0.618-0.821), the sensitivity was 0.653, and the specificity was 0.800.The AUC of LSM combined with GGT/PLT was 0.715 (0.612-0.817), the sensitivity was 0.653, and the specificity was 0.782.The AUC of LSM combined with AST/PLT was 0.719 (0.618-0.821), the sensitivity was 0.653, and the specificity was 0.800.(Table 3, Figure 1) Tab 1 Clinical pathological features of patients with liver fibrosis in each stage of CHB combined with NAFLD Tab 2< S2 and S2 groups of patients with clinical and pathological features Among the non-invasive diagnostic methods, LSM had the best diagnostic efficiency, and AUC was higher than FIB-4, APRI,GGT/PLT, and AST/PLT, but the differences were not statistically significant (P>0.05).LSM combined with FIB-4, APRI, GGT/PLT and AST/PLT were used to evaluate CHB patients with NAFLD S2.The results showed that the diagnostic efficacy of LSM combined with FIB-4 was higher than that before, and the AUC difference between LSM combined with FIB-4 and FIB-4 was 0.090, which was statistically significant (P>0.05).(Table 4) The number of chronic HBV infection is still high in China[16],with the increase of the prevalence of NAFLD, merger of CHB patients with NAFLD increasing, need to cause enough attention.The effect of NAFLD on the progression of HBV infection is still not very clear.Regardless of the conclusion of the current relevant research, NAFLD and CHB are chronic liver diseases, which pose a serious threat to the health of patients by destroying liver function and aggravating liver fibrosis and progressing to end-stage cirrhosis or hepatocellular carcinoma [18].Therefore, early diagnosis and intervention in the stage of liver cirrhosis are also the key ways to prevent the progression of CHB complicated with NAFLD. Tab 3 The diagnostic value of non-invasive diagnostic methods for significant liver fibrosis ( S2) in CHB complicated with NAFLD patients Fig 1 Noninvasive diagnostic methods significant liver fibrosis patients in CHB complicated with NAFLD ( S2) diagnostic value of ROC curve Liver biopsy has been the cornerstone of treatment decisions and prognosis in chronic liver disease and remains the “gold standard”for assessing the staging of injury, inflammation, and fibrosis.Liver biopsy has been a cornerstone of chronic liver disease treatment decisions and prognosis, and evaluate injury, inflammation, and fibrosis stage is still the “gold standard”, but because of its reasons,and so on have the invasive degree of patients accepted, along with the development of the noninvasive diagnostic technique, many with serum biochemical markers or imaging methods to evaluate the degree of liver fibrosis in patients with chronic liver disease. Such as FIB-4 index (Fibrosis Score 4) was firstly put forward in 2006 by Sterling[19] a noninvasive assessment of liver Fibrosis in patients with chronic liver disease of a kind of method, APRI Score is put forward by doctors in the United States, used for assessment of liver Fibrosis and cirrhosis of the liver[20].The above two non-invasive assessment methods are based on mathematical models constructed based on serological indicators.LSM is obtained by transient elastography, point shear wave elastography, and twodimensional shear wave elastography, which belongs to imaging methods. Tab 4 Comparison of the diagnostic efficacy of non-invasive methods In this study, we analyzed the CHB complicated with NAFLD patients , and the results showed that there was a trend of more severe fibrosis and more severe inflammation in patients with S1 to S4 stages, and there were statistically significant differences in the non-invasive liver fibrosis diagnostic methods GGT/PLT, AST/PLT,LSM, FIB-4, and APRI among the four groups (P < 0.05).And in In conclusion, the number of cases included in this study was small,and the proportion of S3 and S4 patients was low, but the results of this study suggest that although the currently commonly used clinical non-invasive liver fibrosis assessment methods have certain diagnostic efficacy for CHB complicated with NAFLD significant liver fibrosis, they cannot replace liver biopsy.Noninvasive assessment of liver fibrosis method is non-invasive, operation convenience and other advantages, can be used as an auxiliary method of liver biopsy in clinical for assessment on a regular basis.In the future, we hope to further expand the sample size to further confirm the results of this study, and hope to develop new and better non-invasive diagnostic methods for assessing liver fibrosis in patients with CHB and NAFLD. All authors’ conflict of interest statement and contribution statement In this paper, all the authors have no conflict of interest, Dou Jing responsible for data statistics and article writing, Litifu Abulimiti responsible for data entry, Wang Xiaozhong is responsible for the conception and audit.1.Introduction
2.Materials and Methods
2.1 Patients
2.2 Research Methods
2.3 Liver Biopsy
2.4 Noninvasive Diagnosis of Liver Fibrosis Indexes
2.5 FibroTouch examination
2.6 Statistical analysis
3.Results
3.1 General Information
3.2 Clinical and pathological data characteristics of patients with different stages of liver fibrosis in CHB combined with NAFLD
3.3 Clinical and pathological characteristics of CHB complicated with NAFLD patients in
3.3 The diagnostic value of non-invasive methods for significant liver fibrosis ( S2) in CHB complicated with NAFLD patients


4.Discussion

杂志排行
Journal of Hainan Medical College的其它文章
- The prevention of high-fat diet-induced non-alcoholic fatty liver disease in mice by Fucoidan
- Mechanism of Qishen Decoction inhibition of macrophage M1 type polarization by targeting TGR5-mediated NLRP3 inflammasome
- Epidemiological characteristics of hyperuricemia in metabolic syndrome and its different components in the physical examination population
- Analysis of E2F3 gene variants, expression and clinical significance in melanoma based on multiple databases
- Meta analysis and data mining of the method of yishenhuoxue in the treatment of nonproliferative diabetic retinopathy
- Discover the key genes for glomerular inflammation in patients with type II diabetic nephropathy based on bioinformatics and network pharmacology
