分类树模型的脑卒中后偏瘫患者心理状态与肢体功能的相关性
2023-10-18沈叶楠马敏李雯
沈叶楠,马敏,李雯
分类树模型的脑卒中后偏瘫患者心理状态与肢体功能的相关性
沈叶楠,马敏,李雯
浙江大学医学院附属第二医院临平院区神经内科,浙江杭州 311100
研究基于分类树模型的脑卒中后偏瘫患者心理状态与肢体功能的相关性及交互作用。选取2021年3月至2022年11月浙江大学医学院附属第二医院临平院区神经内科收治的120例脑卒中后偏瘫患者,心理状态评估量表(mental status scale in non-psychiatric settings,MSSNS)评估心理状态、Fugl-Meyer评定量表(Fugl-Meyer assessment scale,FMA)评估肢体功能;应用Pearson相关性分析法,评估分析脑卒中后偏瘫患者心理状态与肢体功能的相关性。收集入组患者的临床资料,采用多因素Logistic回归分析法明确危险因素,构建分类树模型分析脑卒中后偏瘫患者肢体功能影响因素之间的交互作用。脑卒中后偏瘫患者MSSNS评分、FMA评分分别为(88.22±20.36)分和(73.62±15.25)分,Pearson相关性分析脑卒中后偏瘫患者MSSNS与FMA评分呈正相关(=0.463,<0.05)。Logistic多因素回归分析提示年龄≥65岁、MSSNS评分高、空腹血糖(fasting blood glucose,FBG)高影响脑卒中后偏瘫患者的肢体功能。构建的脑卒中后偏瘫患者肢体功能的分类树模型包括2层、5个节点、3个终末节点,共筛选出2个解释变量,分别为年龄≥65岁和MSSNS评分,该模型的Risk统计量为0.167,提示该模型拟合效果好;脑卒中后偏瘫患者严重肢体功能障碍的影响因素交互作用结果显示,年龄和MSSNS评分之间有正向相加交互作用、无相乘交互作用。脑卒中后偏瘫患者心理状态与肢体功能呈正相关,年龄、MSSNS评分、FBG是影响脑卒中后偏瘫患者肢体功能的危险因素,其中年龄与心理状态之间对脑卒中后偏瘫患者严重肢体功能障碍的影响具有正向相加交互作用。
脑卒中后偏瘫;肢体功能;心理状态;交互作用;分类树模型
脑卒中具有发病急骤、疾病进展快等特点,多发于中老年群体,相关数据显示,我国脑卒中患病率约为1114.8/10万,致残率高达80%以上[1-2]。多数脑卒中患者伴有偏瘫,通常表现为患侧肢体活动不利、肌张力高、感觉减退等,部分患者长期卧床会诱发压疮、感染等多种并发症,严重降低患者的生活质量[3-4]。随着现代生物–心理–社会医学模式的提出,探讨脑卒中后偏瘫患者心理状态与肢体功能的关系尤为关键。陈晓莹等[5]研究指出脑卒中后偏瘫患者的心理健康状况往往与生理症状存在双向影响。影响脑卒中后偏瘫患者肢体功能的影响因素众多,当两个或多个影响因素存在时,疾病的发生率与其单独作用所估计的发病率不同,而当两因素引起的效应互不独立,且一个因素对另一因素有效应修饰作用时,即表明两因素存在相加交互作用,目前研究主要通过模型化的统计学方法探究不同因素间的交互作用[6-7]。分类树模型利用分割的方法深入数据局部,简洁、直观地展示影响因素之间的层次关系,因多数疾病的心理、生理协同发生机制尚不明确,目前的研究较少分析生理与心理影响因素之间的交互作用[8]。基于此,本研究旨在探讨基于分类树模型的脑卒中后偏瘫患者心理状态与肢体功能的相关性及交互作用,现报道如下。
1 资料与方法
1.1 一般资料
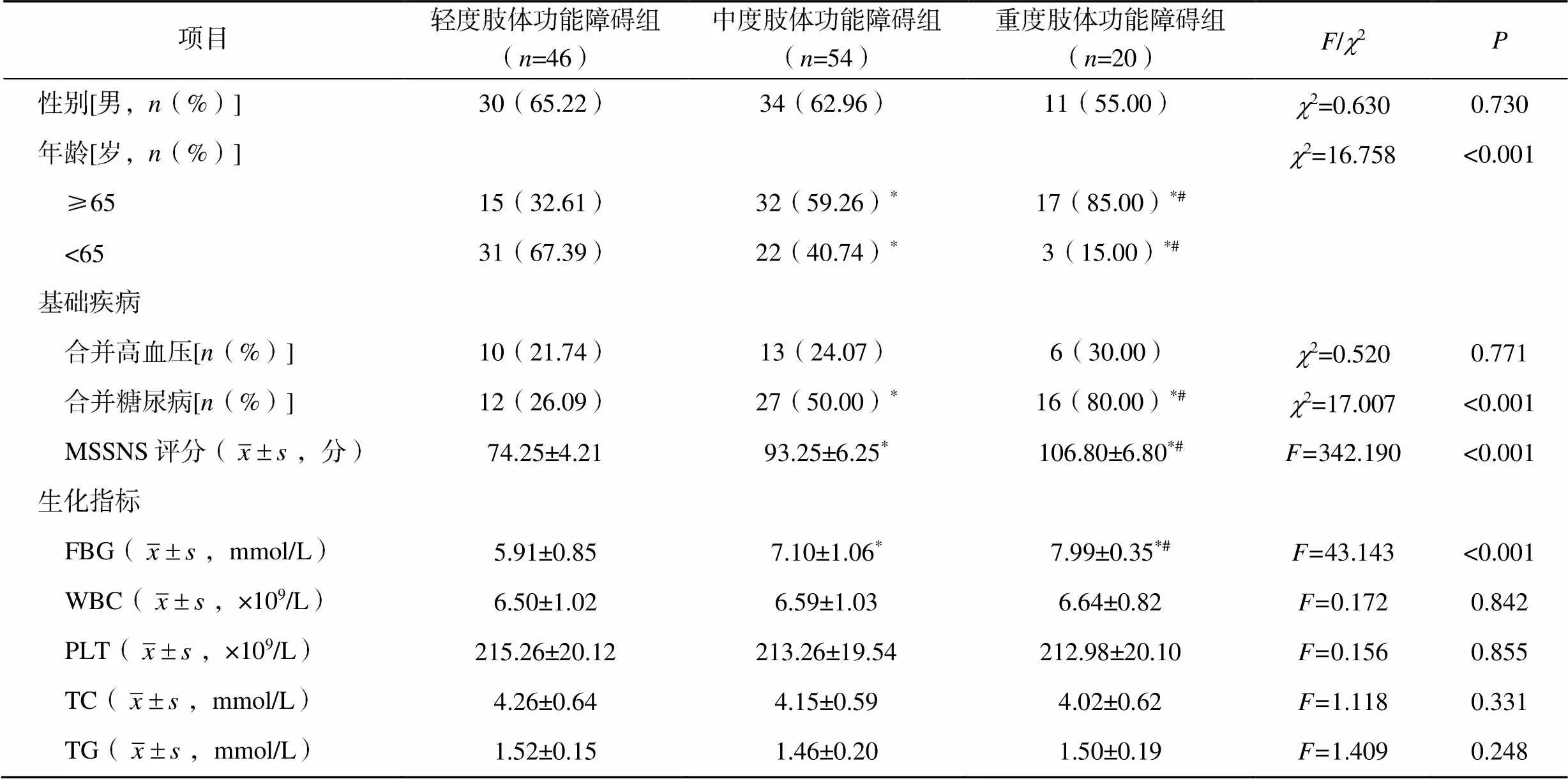
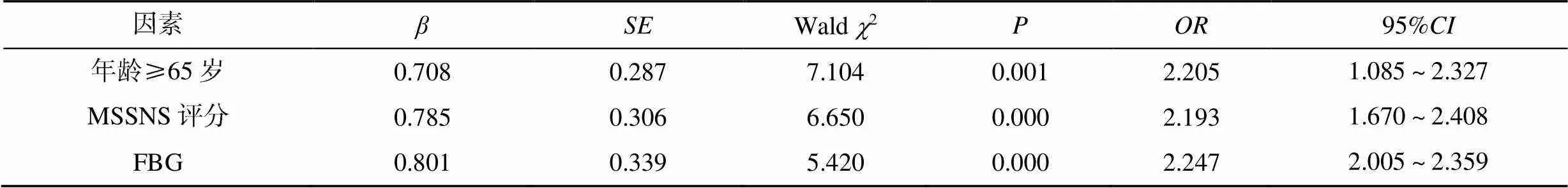
选取2021年3月至2022年11月浙江大学医学院附属第二医院临平院区神经内科收治的120例脑卒中后偏瘫患者,其中男性75例,女性45例,年龄45~74岁,平均(62.25±10.25)岁。依据Fugl-Meyer评定量表(Fugl-Meyer assessment scale,FMA)评分,将患者分为轻度肢体功能障碍组(FMA评分≥95分)、中度肢体功能障碍组(85分 1.2.1 临床资料收集 收集入组患者的临床资料,包括性别、年龄、基础疾病(高血压、糖尿病)、心理状态评估量表(mental status scale in non-psychiatric settings,MSSNS)评分[10]、生化指标[空腹血糖(fasting blood glucose,FBG)、白细胞计数(white blood cell count,WBC)、血小板计数(platelet count,PLT)、总胆固醇(total cholesterol,TC)、三酰甘油(triglyceride,TG)]。 1.2.2 心理状态、肢体功能评估 心理状态采用MSSNS评估,分数与患者心理状态成正比;肢体功能采用FMA评估,分数与患者肢体功能成正比[11]。 入组患者的MSSNS、FMA评分分别为(88.22±20.36)分和(73.62±15.25)分,Pearson相关性分析结果显示,脑卒中后偏瘫患者的MSSNS与FMA评分呈正相关(=0.463,<0.05),即脑卒中偏瘫患者的心理状态越好,肢体功能越好,见图1。 图1 脑卒中后偏瘫患者MSSNS与FMA评分的相关性 与轻度肢体功能障碍组比较,中度、重度肢体功能障碍组偏瘫患者的年龄≥65岁比例、合并糖尿病比例、MSSNS评分、FBG水平均较高,且重度肢体功能障碍组偏瘫患者的上述指标均高于中度肢体功能障碍组(<0.05),见表1。 将上述差异具有统计学意义的指标(年龄≥65岁=1、年龄<65岁=0,糖尿病=1、无糖尿病=0,MSSNS评分、FBG水平)作为自变量(),脑卒中后偏瘫患者肢体功能作为因变量(重度肢体功能障碍=1,轻中度肢体功能障碍=0)进行多因素Logistic回归分析,结果显示年龄≥65岁、MSSNS评分高、FBG水平高是影响脑卒中后偏瘫患者肢体功能障碍的独立危险因素,见表2。 根据多因素Logistic回归分析结果,将<0.05的影响因素纳入分类树模型,构建的脑卒中后偏瘫患者肢体功能的分类树模型包括2层、5个节点、3个终末节点,共筛选出2个解释变量,分别为年龄≥65岁、MSSNS评分,该模型的Risk统计量为0.167,提示该模型拟合效果好;脑卒中后偏瘫患者严重肢体功能障碍的影响因素交互作用结果显示,年龄和MSSNS评分之间有正向相加交互作用、无相乘交互作用,见图2、表3。 脑部血管阻塞或破裂导致血液不能流入大脑而引起的脑组织损伤即为脑卒中,该病多发于中老年群体,但随着人们饮食结构的变化,脑卒中发病人群日趋年轻化[12-13]。多数脑卒中患者经及时溶栓治疗后仍出现不同程度的功能障碍[14-15]。脑卒中后偏瘫患者存在不同程度的肢体功能障碍,患者的身心负担、家庭经济负担较重,极大可能产生焦虑、抑郁和厌世等不良情绪,而心理状态易影响患者治疗主动性,与远期预后相关[16]。了解脑卒中后偏瘫患者的心理状态与肢体功能的关系有助于临床更好地制订后续治疗计划,改善患者预后。本研究分别采用MSSNS、FMA评分评估脑卒中后偏瘫患者的心理状态和肢体功能,Pearson相关性分析显示,脑卒中后偏瘫患者的MSSNS与FMA评分呈正相关,提示患者的心理状态与生理状态密切相关。 表1 脑卒中后肢体功能障碍不同程度偏瘫患者的临床资料比较 注:与轻度肢体功能障碍组比较,*<0.05;与中度肢体功能障碍组比较,#<0.05 表2 影响脑卒中后偏瘫患者肢体功能的因素 图2 脑卒中后偏瘫患者肢体功能的分类树模型 表3 年龄和MSSNS评分的交互作用检验 脑卒中后偏瘫患者因肢体功能不同程度受损,后续可能完全丧失自主生活能力,严重降低患者及家属的生活质量[17]。本研究通过比较轻度、中度、重度肢体功能障碍的脑卒中后偏瘫患者的临床资料发现,与轻度肢体功能障碍组比较,中度、重度肢体功能障碍组偏瘫患者的年龄≥65岁比例、合并糖尿病比例、MSSNS评分、FBG水平均较高,经多因素Logistic回归分析显示,年龄、MSSNS评分和FBG水平是脑卒中后偏瘫患者肢体功能障碍的独立危险因素。机体各项生理功能随年龄增长逐渐衰弱,老年群体血管内纤维蛋白减少、胶原组织萎缩,血管结构发生变化后血管脆性增加,更易在较小外力作用下发生破裂出血,故老年脑卒中偏瘫患者发生重度肢体功能障碍风险较大[18];Maeshima等[19]研究发现,脑卒中后偏瘫患者的焦虑、抑郁程度较未偏瘫者更重。本研究结果显示脑卒中后重度肢体功能障碍偏瘫患者的MSSNS评分最高,提示脑卒中后偏瘫患者的心理状态与生理状态关系密切,后续研究可基于此制定相关措施对脑卒中患者实施早期干预以降低偏瘫发生风险;脑卒中后偏瘫患者FBG水平高可归因于高血糖介导机体炎症反应,诱发广泛性微血管内皮损伤后加重脑组织血管源性水肿程度,加重神经细胞损伤程度,神经细胞支配的躯体功能异常程度,即肢体功能障碍程度随之加重[20-21]。 目前关于疾病影响因素交互作用的研究常采用分类树模型;相较于传统Logistic回归模型,分类树模型很大程度上可减少研究的工作量,在对影响因素相互间交互作用识别方面也更有优势[22-23]。本研究采用构建分类树模型的方法分析脑卒中后偏瘫患者肢体功能影响因素之间的交互作用,分类树模型共筛选出2个解释变量,分别为年龄≥65岁和高MSSNS评分。年龄≥65岁且心理状态差的脑卒中患者发生重度肢体功能障碍的可能性更大,密切监测血糖及其他各项生化指标,可降低病情恶化、减少重度肢体功能障碍发生风险。蒋妮等[24-25]研究认为,分类树模型仍存在一定局限性,如分类树模型在小样本的稳健性欠佳、对自变量单独效应的定量解释不如Logistic回归模型。后续可进一步优化分类树模型数据处理模式,使结果更加准确、合理。 综上,年龄≥65岁、高MSSNS评分和高FBG水平是影响脑卒中后偏瘫患者肢体功能障碍的独立危险因素,且年龄与心理状态对脑卒中后偏瘫患者严重肢体功能障碍的影响具有正向相加交互作用。 [1] TETSUKA S, OGAWA T, HASHIMOTO R, et al. Clinical features, pathogenesis, and management of stroke-like episodes due to melas[J]. Metab Brain Dis, 2021, 36(8): 2181–2193. [2] 刘美快, 徐乐义, 李海燕, 等. 镜像疗法对脑卒中患者运动功能和平衡功能以及胫骨前肌形态结构的影响[J]. 中华物理医学与康复杂志, 2020, 42(5): 419–423. [3] KENT D M, SAVER J L, KASNER S E, et al. Heterogeneity of treatment effects in an analysis of pooled individual patient data from randomized trials of device closure of patent foramen ovale after stroke[J]. JAMA, 2021, 326(22): 2277–2286. [4] 陈煌, 谢红珍, 黎蔚华, 等. 脑卒中肢体功能障碍患者早期康复护理的最佳证据总结[J]. 解放军护理杂志, 2020, 37(6): 6–10. [5] 陈晓莹, 尹祚平, 朱列和, 等. 脑卒中后抑郁患者的心理状况及其与认知功能的相关性[J]. 海南医学, 2020, 31(3): 306–308. [6] DERAKHSHANFAR M, RAJI P, BAGHERI H, et al. Sensory interventions on motor function, activities of daily living, and spasticity of the upper limb in people with stroke: A randomized clinical trial[J]. J Hand Ther, 2021, 34(4): 515–520. [7] CHEN Y H, CHEN C L, HUANG Y Z, et al. Augmented efficacy of intermittent theta burst stimulation on the virtual reality-based cycling training for upper limb function in patients with stroke: A double-blinded, randomized controlled trial[J]. J Neuroeng Rehabil, 2021, 18(1): 91. [8] 何纲, 张志侨, 叶一农, 等. 慢加急性肝衰竭患者发生肝性脑病高危人群的分类树模型和简易风险评估[J]. 中国热带医学, 2020, 20(3): 275–280. [9] 中华医学会神经病学分会, 中华医学会神经病学分会脑血管病学组. 中国急性缺血性脑卒中诊治指南2018[J]. 中华神经科杂志, 2018, 51(9): 666–682. [10] MA Y, KAMALIBAIKE M, XIN C, et al. Effect of the intensive psychological nursing on adverse mood and quality of life in patients with cervical cancer[J]. Am J Transl Res, 2021, 13(8): 9633–9638. [11] CECCHI F, CARRABBA C, BERTOLUCCI F, et al. Transcultural translation and validation of Fugl-Meyer assessment to Italian[J]. Disabil Rehabil, 2021, 43(25): 3717–3722. [12] 王思迅, 陆东, 李婕, 等. 应用CT脑CTP联合头颈CTA诊断缺血性脑卒中的临床价值[J]. 中国CT和MRI杂志, 2022, 20(9): 11–12. [13] MORONE G, MARTINO CINNERA A, PAOLUCCI T, et al. Clinical features of fallers among inpatient subacute stroke: An observational cohort study[J]. Neurol Sci, 2020, 41(9): 2599–2604. [14] SALERNO A, STRAMBO D, NANNONI S, et al. Patterns of ischemic posterior circulation strokes: A clinical, anatomical, and radiological review[J] Int J Stroke, 2022, 17(7): 714–722. [15] 崔林华, 齐丛会, 邢潇, 等. 五线七针疗法治疗脑卒中后肢体功能障碍临床观察[J]. 中华中医药学刊, 2020, 38(12): 237–240. [16] 朱倩. 系统化功能训练治疗老年缺血性脑卒中患者的疗效观察[J]. 中华物理医学与康复杂志, 2020, 42(6): 538–540. [17] GUEYE T, DEDKOVA M, ROGALEWICZ V, et al. Early post-stroke rehabilitation for upper limb motor function using virtual reality and exoskeleton: Equally efficient in older patients[J]. Neurol Neurochir Pol, 2021, 55(1): 91–96. [18] LIU X, YU H J, GAO Y, et al. Combined association of multiple chronic diseases and social isolation with the functional disability after stroke in elderly patients: A multicenter cross-sectional study in China[J]. BMC Geriatr, 2021, 21(1): 495. [19] MAESHIMA S, OKAMOTO S, MIZUNO S, et al. Predicting walking ability in hemiplegic patients with putaminal hemorrhage: An observational study in a rehabilitation hospital[J]. Eur J Phys Rehabil Med, 2021, 57(3): 321–326. [20] 韩啸, 赵越, 尤玉青, 等. 2型糖尿病伴高尿酸患者脑卒中风险及其危险因素[J]. 医学研究杂志, 2020, 49(10): 115–119. [21] MADSEN T E, LONG D L, CARSON A P, et al. Sex and race differences in the risk of ischemic stroke associated with fasting blood glucose in regards[J]. Neurology, 2021, 97(7): 684–694. [22] IMURA T, IWAMOTO Y, INAGAWA T, et al. Decision tree algorithm identifies stroke patients likely discharge home after rehabilitation using functional and environmental predictors[J]. J Stroke Cerebrovasc Dis, 2021, 30(4): 105636. [23] LYASHEVSKA O, MALONE F, MACCARTHY E, et al. Class imbalance in gradient boosting classification algorithms: Application to experimental stroke data[J]. Stat Methods Med Res, 2021, 30(3): 916–925. [24] 蒋妮, 程港, 贺思敏, 等. 基于决策树与多元线性回归模型的出生体重影响因素分析[J]. 中国卫生统计, 2022, 39(2): 202–206. [25] SIRIOPOL D, POPA R, MIHAILA M, et al. Application of survival classification and regression tree analysis for identification of subgroups of risk in patients with heart failure and reduced left ventricular ejection fraction[J]. Int J Cardiovasc Imaging, 2021, 37(6): 1853–1861. Correlation between mental status and limb function of hemiplegic patients after stroke based on classification tree model Department of Neurology, Linping District, the Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou 311100, Zhejiang, China To study the correlation and interaction between mental status and limb function in patients with hemiplegia after stroke based on classification tree model.A total of 120 patients with post-stroke hemiplegia admitted to the Department of Neurology, Linping District, the Second Affiliated Hospital of Zhejiang University School of Medicine from March 2021 to November 2022 were selected, mental status scale in non-psychiatric settings (MSSNS) was used to assess the mental status of the patients, and the Fugl-Meyer assessment scale (FMA) was used to assess the limb function of the patients, Pearson correlation analysis was used to analyze the correlation between mental status and limb function in patients with hemiplegia after stroke. The clinical data of enrolled patients were collected, and the risk factors affecting the limb function of poststroke patients with hemiplegia were determined by multivariate Logistic regression analysis. The classification tree model was built to analyze the interaction between the factors affecting the limb function of poststroke patients with hemiplegia.The MSSNS score and FMA score of patients with hemiplegia after stroke were (88.22±20.36) points and (73.62±15.25) points respectively, Pearson correlation analysis showed that there was a significant positive correlation between MSSNS score and FMA score in patients with hemiplegia after stroke (=0.463,<0.05). Multivariate Logistic regression analysis showed that age ≥65 years old, high MSSNS score and high fasting blood glucose (FBG) level were independent risk factors for limb dysfunction in patients with hemiplegia after stroke. The classification tree model of limb function in patients with hemiplegia after stroke consists of 2 layers, 5 nodes and 3 end nodes. Two explanatory variables are screened out, which are age ≥65 years old, MSSNS score, the Risk statistic of the model is 0.167, which indicates that the model has good fitting effect. The results of the interaction of factors influencing severe limb dysfunction in patients with hemiplegia after stroke showed that there was a positive additive interaction between age and MSSNS score, but no multiplicative interaction.There was a positive correlation between mental status and limb function in patients with hemiplegia after stroke, age, MSSNS score and FBG were risk factors affecting the limb function of poststroke patients with hemiplegia, and there was a positive plus interaction between age and mental status on the influence of severe limb dysfunction in poststroke patients with hemiplegia. Hemiplegia after stroke; Limb function; Mental status; Interaction; Classification tree model R473 A 10.3969/j.issn.1673-9701.2023.27.016 沈叶楠,电子信箱:2383316579@qq.com (2022–12–16) (2023–08–25)1.2 方法
1.3 统计学方法

2 结果
2.1 脑卒中后偏瘫患者心理状态与肢体功能的相关性

2.2 脑卒中后肢体功能障碍不同程度偏瘫患者的临床资料比较
2.3 影响脑卒中后偏瘫患者肢体功能的因素
2.4 脑卒中后偏瘫患者肢体功能影响因素之间的交互作用
3 讨论