AGE预测2型糖尿病患者肌少症发生风险
2023-09-28黄慧静曹永红洪琼邹玲玲戴武
黄慧静,曹永红,洪琼,邹玲玲,戴武
AGE预测2型糖尿病患者肌少症发生风险
黄慧静1,2,曹永红1,洪琼1,邹玲玲1,戴武1,2
1.安徽医科大学附属合肥医院(合肥市第二人民医院)内分泌科,安徽合肥 230011;2.安徽医科大学第五临床医学院,安徽合肥 230032
分析2型糖尿病(type 2 diabetes mellitus,T2DM)患者发生肌少症的危险因素,建立列线图预测模型探讨糖基化终末产物(advanced glycation end product,AGE)预测T2DM患者肌少症的患病风险。选取2021年10月至2022年10月于合肥市第二人民医院住院的T2DM患者180例为研究对象,根据是否合并肌少症将其分为对照组(=146)和肌少症组(=34)。比较两组患者的一般资料,采用Logistic回归分析探讨T2DM患者发生肌少症的危险因素,并建立列线图模型。两组患者的年龄、病程、AGE、肌力、起立试验、四肢骨骼肌质量指数(appendicular skeletal muscle mass index,ASMI)、体质量指数(body mass index,BMI)、糖化血红蛋白、尿白蛋白/肌酐比值比较差异均有统计学意义(<0.05),多因素回归分析结果显示BMI、肌力、AGE均是T2DM患者发生肌少症的独立危险因素(<0.05);以BMI、肌力、AGE建立预测模型,经验证该模型校准度良好,具有良好的区分度。绘制受试者操作特征曲线发现其预测T2DM患者发生肌少症的曲线下面积为0.933,有良好的预测价值;校正曲线及决策曲线分析评估结果显示该模型具有更高的净收益和更好的临床应用价值。AGE是T2DM患者发生肌少症的独立危险因素,对T2DM患者的肌少症诊断具有一定的预测作用。
2型糖尿病;糖基化终末产物;肌少症;列线图
肌少症与老年人的多种不良健康结局相关[1-2]。2型糖尿病(type 2 diabetes mellitus,T2DM)患者肌少症的发病率较普通人群明显增加,甚至认为肌少症是糖尿病新出现的并发症[3-4]。糖基化终末产物(advanced glycation end product,AGE)是指在非酶促条件下,蛋白质、氨基酸、脂类或核酸等大分子物质的游离氨基与还原糖的醛基经过缩合、重排、裂解、氧化修饰后产生的一组稳定的终末产物。AGE的蓄积可消耗机体抗氧化机制,导致β细胞损伤、胰岛素抵抗及慢性炎症,从而与糖尿病及其并发症的发生、发展密切相关。AGE的积累与T2DM患者肌少症的相关性研究还在初步阶段。因此,本研究拟探究AGE与T2DM患者肌少症有无相关性,并建立列线图模型评估AGE对肌少症的预测价值。
1 资料与方法
1.1 研究对象
选取2021年10月至2022年10月于合肥市第二人民医院住院的T2DM患者180例为研究对象。纳入标准:①诊断明确的2型糖尿病患者;②入院前3个月有稳定的降糖方案;③年龄50~80岁。排除标准:①妊娠期和哺乳期女性;②合并心、脑、肾、肝等脏器严重疾病;③合并精神疾病或躯体残疾无法配合检查者;④怀疑或确有酒精、药物滥用史者;⑤糖尿病急性并发症者;⑥合并肿瘤、甲状腺疾病、感染、自身免疫性疾病、影响体内激素水平的相关疾病;⑦有家族遗传性疾病;⑧有减肥药、甲状腺激素、生长激素、糖皮质激素、性激素等药物应用史;⑨3个月内服用维生素D、双膦酸盐等影响骨代谢的药物;⑩合并慢性呼吸道疾病;⑪被检查者前臂内侧皮肤有瘢痕、苔藓样硬化斑、传染性皮肤疾病者;⑫合并帕金森病、运动神经元病、脑卒中后遗症、严重认知功能障碍、重度骨关节炎、类风湿关节炎、重度骨质疏松、营养不良及长期卧床等影响躯体功能者。根据是否合并肌少症将纳入患者分为对照组(=146)和肌少症组(=34)。本研究经合肥市第二人民医院伦理委员会批准(伦理审批号:2022yzd001),所有患者均签署知情同意书。
1.2 研究方法
1.2.1 基本信息 身高、体质量指数(body mass index,BMI)、收缩压(systolic blood pressure,SBP)、舒张压(diastolic blood pressure,DBP)、糖尿病病程。
1.2.2 实验室指标 禁食8h后,次日凌晨空腹采集患者的静脉血,采用全自动生化分析仪测定相关指标:空腹血糖(fasting plasma glucose,FBG)、血钙、磷、三酰甘油(triglyceride,TG)、总胆固醇(total cholesterol,TC)、高密度脂蛋白(high density lipoprotein,HDL)、低密度脂蛋白(low density lipoprotein,LDL)、糖化血红蛋白(glycated hemoglobin,HbA1c)、空腹C肽、尿白蛋白/肌酐比值(albumin/ creatinine ratio,ACR)等生化免疫指标。
1.2.3 骨骼肌及躯体功能 通过GE lunar双能X线骨密度测量仪测量四肢骨骼肌质量后计算四肢骨骼肌质量指数(appendicular skeletal muscle mass index,ASMI)。使用弹簧握力器测定肌力:站立位伸肘测量握力,如果老年人不能独自站立,则选用坐位测量,用优势手或两只手分别最大力量等距收缩,至少测量2次,选取最大读数。躯体功能:受试者在床边用身体能承受的最快速度连续5次起立,记录时间,5次起立试验时间≥12s则反映躯体功能下降。
1.2.4 AGE检测 采用AGE Pro型糖基化终末产物无创检测仪检测受试者皮肤AGE水平,在前臂腹侧连续测量3次取平均值。
1.2.5 肌少症诊断标准 肌少症诊断符合2019亚洲肌少症诊断共识[5]。肌少症诊断:①肌肉量减少:男性ASMI<7.0kg/m2、女性ASMI<5.4kg/m2;②肌肉力量降低:男性握力<28kg、女性握力<18kg;③起立实验阳性。以上①②项为诊断必备条件,③为诊断辅助条件。
1.3 统计学方法
2 结果
2.1 两组患者的一般资料比较
两组患者的年龄、病程、AGE、肌力、起立试验、ASMI、BMI、HbA1c、ACR比较差异均有统计学意义(<0.05),见表1。
2.2 影响T2DM患者发生肌少症的多因素回归分析
多因素回归分析结果显示BMI、肌力、AGE均是T2DM患者发生肌少症的独立危险因素(<0.05),见表2。

表1 两组患者的一般资料比较
注:1mmHg=0.133kPa
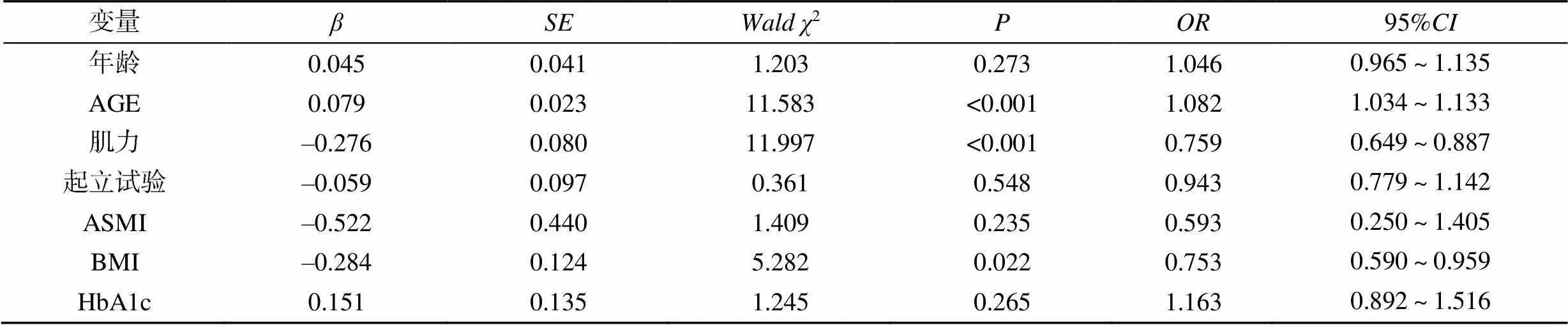
表2 影响T2DM患者发生肌少症的多因素回归分析

图1 预测模型的列线图
2.3 建立列线图模型Model 1预测T2DM患者发生肌少症的风险
根据上述筛选出的独立危险因素构建T2DM患者肌少症发病风险的预测模型,见图1;以收集数据的第一个样本AGE=86.8、BMI=19.10kg/m2、肌力=28.8kg为例,预测其对应肌少症的发生概率为22.8%。使用Bootstrap内部验证法对列线图模型进行验证,校准曲线和Y=X直线相近模型校准度良好,列线图模型的C指数为0.933,校正后的C指数为0.927,说明模型拟合较好,见图2。绘制ROC曲线发现列线图模型预测T2DM患者发生肌少症的AUC为0.933(95%:0.897~0.970),有良好预测价值,见图3。临床获益DCA评估结果显示多因素预测模型列线图具有更高的净收益和更好的临床应用价值,见图4。
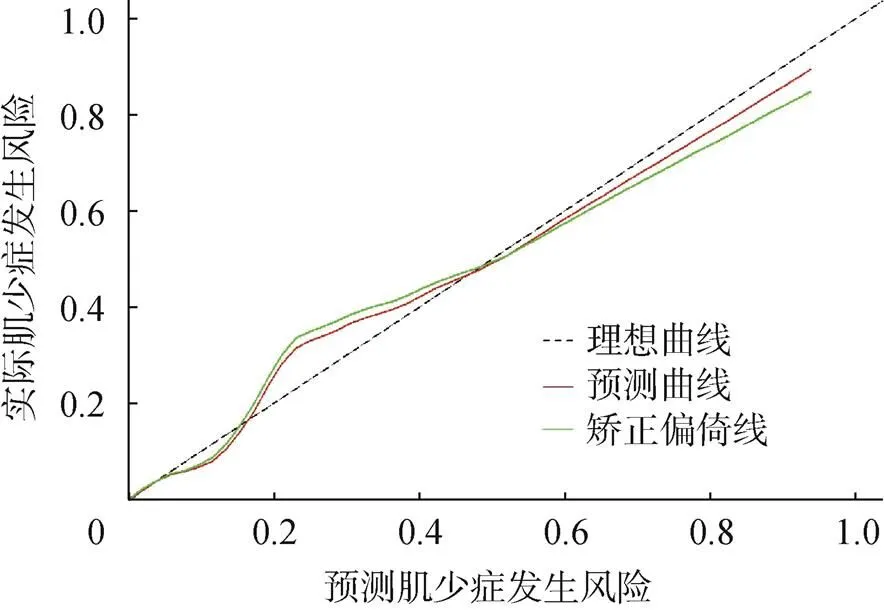
图2 预测T2DM患者发生肌少症列线图的校准曲线

图3 预测T2DM患者发生肌少症列线图的ROC曲线

图4 预测T2DM患者发生肌少症列线图的决策曲线
3 讨论
肌少症近年来逐渐受到关注,糖尿病与其发生发展也有一定相关性。本研究结果显示肌少症患病率为18.9%,男性较女性略高,但差异无统计学意义。目前关于性别对肌少症的影响尚无定论,有研究发现男性或女性的肌少症患病率明显升高[6-7];但也有研究认为T2DM患者肌少症的发病率无性别差异[8]。针对性别对其的影响还需要更多的研究去探索。本研究中肌少症组患者年龄更大,肌力和ASMI更低。关于起立试验两组患者的平均时间均在正常范围内,但多因素回归分析显示没有显著相关性,关于肌少症患者躯体功能是否受损及受损程度如何,未来需要扩大样本量进一步探究。
既往研究发现HbA1c水平与肌肉质量受损[9]、肌肉力量[10]和身体表现[11]无关,本研究结果与上述研究一致。另外,本研究发现BMI与T2DM患者肌少症的发生相关,肌少症患者的BMI值更低,有研究表明随着BMI的增加,肌少症的患病率显著降低,提示低体质量的T2DM患者更易患肌少症,与Fukuoka等[12]研究一致。
AGE在糖尿病患者的各种组织中沉积,与慢性高血糖状态[13]、糖尿病慢性并发症[14]、糖尿病患者骨代谢[15]的发生发展有相关性。本研究发现肌少症组患者较对照组有更高的AGE积累,多因素回归分析显示AGE是T2DM患者肌少症发生的独立危险因素。既往研究发现肌肉量减少与随着年龄增长而积累的AGE相关,AGE可增加氧化应激和炎性细胞因子[16]。此外,AGE在老年人和啮齿动物衰老模型中诱导肌肉蛋白的交联和分解,通过多条信号通路诱导糖尿病小鼠骨骼肌萎缩和功能障碍,AGE在小鼠后肢肌肉中不断积累与其肌肉质量、肌肉耐力和再生能力的下降有关[17-18]。有报道称快缩肌纤维中的AGE积累与肌肉胶原蛋白交联,增加肌肉僵硬并降低肌肉收缩的强直力[19]。说明累积的AGE与T2DM患者的肌肉质量减少有关。
本研究构建一个可量化且简单的列线图来预测T2DM患者肌少症的发生风险。在内部验证之后,发现其具有高度的预测准确性,DCA也证明该模型具有较好的临床价值。此外,列线图因其容易获得的具体参数而在临床具有一定的实用价值,对临床评估患者肌少症患病风险具有简单直接的帮助,未来需要收集更多的数据来完善此列线图。
本研究具有一定局限性,首先是横断面设计,不能推断因果关系;第二,没有关于患者长期饮食运动的信息,不能忽视其对肌肉质量和力量的影响;第三,缺乏炎症相关指标的采集,不能评估炎症相关因素对肌少症的影响;最后,样本量不够大也是推广该结果的重要限制因素,需要后续扩大样本进行前瞻性研究探索AGE与肌少症之间的关系。
综上所述,AGE积累是T2DM患者发生肌少症的独立危险因素,结合AGE、BMI和肌力的多因素预测模型对T2DM患者肌少症的发生有很好的预测价值。
[1] MONTERO-ERRASQUÍN B, CRUZ-JENTOFT A J. The value of sarcopenia in the prevention of disability[J]. Med Clin (Barc), 2019, 153(6): 243–244.
[2] RIZZOLI R, REGINSTER J Y, ARNAL J F, et al. Quality of life in sarcopenia and frailty[J]. Calcif Tissue Int, 2013, 93(2): 101–120.
[3] YANG Q, ZHANG Y, ZENG Q, et al. Correlation between diabetic peripheral neuropathy and sarcopenia in patients with type 2 diabetes mellitus and diabetic foot disease: A cross-sectional study[J]. Diabetes Metab Syndr Obes, 2020, 13: 377–386.
[4] SINCLAIR A J, ABDELHAFIZ A H, RODRÍGUEZ- MAÑAS L. Frailty and sarcopenia - Newly emerging and high impact complications of diabetes[J]. J Diabetes Complications, 2017, 31(9): 1465–1473.
[5] CHEN L K, WOO J, ASSANTACHAI P, et al. Asian Working Group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment[J]. J Am Med Dir Assoc, 2020, 21(3): 300–307.
[6] SAZLINA S G, LEE P Y, CHAN Y M, et al. The prevalence and factors associated with sarcopenia among community living elderly with type 2 diabetes mellitus in primary care clinics in Malaysia[J]. PLoS One, 2020, 15(5): e0233299.
[7] IDA S, NAKAI M, ITO S, et al. Association between sarcopenia and mild cognitive impairment using the Japanese version of the SARC-F in elderly patients with diabetes[J]. J Am Med Dir Assoc, 2017, 18(9): 809.
[8] IDA S, KANEKO R, NAGATA H, et al. Association between sarcopenia and sleep disorder in older patients with diabetes[J]. Geriatr Gerontol Int, 2019, 19(5): 399–403.
[9] YOON J W, HA Y C, KIM K M, et al. Hyperglycemia is associated with impaired muscle quality in older men with diabetes: The Korean longitudinal study on health and aging[J]. Diabetes Metab J, 2016, 40(2): 140–614.
[10] LEENDERS M, VERDIJK L B, VAN DER HOEVEN L, et al. Patients with type 2 diabetes show a greater decline in muscle mass, muscle strength, and functional capacity with aging[J]. J Am Med Dir Assoc, 2013, 14(8): 585–592.
[11] KALYANI R R, METTER E J, EGAN J, et al. Hyperglycemia predicts persistently lower muscle strength with aging[J]. Diabetes Care, 2015, 38(1): 82–90.
[12] FUKUOKA Y, NARITA T, FUJITA H, et al. Importance of physical evaluation using skeletal muscle mass index and body fat percentage to prevent sarcopenia in elderly Japanese diabetes patients[J]. J Diabetes Investig, 2019, 10(2): 322–330.
[13] GENUTH S, SUN W, CLEARY P, et al. Glycation and carboxymethyllysine levels in skin collagen predict the risk of future 10-year progression of diabetic retinopathy and nephropathy in the diabetes control and complications trial and epidemiology of diabetes interventions and complications participants with type 1 diabetes[J]. Diabetes, 2005, 54(11): 3103–3111.
[14] YING L, SHEN Y, ZHANG Y, et al. Association of advanced glycation end products with diabetic retinopathy in type 2 diabetes mellitus[J]. Diabetes Res Clin Pract, 2021, 177: 108880.
[15] SANGUINETI R, PUDDU A, MACH F, et al. Advanced glycation end products play adverse proinflammatory activities in osteoporosis[J]. Mediators Inflamm, 2014, 2014: 975872.
[16] HAUS J M, CARRITHERS J A, TRAPPE S W, et al. Collagen, cross-linking, and advanced glycation end products in aging human skeletal muscle[J]. J Appl Physiol, 2007, 103(6): 2068–2076.
[17] SNOW L M, FUGERE N A, THOMPSON L V. Advanced glycation end-product accumulation and associated protein modification in type II skeletal muscle with aging[J]. J Gerontol A Biol Sci Med Sci, 2007, 62(11): 1204–1210.
[18] CHIU C Y, YANG R S, SHEU M L, et al. Advanced glycation end-products induce skeletal muscle atrophy and dysfunction in diabetic mice via a RAGE-mediated, AMPK-down-regulated, Akt pathway[J]. J Pathol, 2016, 238(3): 470–482.
[19] MORI H, KURODA A, ARAKI M, et al. Advanced glycation end-products are a risk for muscle weakness in Japanese patients with type 1 diabetes[J]. J Diabetes Investig, 2017, 8(3): 377–382.
AGE predict the risk of sarcopenia in type 2 diabetes mellitus patients
HUANG Huijing, CAO Yonghong, HONG Qiong, ZOU Lingling, DAI Wu
1.Department of Endocrinology, Hospital Affiliated to Anhui Medical University (The Second People’s Hospital of Hefei), Hefei 230011, Anhui, China; 2.The Fifth School of Clinical Medicine, Anhui Medical University, Hefei 230032, Anhui, China
To analyze the risk factors of sarcopenia in patients with type 2 diabetes mellitus (T2DM), and establish a nomogram prediction model to investigate advanced glycation end product (AGE) predicts the risk of sarcopenia in T2DM patients.A total of 180 T2DM patients hospitalized in the Second People’s Hospital of Hefei from October 2021 to October 2022 were selected as study objects, and divided into control group (=146) and sarcopenia group (=34) according to whether they were complicated with sarcopenia. The general data of the two groups were compared, and the risk factors of sarcopenia in T2DM patients were discussed by Logistic regression analysis, and a nomogram model was established.There were significant differences in age, course of disease, AGE, muscle strength, standing test, appendicular skeletal muscle mass index (ASMI), body mass index (BMI), glycated hemoglobin and urinary albumin/creatinine ratio between the two groups (<0.05). Multivariate regression analysis showed that BMI, muscle strength and AGE were independent risk factors for sarcopenia in T2DM patients (<0.05). The prediction model was established based on BMI, muscle strength and AGE, and it was proved that the model had good calibration and differentiation. Receiver operating characteristic curve was drawn, and area under the curve was 0.933 in predicting the occurrence of sarcopenia in T2DM patients, which had good predictive value. Calibration curve and decision curve-analysis (DCA) evaluation results showed that the model had higher net benefit and better clinical application value.AGE is an independent risk factor for sarcopenia in T2DM patients, and it can predict the diagnosis of sarcopenia in T2DM patients.
Type 2 diabetes mellitus; Advanced glycation end product; Sarcopenia; Nomogram
R587.1
A
10.3969/j.issn.1673-9701.2023.25.011
合肥市卫生健康应用医学研究项目(合卫科教〔2019〕172号);安徽医科大学校科研基金项目(2020xkj247);合肥市第二人民医院院级科研重点项目(2022yzd001)
戴武,电子信箱:daiwuhf@126.com
(2022–12–07)
(2023–08–08)