Lower alanine aminotransferase levels are associated with increased all-cause and cardiovascular mortality in nonalcoholic fatty liver patients
2023-07-04JiaRuiZhengZiLongWangSuZhenJiangHongSongChenBoFeng
Jia-Rui Zheng,Zi-Long Wang, Su-Zhen Jiang, Hong-Song Chen, Bo Feng
Abstract
Key Words: Non-alcoholic fatty liver disease; Alanine aminotransferase; Mortality; NHANES-III
INTRODUCTION
The number of patients suffering from nonalcoholic fatty liver disease (NAFLD) has reached one billion worldwide, replacing viral hepatitis as the most common chronic liver disease[1-3], as well as increasing the risk of hepatocellular carcinoma[4].Research has demonstrated that NAFLD is no longer restricted to the liver itself but is also the main manifestation of metabolic syndrome in the liver, which is closely related to obesity, dyslipidemia, hypertension, type 2 diabetes, insulin resistance, and cardiovascular disease[5,6].The all-cause mortality of patients with NAFLD is significantly increased, and cardiovascular disease, malignant tumors, and end-stage liver disease are the main causes of death in patients with NAFLD[7-9].Therefore, it is very important to find an effective treatment for NAFLD.
The elevation of alanine aminotransferase (ALT) is a measure of liver disease activity and liver injury severity.Several studies have shown that an increase in ALT levels has a close correlation with an increased risk of NAFLD.It has also been proven to be an independent predictor of NAFLD and is related to nonalcoholic steatohepatitis and advanced liver fibrosis[10-12].Research has shown that elevated ALT levels are also positively correlated with metabolic syndrome-related diseases, such as cardiovascular disease and type 2 diabetes[13,14].Based on these previous findings, it could be inferred that all-cause and cardiovascular mortality are correlated with elevated ALT levels.However, this conclusion appears to be inconsistent and controversial[15-17].Elevated ALT levels are related to mortality from various causes in some studies[18,19], but not in others[20,21].In contrast, some studies have indicated that normal or lower ALT levels appear to be negatively correlated with a higher risk of all-cause mortality[22,23].Moreover, the relationship between ALT levels and all-cause and causespecific mortality in patients with NAFLD has not been fully reported.Therefore, this study focuses on the relationship between serum ALT levels and all-cause mortality and cause-specific mortality in patients with NAFLD in the Third National Health and Nutrition Examination Survey (NHANES-III)database, so as to further explore the clinical significance of using ALT as a potential treatment target and to improve the survival and prognosis of patients with NAFLD.
MATERIALS AND METHODS
Dataset and study population
The NHANES-III produced a national dataset that evaluates the health status of people in the United States, and it was conducted in two phases (1988-1991 and 1991-1994).The NHANES-III conducted interviews, physical examinations, and laboratory tests, and, at the same time, it used ultrasonic examination to evaluate hepatic steatosis, which is the main reason the authors chose this dataset.Data from NHANES-III was also linked to death certificates from the National Death Index (NDI) as of December 31, 2019, allowing for mortality analysis.The NHANES protocol was approved by the Ethics Review Committee of the National Center for Health Statistics, which obtained informed consent from all subjects.
Among the adult participants (aged 20-74 years old) in the NHANES-III survey with liver/gallbladder ultrasound and laboratory test results (n= 14797), individuals without a liver ultrasound steatosis grade and those with significant alcohol consumption (men > 21 drinks/week, women > 14 drinks/week), viral hepatitis (serum hepatitis B surface antigen and/or serum hepatitis C antibody positive), or iron overload (transferring saturation ≥ 50%) (n= 2217) were excluded from this study.Individuals with incomplete mortality information and certain important indicators were also excluded(n= 1139).Finally, this study included a total of 11,441 individuals aged 20-74 years (Figure 1).
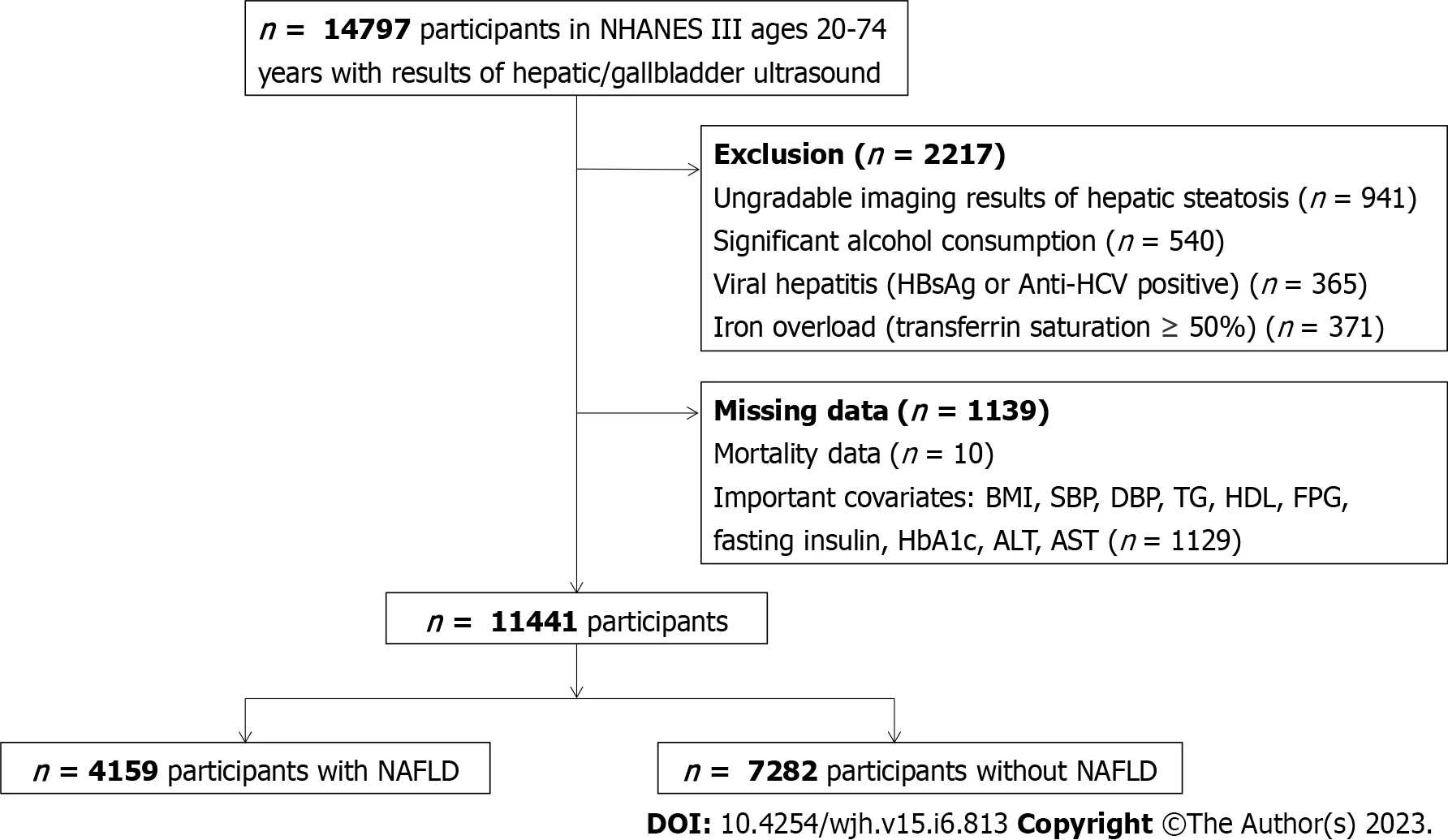
Figure 1 Flow-chart of the Study.NHANE III: The National Health and Nutrition Examination Survey III (1988-1994); HBsAg: Hepatitis B surface antigen; HCV:Hepatitis C virus; BMI: Body mass index; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; TC: Total cholesterol; TG: Triglyceride; HDL: High-density lipoprotein cholesterol; FPG: Fasting plasma glucose; HbA1c: Glycosylated hemoglobin; ALT: Alanine aminotransferase; AST: Aspartate aminotransferase; NAFLD:Nonalcoholic fatty liver disease.
Clinical variables
An elevated ALT level was defined as ALT > 30 U/L in males and > 19 U/L in females, and the ALT levels were classified into four groups [< 0.5 upper limits of normal (ULN), 0.5-1 ULN, 1-2 ULN, ≥ 2 ULN].Race/ethnicity was categorized as non-Hispanic white, non-Hispanic black, Mexican–American,or other.Diabetes was defined as a high fasting blood sugar (> 126 ng/dL), a high glycosylated hemoglobin (HbA1c) (> 6.5%), or a history of diabetes and/or use of diabetic medication.A homeostasis model assessment of insulin resistance > 2.5 was considered as insulin resistant[24].Hypertension was defined as systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg and/or treatment with antihypertensive medication.A self-reported questionnaire on the frequency and amount of alcohol consumption was used to identify drinking status[25].If people answered "no" to having done any of the following activities in the previous month, they were classified as being"sedentary" in terms of sports activities: jogging/running, cycling, swimming, aerobic exercise, other dancing, aerobics, yard work/gardening, weightlifting, or other sports[26].
Definition of NAFLD
The gallbladder ultrasound image files were reviewed by three board-certified clinicians to assess hepatic steatosis.In this study, NAFLD was defined as any degree (mild to severe) of steatosis,according to five criteria, without a competing etiology for secondary liver steatosis.
Mortality
Participants who were aged over 20 years in the NHANES-III were followed up for passive mortality as of December 31, 2019.Probability matching was performed using NDI records to assess the death status(including the date of death) and the cause of death; the potential cause of death 113 code was used to code deaths before 1998, and deaths between 1999 and 2015 were coded according to the Ninth Revision of the International Classification of Diseases.The Centers for Disease Control and Prevention restricted the liver-related mortality data in the NHANES III for public use.
Statistical analysis
All data were analyzed using SPSS 27.0.Weighted analyses were performed using NHANES survey weights[27].The Student’st-test was used to compare continuous variables, and the Rao-Scott chisquare was used to test categorical variables.Multivariate logistic regression was used to confirm an independent relationship between ALT status and NAFLD after adjustment for potential clinical and demographic variables.Cox proportional hazards regression analysis was used to analyze all-cause and cause-specific mortality.APvalue < 0.05 was considered to have a significant statistical difference.
RESULTS
Baseline characteristics of patients
Of the 11441 NHANES-III survey participants (mean age, 44.4 years; male, 44.6%) enrolled in this study,the prevalence of NAFLD was 36.4%, among which moderate to severe steatosis accounted for 22.8%.In this cohort, 84.8% of the participants had normal ALT levels, and 15.2% had elevated ALT levels.Table 1 summarizes the baseline characteristics of the overall population and patients with NAFLD.In the whole population, compared with the individuals with normal ALT levels, those with elevated ALT levels were more likely to be young people, women, or Mexican Americans, those who did little physical activity, and those who were diabetic and insulin resistant.In addition, body mass index (BMI),waist circumference, TC, TG, HbA1c, FPG, and AST were higher in these people, and HDL was lower.The prevalence of NAFLD was higher in individuals with elevated ALT levels compared with those with normal ALT levels (59%vs32.3%,P< 0.001).In patients with NAFLD, compared with individuals with normal ALT levels, those with elevated ALT levels were also younger, more likely to be women,Mexican American, diabetic, insulin resistant, and they had higher BMI, waist circumference, TC, TG,and AST levels.The proportion of patients with moderate and severe steatosis was higher (47.7% and 30.1%, respectively).When ALT was classified into different levels (< 0.5 ULN, 0.5-1 ULN, 1-2 ULN, and≥ 2 ULN), in the univariate model, the incidence of NAFLD increased with the increase in ALT level[odds ratio (OR): 1, 1.65, 3.56, and 6.72 respectively,P< 0.001].When adjusted for age, this relationship still existed.Multivariate analysis showed that with the increase in ALT level, the risk of NAFLD increased by 37%, 128%, and 217%, respectively (Supplementary Table 1).
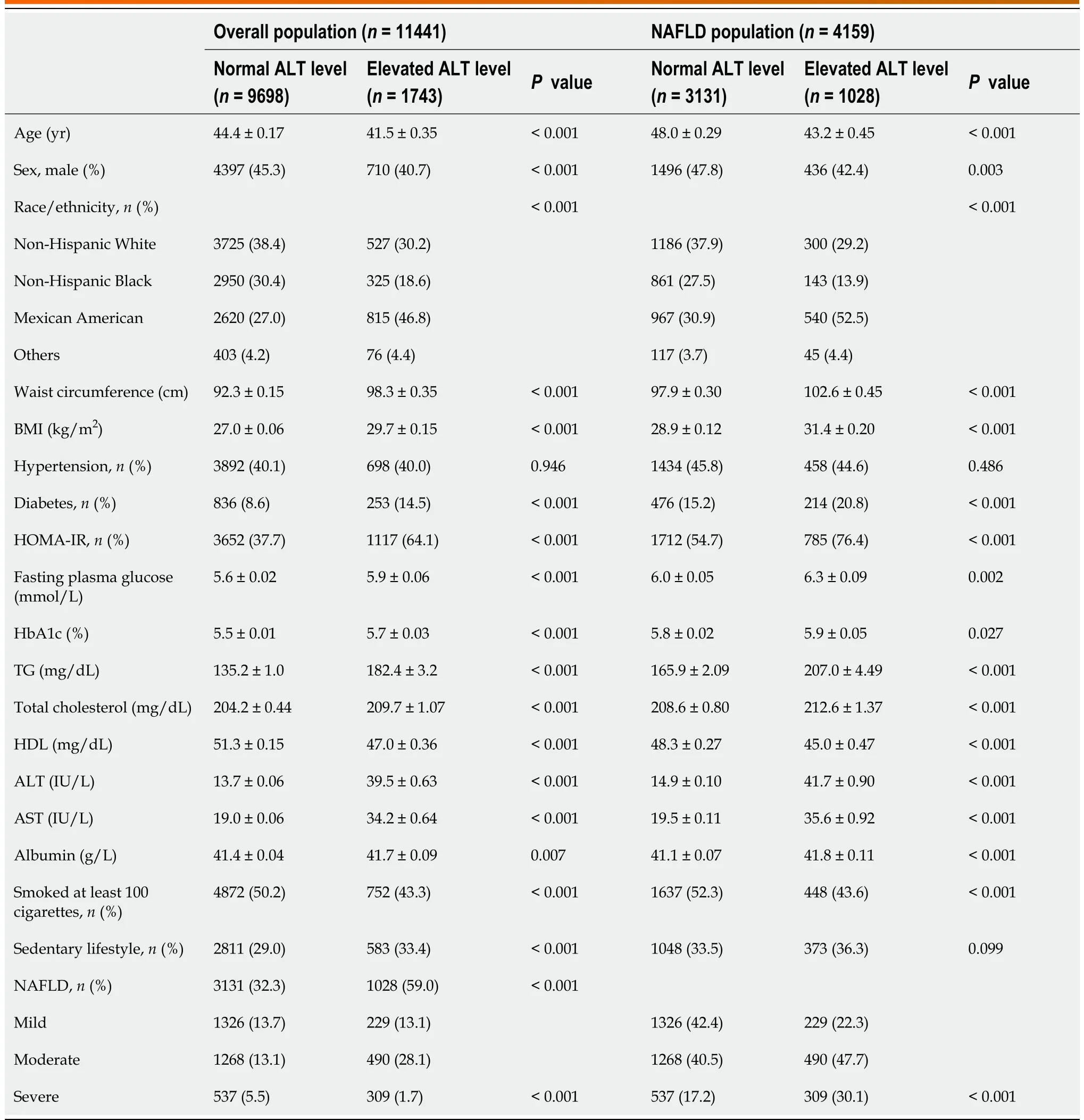
Table 1 Baseline characteristics of the overall population and nonalcoholic fatty liver disease patients with normal or elevated alanine aminotransferase level
ALT levels and mortality in the overall population
The average follow-up time of the 11,441 individuals was 23.8 years.A total of 3,976 people died during the follow-up period, and cardiovascular disease (n= 1104) and cancer (n= 953) were the two leading causes of death.The results of the Cox proportional hazards regression analysis of the overall population are given in Table 2.The univariate analysis showed that all-cause mortality gradually decreased with the increase in ALT level [hazard ratio (HR): 0.76, 0.66, and 0.60, respectively,P< 0.001].When considering known demographic variables and traditional risk factors, all-cause mortality was still the highest when ALT was at the lowest level (< 0.5 ULN).With regard to NAFLD, in univariate analysis, patients with NAFLD had a 41% higher risk of all-cause death than the patients who did not have NAFLD [HR: 1.41, 95% confidence interval (CI): 1.33-1.51,P< 0.001].However, NAFLD was no longer correlated with all-cause mortality when other demographics and covariates were controlled.
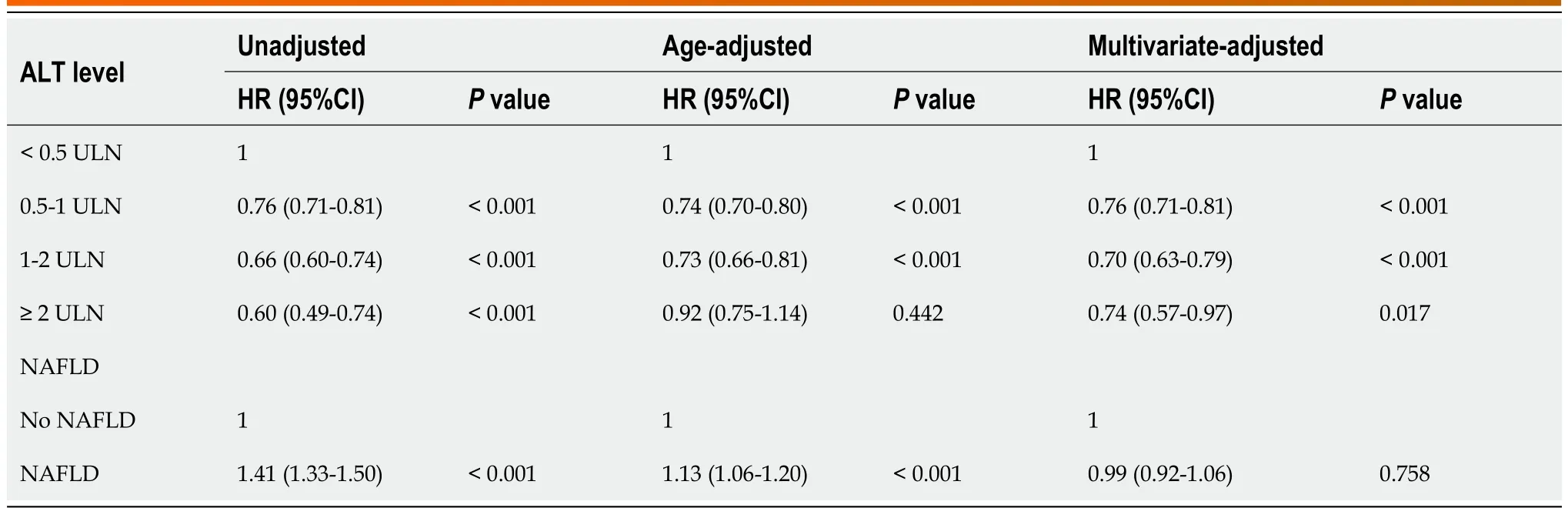
Table 2 Association between alanine aminotransferase level or nonalcoholic fatty liver disease status and all-cause mortality in overall population
When mortality was limited to cardiovascular disease (Table 3), the multivariable analysis indicated that elevated ALT levels were correlated with decreased cardiovascular mortality in individuals overall and in patients with NAFLD, but there was no significant statistical difference when ALT was ≥ 2 ULN.Death caused by other diseases, such as respiratory and cerebrovascular diseases, with different ALT levels also showed a similar result.The analysis of cancer-related mortality had a different result; when ALT was ≥ 2 ULN, the risk of cancer-related death in the whole population increased by 11% and, in patients with NAFLD, it increased by 39%, but there was no significant statistical difference.
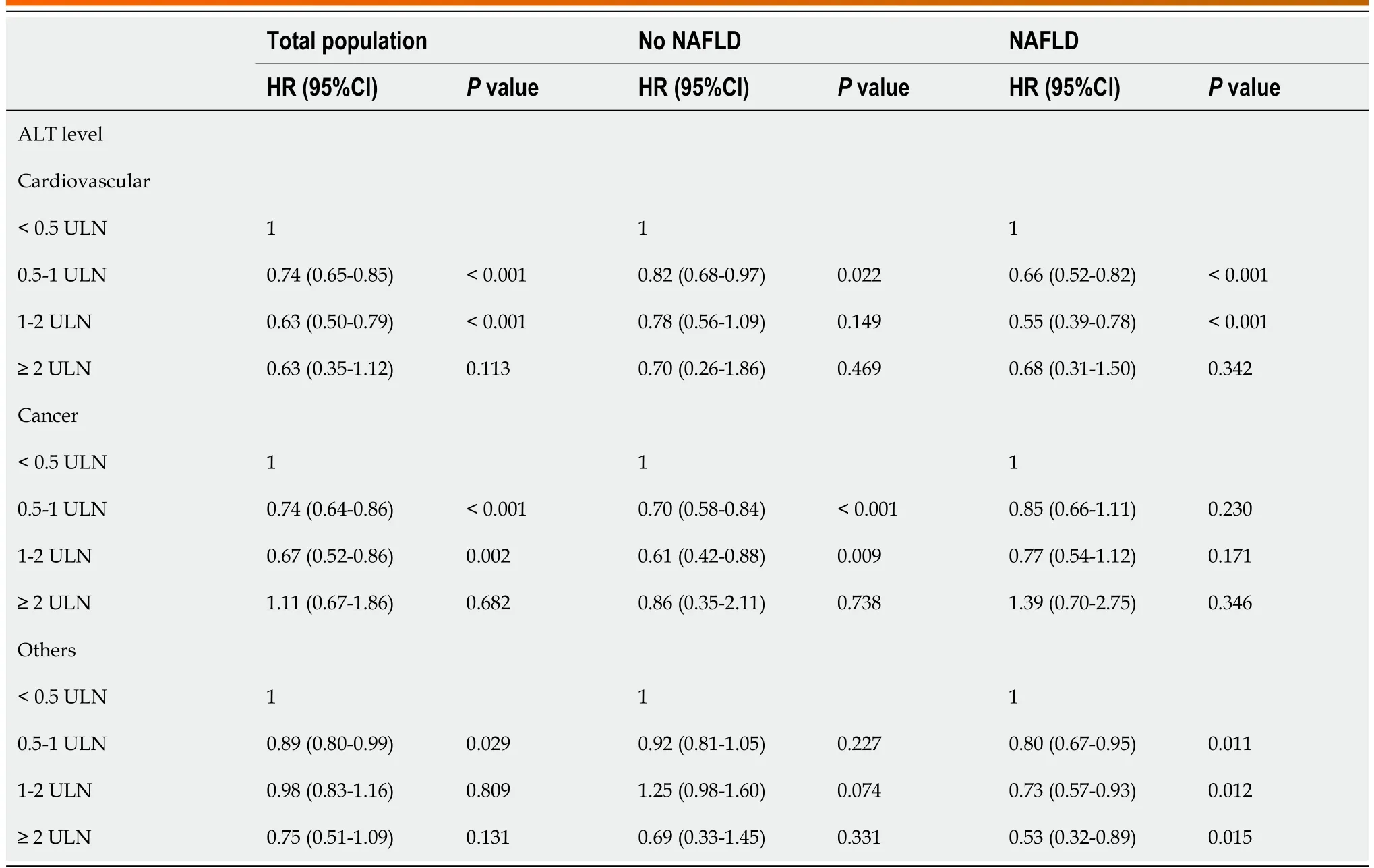
Table 3 Association of alanine aminotransferase level, cardiovascular disease, cancer-related and others-related mortality stratified by the presence/absence of nonalcoholic fatty liver disease
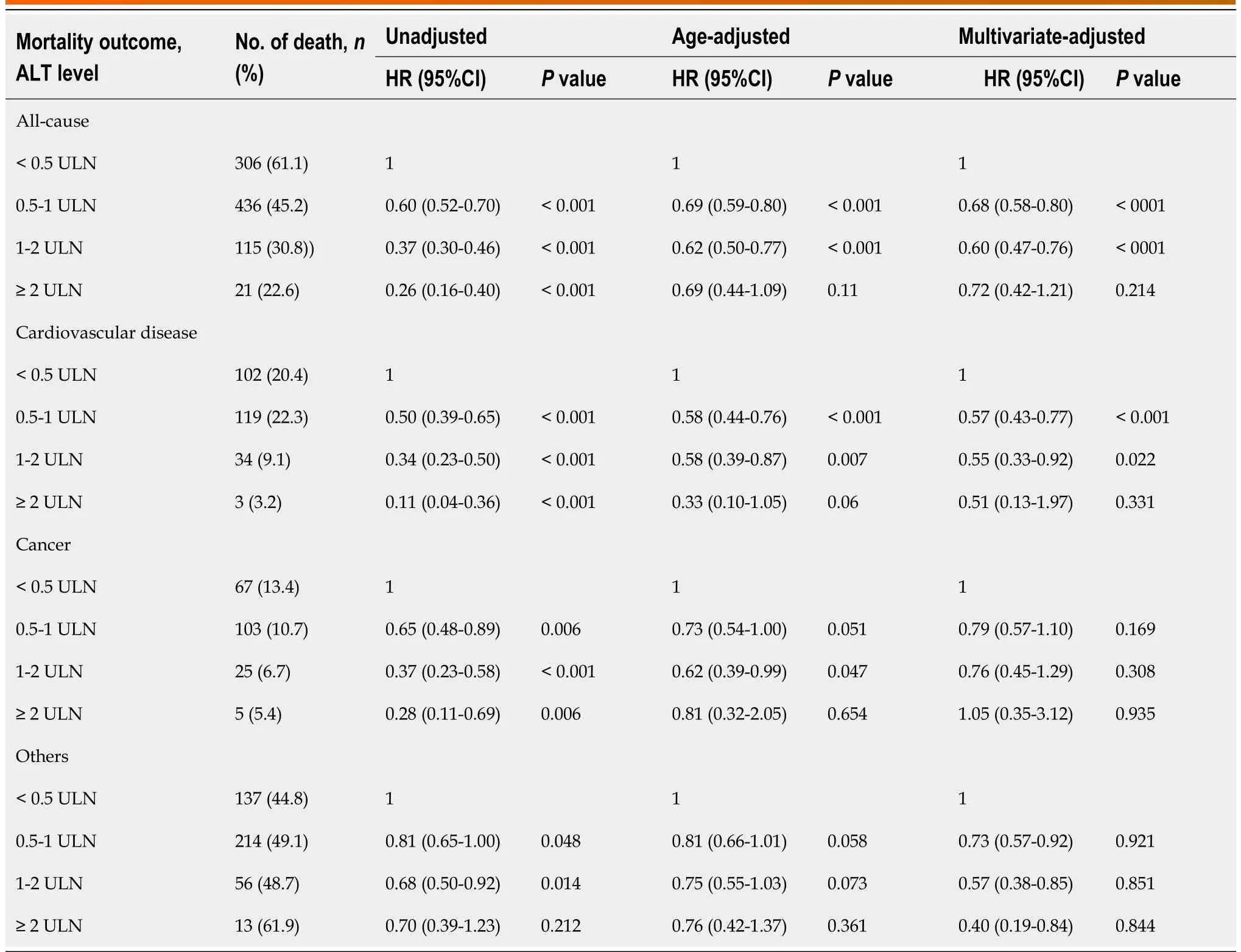
Table 4 Association of alanine aminotransferase level, all-cause, cardiovascular disease, cancer-related and others-related mortality among nonalcoholic fatty liver disease patients in men
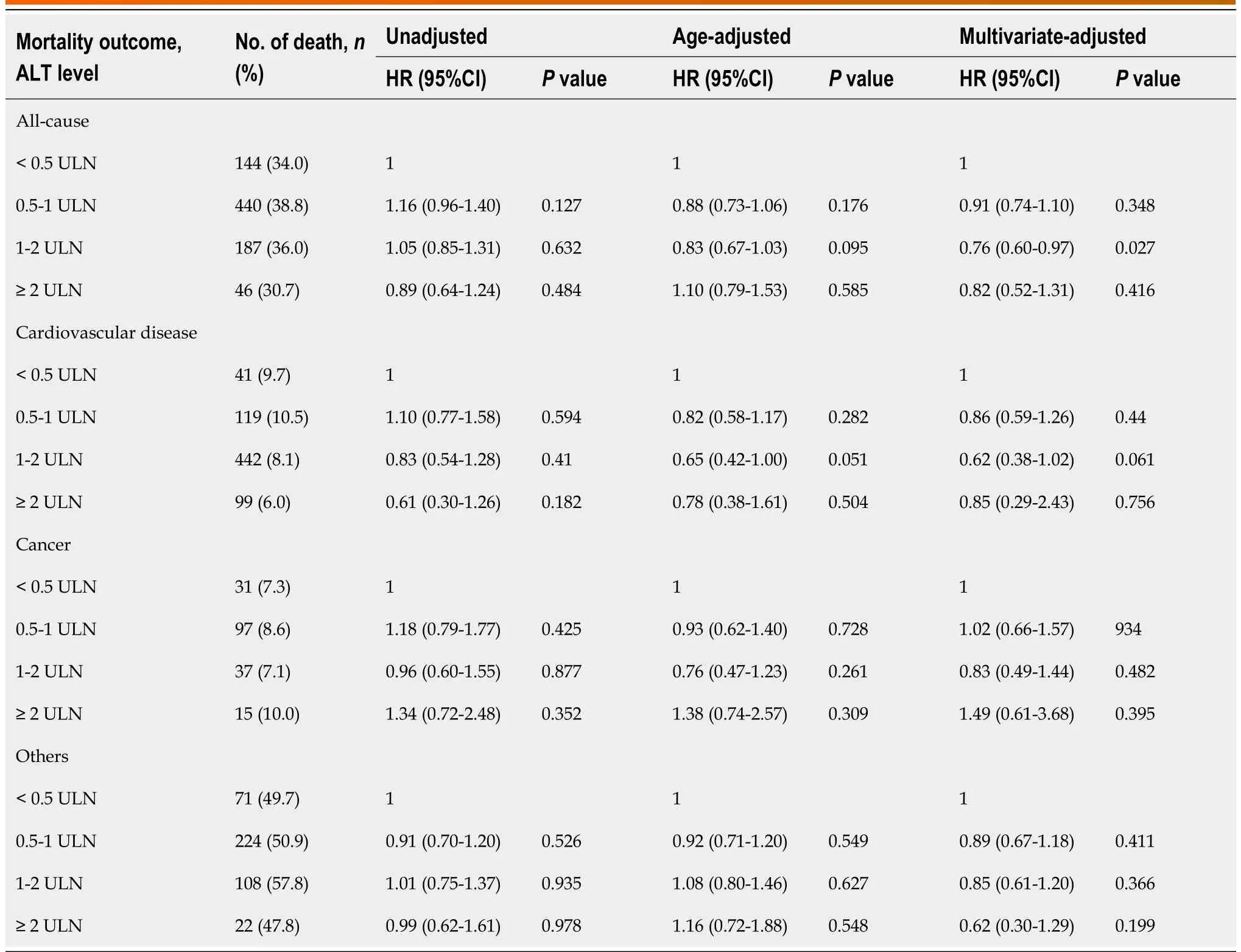
Table 5 Association of alanine aminotransferase level, all-cause, cardiovascular disease, cancer-related and others-related mortality among nonalcoholic fatty liver disease patients in women
ALT levels and mortality in patients with NAFLD
Further research was done concerning the patients with NAFLD (Supplementary Table 2 in the ESM).Because the ULN of the ALT level differs in men and women, an analysis was performed according to gender.The baseline characteristics of the enrolled patients with NAFLD are summarized in Supplementary Table 3 in the ESM.A total of 1932 men and 2227 women are included, with an average age of 47.9 and 45.8 years, respectively.The median ALT level was 25 U/L in men and 18 U/L in women.In most patients with NAFLD, ALT levels were within the normal range, of which 0.5-1 ULN was the most common (found in 49.9% of males and 50.9% of females, respectively).All-cause mortality and cause-specific mortality were investigated based on ALT levels in men and women.In male patients with NAFLD, the univariate model showed that all-cause and cancer-related mortality decreased with the increase in ALT level, but the age-adjusted and multivariate models showed that mortality increased when ALT was ≥ 2 ULN.However, the difference was not statistically significant.Regarding death caused by cardiovascular disease and other causes, the three models showed that the risk of death decreased with the increase of ALT level.Among female patients, cancer-related mortality was thehighest in the univariate, age-adjusted, and multivariate models when ALT was ≥ 2 ULN, which was similar to the results in the whole population with NAFLD (Tables 4 and 5).
The different models and mortality in patients with NAFLD
The different NAFLD statuses (mild to moderate or severe) were then combined with the different ALT levels (normal or elevated) for further analysis of all-cause and cause-specific mortality.In patients with NAFLD, the univariate and age-adjusted models showed that severe NAFLD with normal ALT levels had the highest all-cause mortality (HR: 1.45,P< 0.001 and 1.11,P= 0.139), but this relationship no longer existed after multivariable adjustment (HR: 0.98,P= 0.727) (Table 6).In terms of cause-specific mortality, Model 1 (mild to moderate NAFLD with normal ALT level) and Model 3 (severe NAFLD with normal ALT level) had a higher risk of death than Model 2 (mild to moderate NAFLD withelevated ALT level) and Model 4 (severe NAFLD with elevated ALT level).Further analysis was made according to gender (Supplementary Tables 4 and 5).Among male patients with NAFLD, those with severe NAFLD and elevated ALT levels had higher cancer-related mortality (HR: 1.18,P= 0.602).The risk factors of ALT at the lowest and highest levels were explored (Supplementary Table 6 in the ESM).In male patients, the univariate analysis indicated that the age of those with ALT ≥ 2 ULN wassignificantly lower than that of those with ALT < 0.5 ULN, with more patients aged 20-39 years and fewer patients aged over 60 years.The multivariable-adjusted analysis also indicated that age was a protective factor in male patients.However, in female patients, no significant statistical difference was seen between the two age groups.

Table 6 Association of different models, all-cause, cardiovascular disease, cancer-related and others-related mortality among nonalcoholic fatty liver disease patients
DISCUSSION
The main findings of the present large cohort study were that elevated serum ALT levels were closely related to the increased risk of NAFLD but did not increase the risk of all-cause and cardiovascular mortality in the whole population and in patients with and without NAFLD.On the contrary, in the patients with NAFLD, all-cause and cardiovascular mortality was the highest when ALT was < 0.5 ULN, and this was the same for both sexes and all ages.Cancer-related mortality was the highest when ALT was ≥ 2 ULN, but there was no significant statistical difference.With different degrees of NAFLD(mild to moderate or severe), whether the ALT level was elevated or not seems to have had no significant effect on all-cause and cause-specific mortality.
为提高国产存储阵列的数据安全性,保证存储阵列客户端的隐私安全,同时不降低存储系统高速率、高带宽的数据传输性能,文中提出了一种基于硬件加解密的国产平台安全存储阵列设计与实现方法,实现对存储阵列中核心数据进行快速、有效加解密,最大程度地保护存储阵列客户端的信息安全。基于本文所述架构实现的安全存储阵列具有高通用性和灵活性,不但减少了对系统计算资源的占用,而且利用硬件加解密快速、较难破解的特性,大幅提升了国产平台存储阵列的安全性,对提高我国国产存储领域的数据信息安全具有较高的意义。
Previous research has shown that NAFLD is related to a higher risk of all-cause mortality[28].In addition, the correlation between NAFLD and increased risk of cardiovascular events was proved in a meta-analysis[29].Cardiovascular disease, malignant tumors, and end-stage liver disease are the main causes of death in patients with NAFLD[7,8], but cardiovascular disease is the primary cause of death[7].Therefore, it is of great importance to recognize the significant influence of metabolic complicationson NAFLD, especially as seen in patients with NAFLD who died of cardiovascular disease.Since ALT is often considered a marker to evaluate the activity of liver disease and the severity of liver injury in clinical practice, many believe that monitoring ALT levels can be an effective means of following the progression of NAFLD[30,31].Because of the invasive nature of liver biopsy, clinicians often take ALT levels as the basis of liver protection treatment.The association between elevated ALT levels and increased mortality has been reported in several epidemiological studies[18,32].It seems to be a reasonable inference that elevated ALT levels may increase the risk of death.However, in different countries and cohorts, the opposite relationship between ALT levels and all-cause mortality has been observed.One study of NHANES-III data found that the relationship between ALT levels and all-cause mortality was similar to a U-shaped curve[22].Another large cohort study also indicated that ALT at the lowest levels (≤ 10 U/L) and elevated ALT levels (> 40 U/L) were associated with increased all-cause mortality, especially among people aged over 60 years[33].Two recent studies also showed that lower ALT levels within the normal range were related to a higher risk of all-cause and cardiovascular mortality in the elderly population[34,35].These findings consistently indicate that there is a certain non-linear correlation between ALT levels and all-cause mortality although some unmeasured or residual confounding cannot be excluded.
The results of the current study showed that in patients with NAFLD, the ALT levels of the vast majority, both male and female, are within the normal range, and the number of patients with an ALT level in the range of 0.5-1 ULN is the largest, while the number in the range ≥ 2 ULN is the smallest.In addition, nearly half of the male patients with NAFLD with an ALT level < 0.5 ULN were elderly, while nearly 3/4 of those with an ALT level ≥ 2 ULN were young.Another study also showed that the ALT level first increased and then decreased with age[36], which may explain why in patients with NAFLDthe mortality rate is the highest when ALT is < 0.5 ULN.That is to say, during the follow-up period of over 31 years, individuals with an ALT level < 0.5 ULN at baseline were mostly elderly, so the rate of all-cause and cause-specific death outcomes was higher.However, most of the patients with ALT level ≥2 ULN at baseline were young people, so the rate of endpoint events was low.However, in the ageadjusted model and multivariable model, the results were still approximately the same, which shows that other factors besides age may play a more important role, and this possibility needs further study.
Three mechanisms might explain the underlying association between ALT levels and death.First, as an enzyme, ALT plays a vital role in converting L-alanine and α- ketoglutarate to pyruvate and glutamic acid in the heart, liver, kidney, skeletal muscle, and brain, and a low ALT level increases the risk of death by reducing the catalytic capacity for the vital metabolic steps of amino acid metabolism and gluconeogenesis[37-40].Second, a low ALT level indicates a vitamin B6 deficiency, and epidemiological evidence indicates that a deficiency of vitamin B6 can increase the risk of cardiovascular disease,immune dysfunction, depression, and neurocognitive impairment[41,42].Finally, other unmeasured confounding factors, rather than vitamin B6, may lead to death.
It was also found that the BMI of male and female patients with NAFLD with ALT levels < 0.5 ULN were 26.8 kg/m2and 27.8 kg/m2, respectively.Recent epidemiological studies have shown that mild obesity (BMI: 23-29 kg/m2) has a protective effect on overall mortality[43,44].However, the underlying mechanism is unclear and needs further research.
Some limitations exist to the current study.First, it is a cross-sectional observation of the relationship between ALT levels and NAFLD, so the time correlation cannot be determined.Second, the diagnosis of NAFLD was carried out by hepatic ultrasound, which does not distinguish fat accumulation of less than 30%[45].However, the advantages of ultrasound include safety, repeatability, low cost, high sensitivity,and specificity[46].Therefore, ultrasound is considered a first-line imaging technology in epidemiological research and clinical practice[47].Third, despite the adjustments of multiple covariates affecting all-cause and cause-specific mortality, some unmeasured or residual confounding factors may still exist.It was also not possible to extract specific information about liver-related mortality (due to NHANES),and obtaining such data could provide more clarity.Finally, since the participants in NHANES-III represent the population from 1988 to 1994, there may have been a much lower prevalence of diabetes and NAFLD than would be expected today.
However, this study also has its strengths.This is the first study focusing on ALT levels and all-cause and cause-specific mortality in patients with NAFLD.In a large cohort of the United States population,there are rich demographic and metabolic variables, with a median follow-up period of 23.8 years.Unlike other NHANES cycles that lack liver ultrasound results, NHANES-III includes liver steatosis diagnosed by ultrasound, which makes the diagnosis of NAFLD more accurate than that using noninvasive laboratory markers.
CONCLUSION
In conclusion, the present study’s findings confirmed that all-cause and cardiovascular mortality in patients with NAFLD was the highest when ALT was < 0.5 ULN, and, regardless of the severity of the NAFLD, normal or lower ALT levels are associated with higher mortality than elevated ALT levels.This knowledge may be of importance to clinicians who, because of the invasive nature of liver perforation,often use ALT levels as the basis for liver protection treatment.According to the results of this study, in terms of treatment, it may not be beneficial to reduce ALT levels as low as possible.The findings suggest that, on the contrary, clinicians should be more vigilant of patients with NAFLD who have ALT levels < 0.5 ULN.
ARTICLE HIGHLIGHTS

Research perspectives
The underlying mechanism about the lower ALT levels and high mortality death is unclear and needs further research.
FOOTNOTES
Author contributions:Feng B designed the study; Zheng JR and Wang ZL contributed to the acquisition, analysis and interpretation of data and drafted the manuscript; Jiang SZ contributed to the critical revision of the manuscript for important intellectual content and Chen HS contributed to the study supervision; all authors have made a significant contribution to this study and have approved the final manuscript.
Institutional review board statement:The NHANES protocol was approved by the Ethics Review Committee of the National Center for Health Statistics, which obtained informed consent from all subjects.
Informed consent statement:Patients were not required to give informed consent to the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.
Conflict-of-interest statement:The authors have declared no conflict of interest.
Data sharing statement:No additional data are available.
STROBE statement:The authors have read the STROBE Statement—checklist of items, and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Jia-Rui Zheng 0000-0003-0202-7488; Zi-Long Wang 0000-0003-0983-467X; Bo Feng 0000-0001-5084-6715.
S-Editor:Yan JP
L-Editor:A
P-Editor:Yan JP
猜你喜欢
杂志排行
World Journal of Hepatology的其它文章
- Ductular reaction in non-alcoholic fatty liver disease: When Macbeth is perverted
- Recent advances in pathophysiology, diagnosis and management of hepatorenal syndrome: A review
- Treatment of liver fibrosis: Past, current, and future
- Tumor budding as a potential prognostic marker in determining the behavior of primary liver cancers
- Role of vascular endothelial growth factor B in nonalcoholic fatty liver disease and its potential value
- Acute pancreatitis in liver transplant hospitalizations: Identifying national trends, clinical outcomes and healthcare burden in the United States
