Use of endolumenal functional lumen imaging probe in investigating paediatric gastrointestinal motility disorders
2023-11-16EmilyWhiteMohamedMutalib
Emily White, Mohamed Mutalib
Abstract
Key Words: Endolumenal functional lumen imaging probe; Paediatric; Gastrointestinal motility
INTRODUCTION
Investigating gastrointestinal (GI) motor function requires a careful assessment of muscle contractions and sphincters function[1].Manometries can directly measure the lumen-generated pressure and are considered the gold standard to evaluate the strength and propagation of muscle contractions, peristalsis velocity and the integrity and coordination of different types of GI sphincters[2].Sequential multi-channel impedances, in isolation or combined with manometry, will evaluate the directional flow and the bolus transit[3].However, it has long been recognised that the competency of GI sphincters does not always relate to the tightness of their contractions[4-6].Measuring the resistance to distension, also known as distensibility assessment, can provide an accurate geometric measurement of the sphincters and a plethora of diagnostic information[7].
Endolumenal functional lumen imaging probe (EndoFLIP) uses the principles of impedance planimetry, a technical term that describes the measuring of the cross-sectional area (CSA) of a distending bag by using an internal electrical impedance measurement[8,9].EndoFLIP consists of 16 sensors and a solid state pressure transducer placed inside a distensible and compliant balloon to provide a measurement length of 8 or 16 cm[10].EndoFLIP is used during endoscopy under the same anaesthesia.To obtain the desired data, the balloon is filled with a conducting fluid (in a predetermined volume) (Figure 1), then the system will run a constant alternating current and the voltage difference between the excitation and the detection electrodes is measured[11].The voltage is mathematically proportioned to the CSA of the balloon, from which, the balloon diameter can easily be calculated[12].The EndoFLIP data will be presented as geometric plots and will provide the following values: Distensibility is the resistance of the luminal wall to a distending force, compliance is the change in volume in response to a change in pressure, the CSA, the internal diameter of the balloon and the intra balloon pressure[13,14] (Figure 2A).
EndoFLIP has been increasingly used in clinical practice to study the lower oesophageal sphincter (LOS), the pylorus and the anal sphincters[11].It has also been used to assess distensibility of the oesophageal body in conditions such as eosinophilic oesophagitis (EoE)[15] and to guide surgical interventions (e.g.,during and post fundoplication)[16].Recently, EndoFLIP topography was developed allowing real life display of the balloon diameter continuum during volumetric distension.Oesophageal body contraction can then be visualised and analysed[17,18] (Figure 3).
In this article, we aim to review the use of EndoFLIP as a tool to investigate GI motility disorders with a special focus on paediatric practice.We searched PubMed database for English Language literature on the following keywords:EndoFLIP; Gastrointestinal Disorders; GI disorders; oesophagus; pylorus; rectum; anorectum; paediatric; children using AND/OR combination as appropriate.The extracted articles were reviewed and their salient findings were summarised and presented in the headings below.
Uses of EndoFLIP in the oesophagus
The oesophageal body, the LOS and the upper oesophageal sphincter were the most commonly studied part of the GI tract in regards to EndoFLIP measurement[19].Normative values from healthy adults have been recently published in a meta-analysis[20].
Achalasia
Achalasia is an uncommon oesophageal motility disorder, characterised by impaired relaxation of the LOS and absent or spastic oesophageal body contractions[21].It has three distinct types based on peristalsis patterns: Absent peristalsis in type I, pan-oesophageal body pressurisation in type II and an abnormal peristalsis with premature contractions in type III[22].Impaired LOS relaxation is the hallmark of all three types.High resolution oesophageal manometry (HROM) is universally agreed on as the gold standard tool to diagnose and characterise achalasia[23].
In adults, EndoFLIP assessment of LOS can appropriately identify patients with achalasia who may have a normal integrated relaxation pressure but other features of achalasia[4,6].EndoFLIP was able to bridge a gap in the understanding of the physiological behaviour of the LOS and the limitation of HROM as a sole diagnostic tool for major oesophageal motor disorders[24,25].LOS distensibility index (DI) of < 2 mm2/mmHg is strongly suggestive of an obstructive process and is significantly lower in patients with achalasia compared to healthy volunteers[21,26,27].LOS DI also appears to correlate well with achalasia symptoms prior to and after therapeutic interventions; achieving a definitive increase in DI after pneumatic dilatation was reported to be associated with improved clinical response[26,28].Using DI,CSA and balloon pressure as complementary data can help predict response to therapeutic interventions [Heller’s myotomy and peroral endoscopic myotomy (POEM)] in patients with achalasia[29-31], however, the data on the use of EndoFLIP parameters as a predictor of pneumatic dilatation response is conflicting, Rohofet al[26] experience showed a positive outcome while Smeetset al[32] reports no added therapeutic benefits.
In paediatrics, EndoFLIP has been used intra-operatively during POEM and laparoscopic myotomy to guide and assess the immediate post-procedural DI[33,34].The authors have reported a significant improvement in DI from baseline and a successful clinical outcome.Howket al[33] have reported on the use of intra-operative EndoFLIP with the balloon inflated throughout the procedure to guide the myotomy length and provide a real time feedback on DI and CSA.Their use of EndoFLIP resulted in a shorter operative time.Figure 2A is showing EndoFLIP data from a child with type 1 achalasia showing reduced LOS DI and diameter.
EoE
EoE is a chronic immune mediated and eosinophil predominant inflammation characterised by symptoms related to oesophageal dysfunction[35].EoE is associated with many types of oesophageal motility disorders and often thought to be secondary to oesophageal remodelling and fibrosis[36,37].Oesophageal strictures and luminal narrowing are also common in patients with EoE[38,39].Early identification of lamina propria fibrosis is crucial in guiding therapeutic strategies and endoscopic assessment but mucosal biopsies have a poor correlation with the degree of oesophageal fibrosis[40,41].HROM findings are not specific or sensitive to EoE motility disorders and they do not describe a characteristic pattern for EoE symptoms[42,43].
In adults, EndoFLIP can provide an accurate information in relation to oesophageal distensibility and compliance.Reduced oesophageal distensibility is reported in both children and adults with EoE and is associated with increased risk of food bolus impaction and the need for oesophageal dilatation[40,44].Distensibility is also significantly reduced in children with active EoE compared to an age matched control and the natural increase in oesophageal distensibility normally observed with age, appeared to plateau in children with EoE[44,45].This may represent a fibrotic remodelling or a separate EoE phenotype[44].Figure 2B is a child with EoE and reduced diameter/distensibility.
In paediatrics, a reduced oesophageal distensibility was reported in children with EoE and high endoscopic reference score part of (EREF)[44].In EREF, rings and strictures are considered as features of fibrosis and remodelling changes,while oedema, furrows and exudates are considered as features of inflammatory changes[46].It is increasingly recognised that inflammatory features can progress to fibrosis and remodelling in the context of EoE and although children can predominantly present with inflammatory EoE phenotype, early fibrosis in paediatric patients is commonly described[44,45].Oesophageal DI, but not CSA or diameter, has a strong correlation with endoscopic fibrostenotic severity and history of food bolus impaction in paediatrics independent of age, height or oesophageal inflammation[44].Oesophageal DI < 4.5 mm2/mmHg has been suggested as a predictor of the presence of grade II rings in children[44].The association between EndoFLIP findings, particularly DI, and the degree of EoE inflammation in paediatric is conflicting and is in contrast to adult studies which showed no correlation between reduced DI and the degree of oesophageal inflammation[40].This is likely to represent the small scales of paediatric studies and the difference in selection criteria.
Gastrooesophageal reflux disease
Limited data is available on the use of EndoFLIP for the assessment of patient with gastrooesophageal reflux disease(GORD) and is mostly from adult studies.In adults, there were contradicting results regarding DI of the gastrooesophageal junction (GOJ) in the context of GORD[47,48].In one study, GOJ DI was reported to be higher in patients with GORD compared to controls irrespective of the presence of distal oesophagitis, but the authors did not look for the presence of hiatal hernia[47].Hiatal hernia is an important factor that may independently affect GOJ morphological studies, although in a separate study, Lottrupet al[49] have reported on the usefulness of EndoFLIP in identification and assessment of hiatal hernia.In another study, the authors did not find a statistically significant difference in the measurements of GOJ DI between patients with GORD and healthy volunteers but they did acknowledge the presence of many independent confounding factors (e.g.,obesity)[48].
EndoFLIP can provide a useful tool in the assessment of fundoplication and can be used intraoperatively during antireflux surgery.Using FLIP intraoperatively can provide a real time measurement of GOJ DI and diameter, although direct clinical outcome data is lacking, proxy data appeared to support the clinical outcome associated with certain EndoFLIP values[16,50,51].
Oesophageal atresia and oesophageal strictures
EndoFLIP offers a promising tool to study the oesophageal morphology post oesophageal atresia repair.One small paediatric study has reported on the use of EndoFLIP to assess the geometry of OGJ, oesophageal body distensibility and anastomotic strictures.They have reported a DI within published normal values for the oesophageal body and the OGJ,while their data on FLIP measurements of the anastomosis site were combined with other diagnostic modalities to help guide therapeutic and prognostic directions[52].Figure 2C is a child with repaired oesophageal atresia showed a reduced diameter at the site of anastomotic scare and a dilated oesophageal segment above.
Another retrospective paediatric study has reported on the use of EndoFLIP and the FLIP dilatation catheter EsoFLIP in assessment and management of different types of oesophageal strictures in children.They reported a potential clinical benefit of reduction in procedural time and achieving a larger diameter changes post dilatation[53].Both studies recruited a small number of children in a retrospective manner affecting their wider applicability.With such limited data, the use of EndoFLIP in the assessment of children with repaired oesophageal atresia and/or oesophageal strictures is to be explored.
Uses of EndoFLIP in the pylorus
In contrast to LOS, the pyloric sphincter did not receive the same level of diagnostic scrutiny.Although the pylorus plays a vital role in regulating gastric emptying (GE), the association between symptom severity and measured GE remains poor[54].In part, this can be explained by the complex role of the pylorus sphincter compared to other GI sphincters.Detailed assessment of post prandial period reported that GE occurred during the relaxation of the pylorus and was driven primarily by the pressure generated by gastric tone and content (pressure pump) rather than the effect of antral contraction wave (peristalsis pump)[55].On the other hand, contraction of the pylorus in the face of gastric peristalsis wave will lead to bolus retention and gastric content mixing.However, the pylorus pressure measurements did not differ in patients with normal or delayed GE[54,56].
In adults, geometric assessment of the pylorus by EndoFLIP has been widely studied in patients with gastroparesis or with symptoms suggestive of gastroparesis (such as nausea and vomiting)[57-59].Pylorus DI has been found to correlate with GE and gastroparesis symptoms, a promising finding to identify a group of patients who may respond to targeted pylorus therapy[58,59].
EndoFLIP catheter is usually insertedper osunder direct endoscopic vision and prior to endoscopic intubation of the pylorus.The effect of anaesthesia and sedation on the EndoFLIP findings are yet to be studied.Pylorus geometric measurements are often taken after the EndoFLIP balloon is filled with a predetermined volume of 20, 30, 40 and 50 mL.Pylorus DI was significantly lower in patients with gastroparesis compared to healthy volunteers, but there was no difference in DI between diabetic gastroparesis and other forms of the disorder[19].Early satiety and postprandial fullness were inversely correlated to pylorus CSA and diameter, this has been the only clear association between a diagnostic investigation and symptoms of gastroparesis, in contrast to other investigative modalities such as GE scintigraphy and manometry[58].Although the authors were unable to offer a concrete explanation of this association, and the absence of correlation with any EndoFLIP parameters and other gastroparesis symptoms, it is possible that the pylorus opening diameter rather than distensibility or compliance is the driving force behind these two symptoms but further research is needed to study this hypothesis.
EndoFLIP has also been used to predict clinical response to intra pylorus Botulinum Toxin injection[60].Patients with gastroparesis and an abnormal pylorus EndoFLIP measurements appear to show sustained symptom improvement at 3 mo compared to gastroparesis patients with normal FLIP parameters[60].A similar clinical response was also observed post pylorus dilatation and gastric POEM guided by EndoFLIP findings in patients with therapy refractory gastroparesis[59,61].
In paediatrics, Hirschet al[62] have reported in a retrospective observational study in children with nausea and vomiting that the pylorus distensibility were lower in children with delayed GE compared to the normal GE group but the differences were not statistically significant.This is likely to be secondary to small sample size and patient selection.In the same study, EndoFLIP did not predict the symptomatic response to intra pylorus Botulinum Toxin injection[62].A likely explanation is the selection criteria for included children as 44% had normal GE and previous adult studies did not show correlation between EndoFLIP and the reported symptoms of nausea and vomiting.
We have recently published our experience in using pylorus EndoFLIP in children with neuromuscular disorders and the response to Botulinum Toxin injection[63].In our cohort, children with symptoms suggestive of gastroparesis had abnormal EndoFLIP measurements according to both adults and previous paediatric studies.We reported good symptoms improvement, weight gain and feed tolerance after Botulinum Toxin injections, a response that had been replicated after repeat injections 6-9 mo later.We did observe a trend of improvement in EndoFLIP measurements even though the FLIP remeasurements were obtained due to symptoms recurrence.Our sample size was small and we did not measure GE due to the comorbidities present in our studied group[63].Figure 4 is from a child with gastroparesis showed reduced pylorus distensibility.EndoFLIP usage in the assessment of pylorus sphincter is increasing and appear to show promising diagnostic data, symptom correlation with GE and most importantly, it can identify a subset of patients who can response to targeted pylorus therapy.
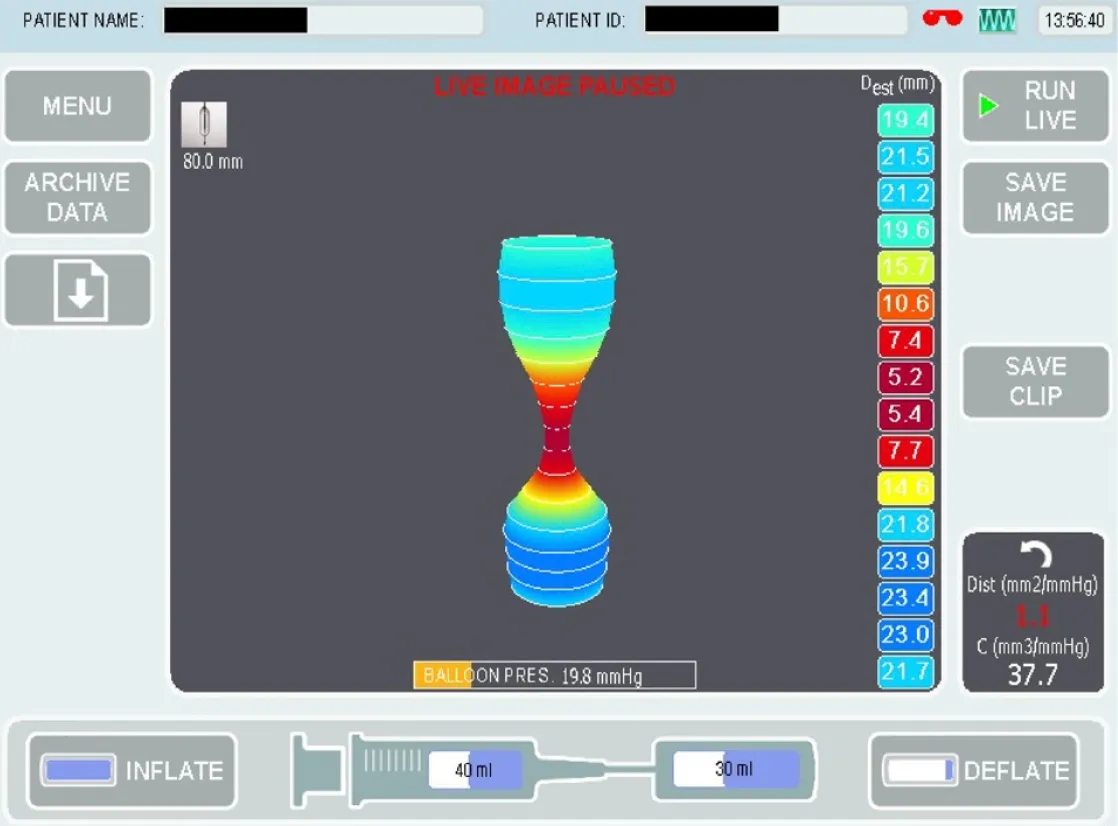
Figure 4 Endolumenal functional lumen imaging probe of the pylorus sphincter from a child with gastroparesis showing reduced pylorus distensibility.
Uses of EndoFLIP in the anal sphincter
There are very few studies reporting on the use of EndoFLIP in assessment of the geometry of the anal canal, all were from adult patient and healthy volunteers[64-66].To date, there is no published paediatric study.Although there was a general harmony on the methods used in all published studies, there were no agreement on the relevant FLIP measurements or their applicability to clinical practice.All published studies have reported a higher anal distensibility in patients with faecal incontinence compared to healthy volunteers, however, the clinical utility of such a finding is yet to be explored.
CONCLUSION
EndoFLIP is a promising tool to further improve our ability to understand the motility function of the GI tract.By providing a detailed geometric assessment to the oesophageal lumen and various sphincters in the GI tract, EndoFLIP findings are complementary to the existing GI motility investigations, but the data does not support the use of EndoFLIP to replace standard GI motility investigations.EndoFLIP has been successfully used to aid diagnosis and to guide therapeutic interventions.EndoFLIP studies in paediatrics are lagging behind adult studies but they have replicated some of adult results.The absence of normative values for children may limit the wider uptake within paediatrics but with the increase in complexity and prevalence of paediatric GI motility disorders, EndoFLIP can provide a valuable diagnostic and prognostic data.
FOOTNOTES
Author contributions:White E wrote the draft; Mutalib M wrote and edited the manuscript; and all authors approved the final version of the manuscript.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:United Kingdom
ORCID number:Mohamed Mutalib 0000-0001-8869-9466.
S-Editor:Wang JJ
L-Editor:A
P-Editor:Zhang XD
杂志排行
World Journal of Clinical Pediatrics的其它文章
- Transient hyperphosphatasemia in a toddler with COVID-19 infection: A case report and literature review
- Radiation dose analysis of computed tomography coronary angiography in Children with Kawasaki disease
- Safety and efficacy of intravitreal anti vascular endothelial growth factor for severe posterior retinopathy of prematurity with flat fibrovascular proliferation
- Accidental ingestion of foreign bodies/harmful materials in children from Bahrain: A retrospective cohort study
- Gastrointestinal and nutritional care in pediatric neuromuscular disorders
- Role of gastrointestinal health in managing children with autism spectrum disorder
