血维生素K2和IL-6水平与慢性肾脏病患者冠状动脉钙化的相关性研究
2023-09-15王牡丹周丽娜杨仲煌李恩慈梁世凯
王牡丹 周丽娜 杨仲煌 李恩慈 梁世凯


[摘要] 目的 探討血维生素K2和白细胞介素6(interleukin-6,IL-6)水平与慢性肾脏病(chronic kidney disease,CKD)患者冠状动脉钙化(coronary artery calcification,CAC)的相关性。方法 选取2019年1月至2022年6月温州市人民医院肾内科收治的CKD患者111例,采用酶联免疫吸附试验(enzyme linked immunosorbent assay,ELISA)检测血维生素K2和IL-6水平;通过Agatston评分评价CAC;分析维生素K2、IL-6与CAC的相关性。结果 CAC组的年龄、高敏C反应蛋白(hypersensitive-C-reactive-protein,hs-CRP)、血磷、甲状旁腺素(parathyroid hormone,PTH)、同型半胱氨酸(homocysteine,Hcy)、IL-6水平较非CAC组高,而估算肾小球滤过率(estimated glomerular filtration rate,eGFR)、维生素K2较非CAC组低;Logistic回归分析显示年龄、Hcy、IL-6是CAC独立危险因素(OR值分别为1.69、1.14及1.12,95%CI分别为1.237~2.181、1.005~1.623、1.014~1.328);eGFR、维生素K2为CAC的保护因素(OR值分别为0.328、0.243,95%CI分别为0.216~0.713、0.076~0.651);重度CAC组维生素K2较轻度CAC组降低,IL-6则较轻度CAC组、中度CAC组升高(F值分别为5.70、6.13,P<0.05)。结论 高龄、高Hcy、高IL-6水平是CAC的独立危险因素,eGFR和维生素K2是CAC的保护因素。
[关键词] 维生素K2;白细胞介素6;慢性肾脏病;冠状动脉钙化
[中图分类号] R692.5 [文献标识码] A [DOI] 10.3969/j.issn.1673-9701.2023.24.001
Correlation of serum vitamin K2 and IL-6 levels with coronary artery calcification in chronic kidney disease patients
WANG Mudan1, ZHOU Lina1, YANG Zhonghuang1, LI Enci1, LIANG Shikai2
1.Department of Nephrology, Wenzhou Peoples Hospital, Wenzhou 325000, Zhejiang, China; 2.Zhejiang Provincial Peoples Hospital, Hangzhou 310000, Zhejiang, China
[Abstract] Objective To investigate the correlation of serum vitamin K2 and interleukin-6 (IL-6) levels with coronary artery calcification (CAC) in chronic kidney disease (CKD) patients. Methods A total of 111 patients who admitted to the department of nephrology in Wenzhou Peoples Hospital for chronic kidney disease during January 2019 to June 2022 were collected and divided into different groups. The levels of serum vitamin K2 and IL-6 were detected by enzyme linked immunosorbent assay (ELISA). Chest CT was assessed by Agatston score; The relationship between vitamins K2, IL-6 and CAC was analyzed. Results The levels of age, hypersensitive-C-reactive-protein (hs-CRP), phosphorus, parathyroid hormone (PTH), homocysteine (Hcy), and IL-6 were higher in the CAC group than those in the non-CAC group, while estimated glomerular filtration rate (eGFR) and vitamin K2 were lower than those in the non-CAC group. By logistic regression analysis, advancde age, high levels of Hcy and IL-6 were independent risk factors for CAC (OR were 1.69, 1.14 and 1.12, 95%CI were 1.237-2.181, 1.005-1.623, 1.014-1.328, respectively). eGFR, vitamin K2 were protective factors of CAC (OR were 0.328, 0.243, 95%CI were 0.216-0.713, 0.076-0.651); Vitamin K2 in the severe CAC group was lower than in the mild CAC group, while IL-6 was higher in the mild、moderate groups than the severe CAC group (F were 5.70, 6.13, P<0.05). Conclusion Advancde age, high levels of Hcy and IL-6 were independent risk factors for CAC, while eGFR and vitamin K2 were the protective factors for CAC.
[Key words] Vitamin K2; IL-6; Chronic kidney disease; Coronary artery calcification
![]() 慢性肾脏病(chronic kidney disease,CKD)非常普遍,对公众健康构成严重威胁[1]。据估计CKD患者的死亡风险较正常人群高8倍,54%~100%的患者存在血管钙化[2-3]。最新研究显示维生素K2不仅能通过dp-ucMGP抑制血管钙化,而且能通过生长停滞特意基因6(growth arrest specific gene 6,Gas 6)抑制血管平滑肌细胞钙化[4-5]。研究证实维生素K2水平较高者出现冠脉事件风险偏低[6-7];CKD患者普遍存在维生素K2缺乏,但其与CKD患者的冠状动脉钙化(coronary artery calcification,CAC)的相关性研究较少。微炎症在CKD患者中常见,与多种原因有关,如营养不良、氧化应激等。研究报道血管钙化患者白细胞介素6(interleukin-6,IL-6)水平较高[3,8]。本研究拟观察CKD患者中维生素K2、IL-6水平变化,进一步探讨其与CAC及严重程度的关系。
慢性肾脏病(chronic kidney disease,CKD)非常普遍,对公众健康构成严重威胁[1]。据估计CKD患者的死亡风险较正常人群高8倍,54%~100%的患者存在血管钙化[2-3]。最新研究显示维生素K2不仅能通过dp-ucMGP抑制血管钙化,而且能通过生长停滞特意基因6(growth arrest specific gene 6,Gas 6)抑制血管平滑肌细胞钙化[4-5]。研究证实维生素K2水平较高者出现冠脉事件风险偏低[6-7];CKD患者普遍存在维生素K2缺乏,但其与CKD患者的冠状动脉钙化(coronary artery calcification,CAC)的相关性研究较少。微炎症在CKD患者中常见,与多种原因有关,如营养不良、氧化应激等。研究报道血管钙化患者白细胞介素6(interleukin-6,IL-6)水平较高[3,8]。本研究拟观察CKD患者中维生素K2、IL-6水平变化,进一步探讨其与CAC及严重程度的关系。
1 资料与方法
1.1 一般资料
选取2019年1月至2022年6月在温州市人民医院肾内科诊断为CKD的住院患者。入选标准:①年龄>18岁;②已明确诊断为CKD,处于CKD2~5期非透析患者。排除标准:①有急性感染及炎症表现;②肿瘤病史;③精神异常家族病史;④肝功能异常。本研究共入选111例CKD患者,其中男61例,女50例;年龄18~82岁;原发病诊断为慢性肾小球肾炎35例,糖尿病肾病30例,高血压肾病26例,多囊肾4例,慢性间质性肾炎5例,病因不详CKD 11例。CKD患者根据EPI公式估算肾小球滤过率(estimated glomerular filtration rate,eGFR),将CKD患者分为CKD2~5期。根据是否存在CAC分为非CAC组和CAC组,CAC组进一步根据Agatston评分为轻度、中度或重度(<100分为轻度CAC组,100~400分为中度CAC组,>400分为重度CAC组)。本研究经温州市人民医院伦理委员会审批[伦理审批号:伦审(2019)第(46)号],所有患者均签署知情同意书。
1.2 检测方法
各组患者均空腹抽取静脉血,采用酶联免疫吸附试验(enzyme linked immunosorbent assay,ELISA)检测血维生素K2和IL-6水平。试剂盒购自上海仁捷生物科技有限公司,所有操作均严格按照试剂盒说明书进行。
1.3 CAC评估
CAC在温州市人民医院采用非增强胸部CT按照特殊標准进行量化,采用Agatston评分评价CAC。钙化评分工作由专业影像科医生进行。
1.4 统计学方法
采用SPSS 21.0统计学软件进行分析。计量资料采用均数±标准差(![]() )表示,比较采用t检验;非正态分布数据以中位数(四分位数间距)[M(Q1,Q3)]表示,组间比较用非参数检验;计数资料以例数(百分率)[n(%)]表示,比较采用c2检验;多组间比较采用方差分析,进一步两两比较用LSD-t检验;多因素分析用Logistic分析回归;P<0.05为差异有统计学意义。
)表示,比较采用t检验;非正态分布数据以中位数(四分位数间距)[M(Q1,Q3)]表示,组间比较用非参数检验;计数资料以例数(百分率)[n(%)]表示,比较采用c2检验;多组间比较采用方差分析,进一步两两比较用LSD-t检验;多因素分析用Logistic分析回归;P<0.05为差异有统计学意义。
2 结果
2.1 一般临床资料及维生素K2、IL-6水平比较
CKD患者中,CAC发生率为57.6%(63/111)。CAC组患者的年龄、高敏C反应蛋白(hypersensitive- C-reactive-protein,hs-CRP)、血磷、甲状旁腺素(parathyroid hormone,PTH)、Hcy和IL-6均高于非CAC组,差异有统计学意义(P<0.05);CAC组患者的eGFR和维生素K2水平低于非CAC组,差异有统计学意义(P<0.05);CAC组患者的糖尿病及吸烟比例较非CAC组高,但差异无统计学意义(P>0.05),见表1。
2.2 CAC相关因素分析
以CKD患者是否存在CAC(是=1,否=0)为因变量,以年龄、血磷、PTH、hs-CRP、Hcy、IL-6、eGFR及维生素K2水平为自变量,纳入多因素回归模型。结果显示,年龄、Hcy、IL-6是CKD患者发生CAC的独立危险因素(P<0.05),eGFR和维生素K2是独立保护因素(P<0.05),见表2。
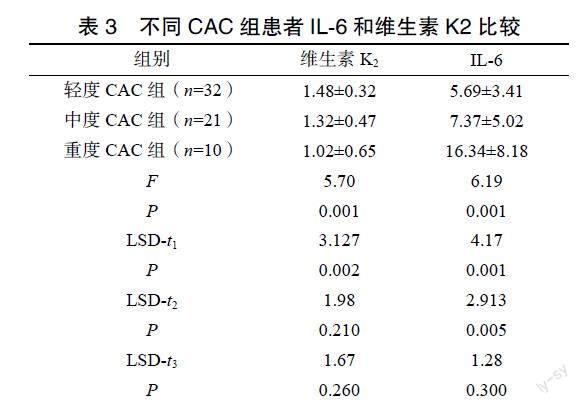
2.3 不同CAC程度的患者IL-6和维生素K2比较
根据评分将CAC分为轻度32例,中度21例及重度10例。重度CAC组维生素K2水平较轻度CAC组和中度CAC组低,但仅与轻度CAC组差异有统计学差异(P<0.05)。重度CAC组IL-6水平较轻度CAC组和中度CAC组高;轻度CAC组与中度CAC组的维生素K2、IL-6水平差异无统计学意义(P>0.05),见表3。
3 讨论
本研究探讨维生素K2与CKD患者CAC的关系,结果显示维生素K2在CAC组明显降低,提示维生素K2是CKD患者CAC的保护因素。维生素K2抑制血管钙化的机制:①通过介导羧基谷氨酸蛋白(matrix gla protein,MGP)羧化发挥作用;②通过影响Gas 6羧化发挥作用[9]。近期研究表明补充维生素K2可改善肾移植患者的动脉僵硬度[10]。Joanna等[3]研究CKD 2~5期患者血管钙化生物标志物,结果显示随着CKD的进展,血IL-6水平显著升高,患者5年全因和心血管死亡风险也显著升高,故认为炎症参与CKD患者CAC,其机制可能是由于IL-6促进Runx2的表达,从而诱导平滑肌细胞发展成骨细胞样特征[11]。另有研究提示Hcy在CKD患者心血管疾病中起一定作用[12]。本研究结果也证实Hcy与CAC存在相关性。此外,本研究未显示血脂代谢紊乱在非CAC组和CAC组间的差异,可能是由于CKD患者接受他汀治疗后影响结果所致。
本研究具有一定的局限性:①证实升高的维生素K2、IL-6和CAC之間的关联,但未确定因果关系;②入选患者为住院患者,研究可能存在选择性偏差;③由于时间限制,本研究无长期随访资料,无法判断预后;④样本量较小,存在一定程度的偏倚。未来研究可通过扩大样本量、延长随访时间等进一步评估维生素K2、IL-6和CKD患者CAC及预后的相关性,并探讨CKD患者是否需要常规补充维生素K2等临床问题。
[参考文献]
[1] ZHANG L, WANG F, WANG L, et al. Prevalence of chronic kidney disease in China: A cross-sectional survey[J]. Lancet, 2012, 379(9818): 815–822.
[2] BANSAL N. Evolution of cardiovascular disease during the transition to end-stage renal disease[J]. Semin Nephrol, 2017, 37(2): 120–131.
[3] JOANNA K, MAREK S, KRZYSZTOF M, et al. IL-6 but not TNF is linked to coronary artery calcification in patients with chronic kidney disease[J]. Cytokine, 2019, 120(8): 9–14.
[4] DISTHABANCHONG S, BOONGIRD S. Role of different imaging modalities of vascular calcification in predicting outcomes in chronic kidney disease[J]. World J Nephrol, 2017, 6(3): 100–110.
[5] 吴志茹, 王梦慈, 吴雪平, 等. 血清去磷酸化未羧化基质Gla蛋白和维生素K2水平与慢性肾脏病患者血管钙化相关性研究[J]. 中国血液净化, 2022, 21(4): 253–257.
[6] 魏萌, 魏丽敏, 王萌, 等. 维持性血液透析患者血管钙化的危险因素分析[J]. 中国血液净化, 2020, 19(11): 742–746.
[7] HAUGSGJERD T R, EGELAND G M, NYG?RD O K, et al. Association of dietary vitamin K and risk of coronary heart disease in middle-age adults: The Hordaland Health Study Cohort[J]. BMJ Open, 2020, 10(5): e035953.
