Transient hyperphosphatasemia in a toddler with COVID-19 infection: A case report and literature review
2023-11-16PemigaSukhupanyarakVoraluckPhatarakijnirund
Pemiga Sukhupanyarak, Voraluck Phatarakijnirund
Abstract
Key Words: Alkaline phosphatase; Coronavirus; Pediatric endocrinology; Case report
INTRODUCTION
Transient hyperphosphatasemia (TH) is a benign and self-limiting condition characterized by a marked increase in serum alkaline phosphatase (ALP) in the absence of liver or bone disease[1].The elevated serum ALP level usually declines into the normal range within a few months[1,2].TH is observed in either sick or healthy infants and children under the age of 5 by finding incidentally elevated serum ALP on routine laboratory investigation for other purposes[3-8].Although its etiology remains unclear, the propensity of TH associated with various conditions, such as post organ transplantation,hematologic malignancy, rheumatologic disease[9-11], and, in particular, infectious diseases, has been reported in the literature[5,12,13].
Coronavirus disease 2019 (COVID-19) infection is a highly contagious infection that quickly became a global pandemic disease.Endocrinopathies associated with COVID-19 infection in children, such as thyroid diseases (subacute thyroiditis,hypothyroidism, hyperthyroidism), adrenal insufficiency, diabetes mellitus, vitamin D deficiency and hypopituitarism,had been previously reported[14,15].TH observed with COVID-19 infection in toddlers is a new discovery that was recently described in two cases[16,17].Here, we report a case of a 2-year-old boy who developed TH associated with COVID-19 infection.
CASE PRESENTATION
Chief complaints
A previously healthy 2-year-old boy was admitted to our hospital with an acute febrile illness of 4 d duration.
History of present illness
There was a history of the patient being in close contact with his grandfather, who was later diagnosed with symptomatic COVID-19 infection.The patient had a positive test of real-time reverse transcription polymerase chain reaction for severe acute respiratory syndrome coronavirus 2.
History of past illness
He was a full-term baby with a birth weight of 2800 g, requiring no medication since his birth.
Personal and family history
No special notes.
Physical examination
The physical examination upon admission revealed that the patient was in good general condition, with no sign of respiratory distress or dehydration, body temperature 37.6°C, pulse rate 90/min, respiratory rate 22/min and O2saturation in room air 99%.His weight and height were 12.1 kgs (-0.7 SDS) and 86.5 cm (+0.7 SDS), respectively.The skeletal examination revealed no wrist joint swelling, rachitic rosary, knock knee or abnormal gait to suggest definite skeletal disease.There were no clinical findings of jaundice or hepato-splenomegaly to indicate hepatobiliary disease.
Laboratory examinations
The initial laboratory results showed hemoglobin 13.3 g/dL, white blood cell 10100/µL with 61.6% lymphocytes and platelet count 196000/µL.Chest X-ray revealed no infiltration.The liver function test (LFT) on the 5thday of his illness showed a markedly elevated serum ALP of 4178 U/L (normal range: 111-277).Additionally, the occurrence of bone or hepatobiliary disease was assessed, and the results were normal as follows: Blood urea nitrogen 12.4, Cr.0.3, calcium 9.9,phosphate 4, magnesium 2.2 mg/dL, intact-PTH 21.3 pg/mL, 25-OHD 33.6 ng/mL and gamma-glutamyl transferase 12 U/L (Table 1).The serum ALP was repeated 4 d following the initial study.It remained elevated at 4662 U/L, but the rest of the LFT was normal.
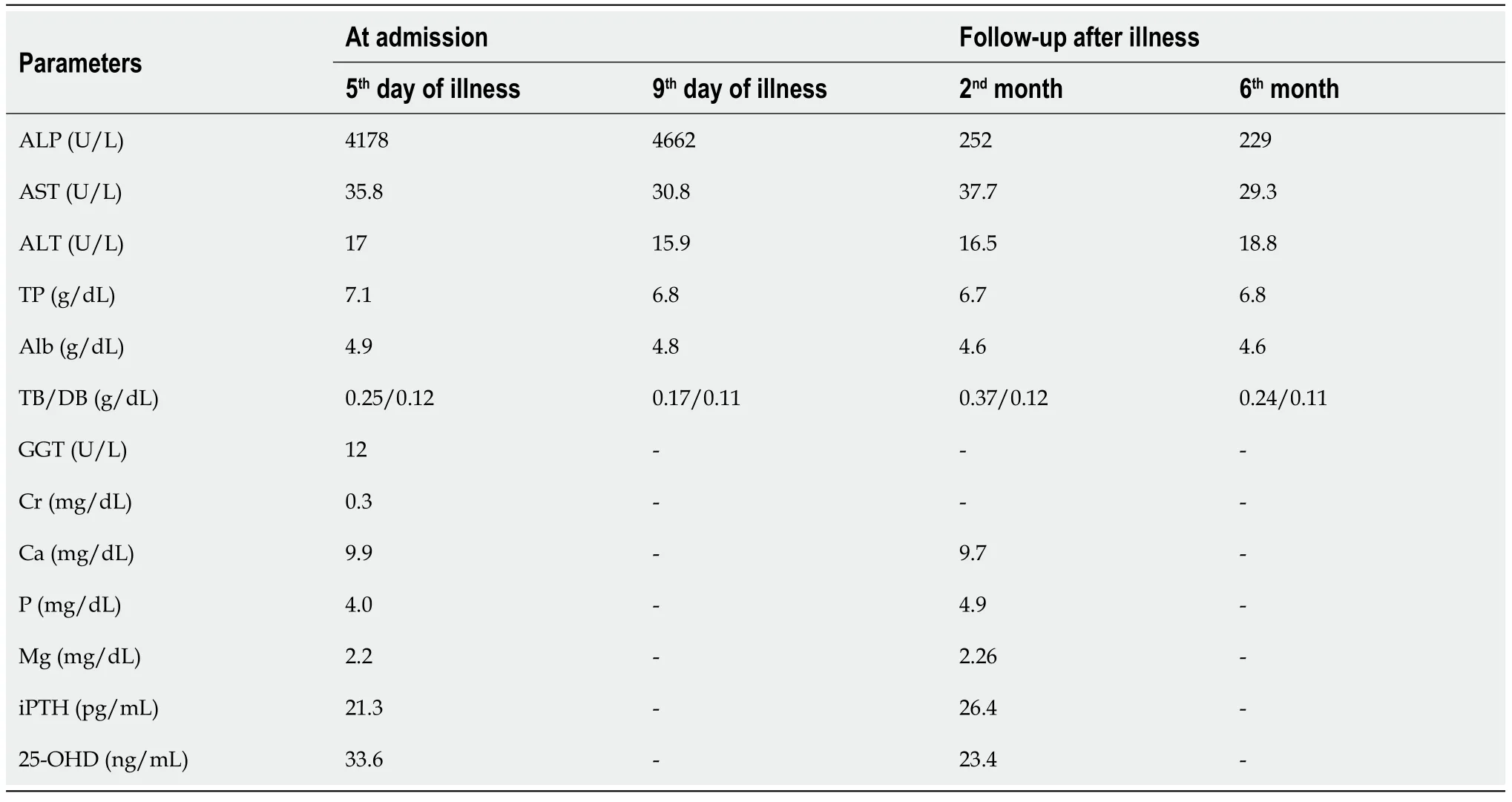
Table 1 Laboratory tests of our patient during coronavirus disease 2019 infection and follow-up
Imaging examinations
No special notes.
FINAL DIAGNOSIS
At this point, the diagnosis of TH was strongly considered.The entire 7 d of his hospital course was uneventful without fever, diarrhea or respiratory tract symptoms.
TREATMENT
The management was symptomatic and supportive care with oral antipyretic, anti-emesis and oral rehydration solution.
OUTCOME AND FOLLOW-UP
Two months after discharge, the patient was re-evaluated at the outpatient endocrine clinic.His physical examination was normal.Serum ALP became normal at 252 U/L.The other investigations, including LFT, calcium, phosphorus,magnesium, 25-OHD and skeletal survey radiography, were completely normal.A six-month follow-up study with the same parameters as the 2-month follow-up study revealed that everything remained within the normal range (Table 2).
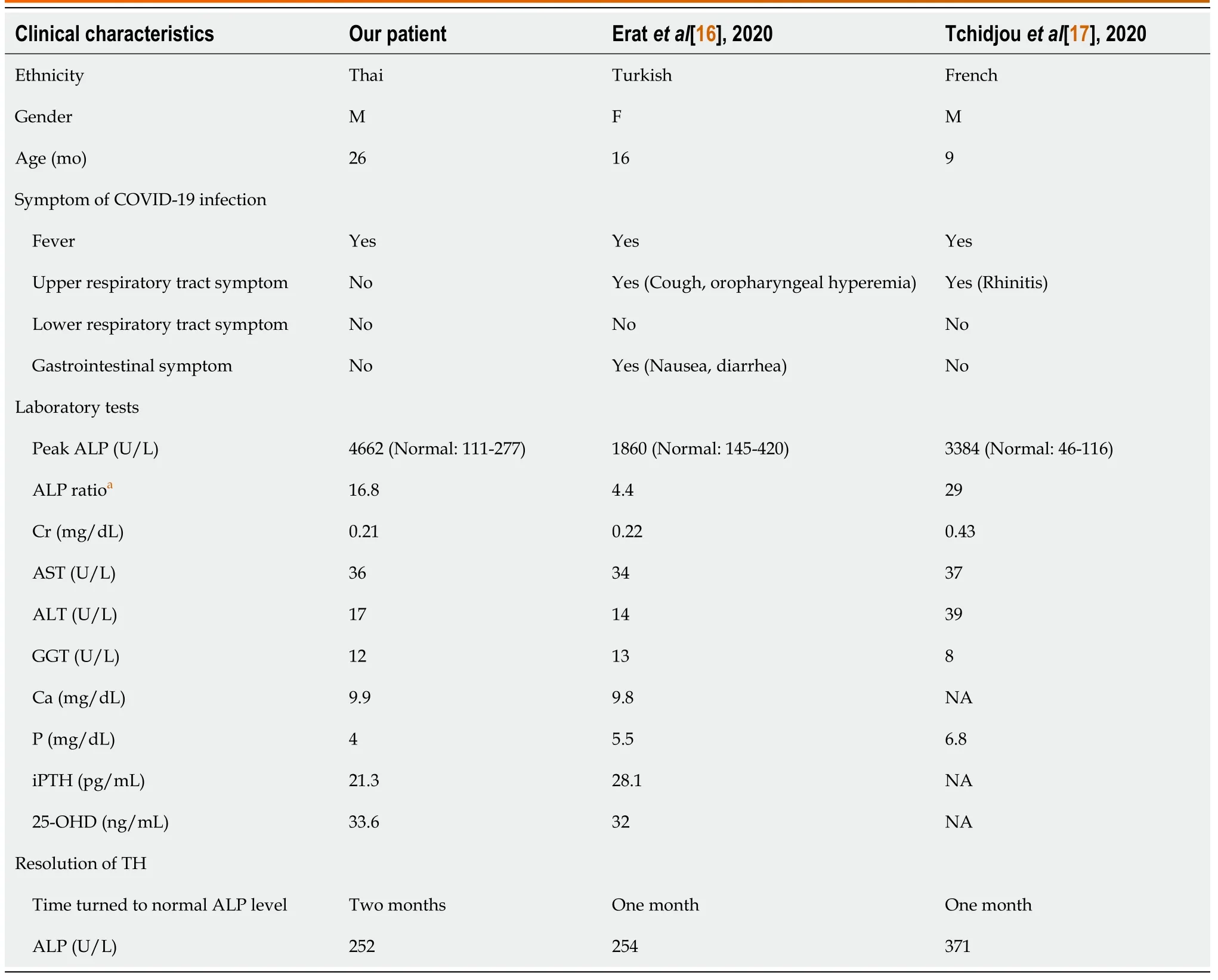
Table 2 Clinical characteristics and laboratory tests in hyperphosphatasemia associated with coronavirus disease 2019 infection: our patient and previous reports
DISCUSSION
ALP is a membrane-bound phosphomonoesterase enzyme consisting of four isoenzymes, three tissue-specific ALPs(intestinal, placental and germ cell) and the tissue-nonspecific ALP (TNSALP)[18].TNSALP is abundant in the bone, liver and kidney and accounts for 95% of total ALP activity in serum[19].Therefore, abnormally high ALP levels are an important marker for skeletal and hepatobiliary diseases.
TH is a benign self-limited condition that reportedly has a prevalence from 1.1% to 3.5% among infants aged 2-24 mo and affects both sexes equally[20,21].This condition was first described in 1954 by Bach[22].In 1985, Krautet al[2]established the criteria for the diagnosis of TH in infancy and children, defined as an age group below 5 years, no evidence of bone or liver disease on physical examination or laboratory test, elevation of both bone and liver ALP isoenzymes and a return to normal serum AP values within 4 mo.Although the specific cutoff value of ALP level for diagnosis of TH had not been identified by the original criteria, recent studies have suggested that TH is considered when serum ALP is above 800[5,13], 1000 (6, 11, 21) or 2000 U/L[23].However, the peak serum ALP of TH was distinctively higher than the serum ALP levels of other bone and hepatic diseases.In a review of 733 TH patients, the mean ALP level was 9 times above the upper limit of the normal range, and 71% of these patients had the highest ALP > 5 times above the upper limit of the reference value[4].
Numerous reports have identified various viral infections as contributing factors to the etiology of TH (Table 3)[13,23-27].Suzukiet al[28] identified antibodies against enteroviruses, such as ECHO 22, entero-71 and coxsackie B4, in the serum of 50 TH children.Among these viruses, ECHO 22 antibody was most frequent, accounting for 32% of TH cases.Additionally, few but not all studies reported clusters of TH during the fall and winter seasons, which supported the assumption of the viral etiology[3,12,21].
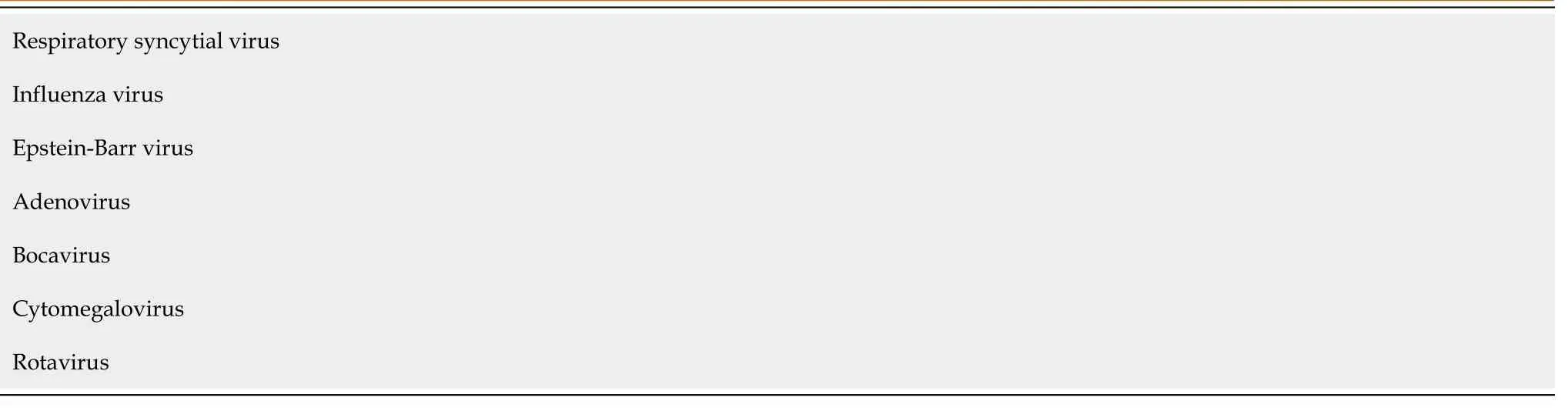
Table 3 Viral infections associated with hyperphosphatasemia [13,23-27]
The mechanism of TH is obscure.Several hypotheses have been postulated, including increased activities of ALP in plasma, increased production and impaired clearance of ALP.The most likely mechanism is decreased hepatic clearance due to the high sialic acid content of ALP, but the mechanism involved in excessive sialic acid content of the molecule is unknown[29].Increased bone ALP production is thought to be a result of increased bone resorption triggered by virus infection, consequently increasing osteoblast activities and bone formation and hence increasing bone turnover.This was supported by evidence of transiently increased urinary hydroxyproline (bone resorption marker) excretion[30].In contrast, the study by Kutileket al[8] in 2012 showed a lack of elevated iPTH, Beta-CrossLaps and osteocalcin in TH patients.As such, the hypothesis of increased bone turnover leading to elevated ALP in TH remains controversial.
TH typically resolves without any treatment.A reduction in ALP level to the normal range occurs between 2 wk and 4 years with a median of 10 wk[4].In 80% of cases, ALP returns to the normal level in 16 wk[4].
Our patient, who was confirmed to have an active COVID-19 infection, exhibited typical clinical features of TH,including high serum ALP levels and no clinical or laboratory evidence of bone or hepatic disease.His biochemical markers of bone metabolism were normal, including calcium, vitamin D and intact PTH.ALP isoenzyme assays were not available at our facility, nor were the other more specific tests for bone turnover markers.The markedly elevated ALP in our patient became normal within 3 mo of follow-up and remained stable at the 6-month follow-up.Given the reports of TH associated with other viral infections, we concluded that our patient developed TH related to COVID-19 infection.Recently, two cases of TH associated with COVID-19 infection in children have been reported[16,17].All 3 cases,including ours, were aged under 3 years, in accordance with the preponderance (82%) of TH in patients aged < 36 mo in a previous report[4].The peak level of ALP appears to have no association with the severity of the illness.In our patient,the peak ALP was at 4, 662 U/L (16.8 times to upper normal range), while his symptoms were mild only with low-grade fever.However, the other 2 previous cases had additional clinical symptoms of the upper respiratory tract and gastrointestinal symptoms, but peak levels of ALP appeared to be lower (Table 2).Nonetheless, the serum ALP levels of all 3 cases were similar to those in previous case reports, ranging from 805 to 16814 U/L[3,5,8].Our patient had the serum ALP return to the normal range of 252 U/L at 2 mo after the acute illness, which is similar to most of the TH cases.In the 2 previous cases of TH associated with COVID-19 infection, their ALP levels declined to the normal range within a month(Table 2).This can be explained by their early schedule testing compared to ours.
In summary, we demonstrated a typical case of TH in a toddler who had been confirmed to have acute COVID-19.It is likely that a rising number of TH cases will be observed along with continuation of the COVID-19 pandemic.
CONCLUSION
Transient hyperphosphatasemia is a benign and self-limiting condition that occurs mainly in infants and children under the age of 5.This condition can be found in toddlers with COVID-19 who exhibit an isolated high level of serum ALP without evidence of bone or hepatic disease based on physical examination and laboratory testing.Therefore, follow-up monitoring of serum ALP levels to confirm the resolution of hyperphosphatasemia without additional extensive investigation and treatment is recommended.
ACKNOWLEDGEMENTS
We are grateful to Dr.Ruenrudee Suwannasri for suggesting and review of manuscript and would like to thank the patient and family participated in this study.
FOOTNOTES
Author contributions: Sukhupanyarak P and Phatarakijnirund V contributed to manuscript writing and editing, data collection and final approval of the version of the article to be published
Informed consent statement:Subjects and legally authorized representative gave their written and verbal informed consent prior to study inclusion.
Conflict-of-interest statement:All authors state that they have no conflicts of interest.
CARE Checklist (2016) statement:The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Thailand
ORCID number:Pemiga Sukhupanyarak 0000-0001-7441-7608; Voraluck Phatarakijnirund 0000-0002-0955-083X.
S-Editor:Liu JH
L-Editor:A
P-Editor:Liu JH
杂志排行
World Journal of Clinical Pediatrics的其它文章
- Radiation dose analysis of computed tomography coronary angiography in Children with Kawasaki disease
- Safety and efficacy of intravitreal anti vascular endothelial growth factor for severe posterior retinopathy of prematurity with flat fibrovascular proliferation
- Accidental ingestion of foreign bodies/harmful materials in children from Bahrain: A retrospective cohort study
- Gastrointestinal and nutritional care in pediatric neuromuscular disorders
- Role of gastrointestinal health in managing children with autism spectrum disorder
- Use of endolumenal functional lumen imaging probe in investigating paediatric gastrointestinal motility disorders
