Tumor budding as a potential prognostic marker in determining the behavior of primary liver cancers
2023-07-04BetulUnalMennanYigitcanCelikElifOcakGedikCumhurIbrahimBassorgunGulsumOzlemElpek
Betul Unal,Mennan Yigitcan Celik,Elif Ocak Gedik, Cumhur Ibrahim Bassorgun, Gulsum Ozlem Elpek
Abstract
Key Words: Tumor budding; Hepatocellular carcinoma; Cholangiocarcinoma; Prognosis;Liver cancer; Epithelial-mesenchymal transition
INTRODUCTION
Primary liver cancer is the seventh most common cancer worldwide and the fourth leading cause of cancer death[1].Two types of liver cancer constitute a significant majority of cases: Hepatocellular carcinoma (HCC), originating from hepatocytes and usually accompanied by another underlying disease (75%-85%), and intrahepatic cholangiocarcinoma (ICC), arising from the bile duct epithelium(12%-15%)[2].Their incidence rates are increasing in many countries and are expected to continue to rise in the next decade[3,4].Considering that many patients are diagnosed at an advanced stage, there is a lack of current systemic therapy, especially for HCC, and the mortality rates are high, similar to that of other solid organ tumors.Thus, many efforts have been made to identify new markers to determine the course of the disease and the choice of treatment.
Recently, TB has emerged as a promising prognostic parameter to predict tumor behavior and survival across several tumor types[5,6].After the international TB consensus conference, the first guideline for reporting TB was published in 2017[7].Subsequently, the TB score in colorectal carcinoma(CRC) has been included as an important parameter in pathology report protocols[8].These guidelines have also been confirmed to be helpful in cancers of the lung, stomach cancers, and ductal adenocarcinoma of the pancreas[9].However, regarding primary liver tumors, studies focusing on the relationship between TB and clinicopathological parameters and prognosis are relatively new.Nevertheless, numerous studies have shown that many mechanisms involved in TB are associated with tumor behavior in HCC and ICC[10,11].
Therefore, this review aims to provide an overview of the events involved in TB, which is also observed in primary liver tumors.Additionally, this review presents the latest data in these tumors to draw attention to the potential role of this parameter in determining behavior and prognosis and underlines the need to increase the number of further studies focusing on the evaluation of this parameter.
GENERAL OVERVIEW OF THE MECHANISMS OF TB
During the invasion-metastasis process in cancers, tumor cells must undergo various changes to invade the surrounding tissue, transition to the vascular system, and finally engage in a parenchymal invasion of metastatic organs[12].The mechanisms involved in TB are presented in Figure 1.
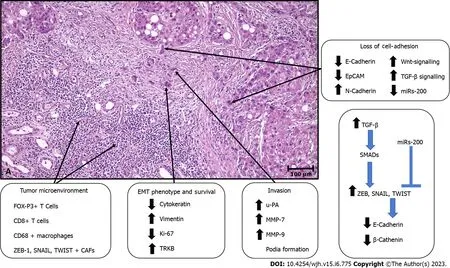
Figure 1 Tumor budding in primary liver cancers.A: Tumor budding consisting of small clusters of 4 or fewer tumor cells present at the invasive edge in a case of hepatocellular carcinoma; B: The main processes and mechanisms involved in tumor budding.EMT: Epithelial to mesenchymal transition; EpCAM: Epithelial cell adhesion molecule; CAFs: Cancer-associated fibroblasts; MMP: Matrix metalloproteinase; TRKB: Tyrosine kinase receptor B; u-PA: Urokinase plasminogen activator.
The epithelial-mesenchymal transition (EMT) program, which contributes to developmental events throughout embryogenesis, has been hypothesized to play a fundamental role in TB formation, particularly in the steps of cell dissociation and cell migration[10-14].Indeed, accumulating evidence indicates that budding tumor cells might display the properties of cells undergoing EMT to acquire more invasive and migratory capacity.
E-cadherin, an essential cell-cell adhesion protein, plays a pivotal role in cellular dissociation.Therefore, the reports indicating a decrease or loss of expression of E-cadherin in the invasive margin and bud areas in many solid organ tumors, including esophageal, colon, pancreas, endometrial, and oral cancers, are not surprising[15-18].In addition, the increase in the expression of EMT-related transcription factors in tumor buds that suppress the expression of this protein, including ZEB1, ZEB2,TWIST1, TWIST2, SNAI1 (SNAIL), and SNAI2 (SLUG), is also noted in many malignancies[17-19].Recently, an increase in the expression of these transcription factors and a decrease in E-cadherin and bcatenin levels in tumor buds compared to tumor bulk have been observed in pancreatic and oral cancers[17,18].In addition, it has been suggested that the decrease in β-catenin expression parallel to that of Ecadherin may be a finding of WNT-b-catenin signaling pathway activation in tumor buds[20-22].
Moreover, data have also shown that TGFβ signaling activation in buds can induce transcriptional repression of E-cadherin by inducing E-cadherin repressors, such as ZEB, TWIST, and SNAIL,viaderegulation of SMADs[18,23].However, the observation that different subtypes of EMT transcription factors are increased in some tumors highlights that not all of them should be expected to be increased together in tumor buds[24].It has been shown that both E-cadherin and molecules such as CD44 and EpCam are lost in TB areas[25-27].Signature changes in some miRNAs have also been shown to contribute to TB.In particular, changes in the miR-200 family have been noted[28-31].The levels of miR-200, which has a suppressive effect on the ZEB family that induces E-cadherin expression, were significantly decreased in tumor buds of colorectal and pancreatic ductal adenocarcinoma[32,33].
In TB, the effect of EMT is not limited to cell dislocation; moreover, it significantly affects cell migration through cytoskeletal reorganization, increased cell-associated proteolytic activity, and reprogramming of gene expression[34].Recently, many studies have shown that these changes are found in budding tumor cells, and marked differences in the expression of genes involved in integrinmediated cell adhesion, cell migration, cytoskeletal changes, and extracellular matrix degradation have been noted[35].
A monomeric form of laminin 5 gamma 2, which plays a role in the anchorage of epithelial cells to the underlying basement membrane, has been found to increase during tumor invasion and in tumor buds[35,36].This finding was associated with aggressive tumor behavior, especially in pulmonary[37,38] and colorectal cancers[39-42].Moreover, in the latter, the dendritic extensions of budding tumor cells are positive for laminin 5 gamma 2, which is associated with vascular invasion[43,44].In addition, in line with the findings that β-catenin induces gene expression of this protein by binding to TCF and LEF family transcription factors, decreased membranous β-catenin levels, increased nuclear β-catenin levels,positivity for laminin 5 gamma 2, and decreased E-cadherin expression were associated with TB[40,45].These data indicate that altered expression of β-catenin may participate in multiple events in TB.In addition, other cell migration markers, including motility class III β-tubulin and high-mobility Group A family proteins, are more abundant in invasive and TB sites[46,47].Furthermore, the expression of proteins such as matrix metalloproteinase 7, matrix metalloproteinase 9 urokinase plasminogen activator and cathepsin B, which degrade the matrix of cells, was found to be significantly increased in tumor buds[41,48-50].In this region, various metastasis suppressors (such as rapidly accelerated fibrosarcoma kinase inhibitor protein and maspin) are frequently disrupted and/or downregulated in tumor buds compared to the primary tumor mass[51-54].
The survival of malignant cells in the tumor bud largely depends on their adaptation to a hypoxic environment.Studies have shown that these cells overexpress TRKB, a marker of resistance to cell death, and hypoxia-inducible factor 1α[55,56].In addition, cells in tumor buds have either shallow levels or the absence of proliferation markers (such as Ki-67)[57,58].These findings support the view that cell proliferation and migration are mutually exclusive processes and that the transition from cell proliferation to invasion may be triggered by hypoxia.Moreover, the fact that budding tumor cells frequently overexpress stem cell markers, such as LGR5, ALDH1, and CD44, suggests the self-renewal capacity of these cells, including those at metastatic sites[26,59-62].
There are also data showing that T cells in the peritumoral stroma (CD8+ T cells and FOXP3+ T cells)[63-65], EMT marker-positive cancer-associated fibroblasts[66-68], the engulfment of budding tumor cells by CD68+ macrophages, and the loss of MHC class I expression may play roles in TB[69-71].
From a morphological point of view, TB is defined as small clusters of 4 or fewer tumor cells at the interface of invasive carcinoma.Although different methods are performed, TB is usually evaluated by determining the most invasive area of the tumor (hot spot) at 20x magnification on hematoxylin and eosin-stained slides.Regardless of tumor type, buds in these areas are counted, and according to the recommendation of TBCC, TB is classified into three grades: Low, intermediate, and high[7].
In the context of HCC and ICC, there is evidence from numerous studies focusing on the mechanisms involved in TB outlined above.Among these, it is noteworthy that the number of studies focusing on the EMT in primary liver tumors is over 200 per year[10,11].
This is not surprising, given the considerable roles of the EMT in tumor behavior and progression[72-74].Accordingly, the number of studies aiming to detect tumor aggression using comprehensive immunohistochemical and molecular methods far exceeds the number of studies focusing on TB, which can be easily detected as a simple, cost-effective morphological finding from resection materials.
TB IN HCC
Unfortunately, according to the literature, there are very few studies on the relationship between TB and tumor behavior and prognosis in HCC (Table 1).Kairaluomaet al[75] studied the prognostic value of TB, including 259 patients with HCC, in a retrospective cohort study from a single institution.TB is evaluated according to the hot spot method, which is recommended when investigating TB in CRC.The overall 5-year survival in bud-negative patients was higher (72.1%) than that in bud-positive patients(29.2%) (P= 0.009).In addition, the difference between the disease-specific 5-year survival rates of these two groups was also significant, 86.5% (in bud-positive patients)vs35.1% (in bud-negative patients) (P= 0.002).Multivariate analysis demonstrated that TB is an independent prognostic factor in surgically treated cases.
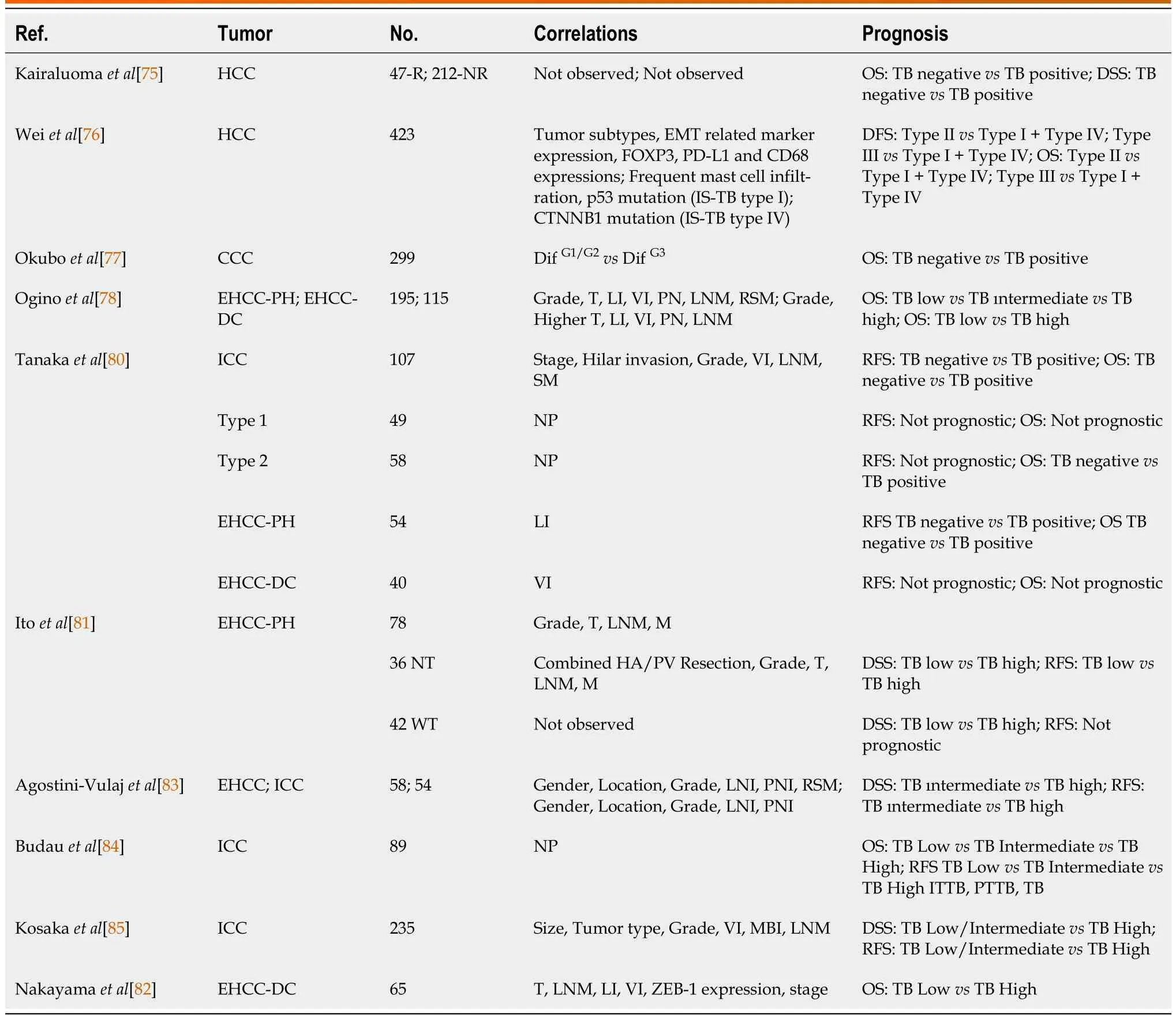
Table 1 Relationship of tumor budding with clinicopathologic parameters and survival in hepatocellular and cholangiocarcinomas
However, this parameter was not correlated with clinicopathological factors.This is the only study investigating TB in HCC in a Western population, although it had some limitations, as noted by the authors.There were relatively few patients, yielding wide confidence intervals in the surgical cohort.Additionally, instead of looking for the optimal threshold value, the analysis was performed by making a negative/positive distinction in TB.Again, the absence of significant results in biopsy samples warrants further studies.
Another study was performed in China by Weiet al[76] to classify HCC based on TB and immune scores in 423 patients.The authors developed a prognosis-relevant immune score based on five types of immune cells.A classification based on TB grade and immune type was established (IS-TB type).To explore the association between IS-TB type and molecular alterations of HCC, tumor samples and adjacent nontumor tissues from 100 patients were investigated by whole-exome sequencing.TB was classified into three grades.In addition, cases were also divided into high-grade TB (with ≥ 10 buds) and low-grade TB (with 0 to 9 buds) groups.TB was an independent prognostic indicator for overall survival (OS) and disease-free survival (DFS) in the training and validation cohorts.They also observed that high-grade TB was significantly associated with EMT markers and had higher incidences in patients with nonsteatotic, nonfibrolamellar HCC, stromal active (high α-SMA expression), and immature tumors.A link between TB and EMT markers (E-cadherin and vimentin) confirmed the hypothesis that TB might represent the EMT process.
Because the role of the immune milieu of HCC as a prognostic feature is only starting to emerge, they also divided cases by an immune score established based on Z scores that included five parameters(CD8 stromal, PD-L1 stromal, mast-cell stromal, CD68 stromal, and FOXP3 stromal) for each patient.According to the cutoff value (0.04), patients were divided into immune type A and B groups.DFS and OS were better in the type A group than in the type B group in both the training and validation cohorts.The combination of TB grade and immune type cases was also divided into four groups: ISA-TBhigh(type I), ISB-TBhigh(type II), ISA-TBlow(type III), and ISB- TBlow(type IV).While cases within IS-TB type II showed the worst long-term survival, cases within IS-TB type III had the best OS and DFS.These findings are in line with previous observations that indicated that a high lymphocyte-to-TB ratio was a good prognostic factor and that the integration of both TILs and TB was advantageous in the prediction of long-term prognosis in colorectal cancers.These findings provide a rationale for the pathologicalevaluation of the TME in addition to the current pathological classifications of HCC.
Another interesting finding of this study was the association between IS-TB type and molecular alterations.TP53 (mainly within IS-TB type I) and CTNNB1 (mainly within IS-TB type IV) mutations in two distinct HCC phenotypes exhibit different immune and pathological characteristics.While TP53 mutations were related to poor differentiation and a thick trabecular pattern, CTNNB1 mutations were associated with impaired antitumor immunity (immune type B), well-differentiated morphology, a pseudoglandular pattern, mature stroma, and low α-SMA (fibroblast activation protein) expression.
As noted above, despite the scarcity of studies examining TB in HCC, there is a wealth of data on the processes involved in this phenomenon.
TB IN CHOLANGIOCARCINOMA
Several studies focusing on TB in cholangiocarcinomas have recently been performed.The number of studies, including extrahepatic perihilar (EHCC-PH) and distal cholangiocarcinoma (EHCC-D) cases,exceeded the number of studies that included ICC cases in the study group.The characteristics and results of these studies are summarized in Table 1.
In an earlier investigation of cholangiocarcinomas from all anatomical locations (CCC), TB was associated with the grade but not with the course of the disease[77].However, in a more recent study, in addition to high grade, high TB was more frequently observed in males and patients with extrahepatic localization, perineural and lymphatic invasion, and presentation in settings with positive resection margins[78].Moreover, TB is an independent prognostic factor for CCC.However, since TB scoring differed in these two studies, it is not possible to compare the results of one with the other (Tables 1 and 2), as noted by Regmiet al[79], who performed a meta-analysis of CCC samples from different locations,including tumors of the ampulla and gallbladder.
In EHCC-PH, TB is associated with tumor invasion, lymph node metastasis, perineural invasion,lymphovascular invasion, and positive resection margin status.It has also been shown to be an independent prognostic factor in determining the course of the disease in all of the studies[78,80,81].In EHCC-D, higher TB was more frequent in tumors with deeper invasion, lymph node metastasis, and lymphovascular and perineural invasion[78,80,82].The correlation between TB and stage and ZEB-1 expression was also noted[83].Similar to EHCC-P, all but one study[81] showed that TB effectively determines the course of the disease, as shown by both univariate and multivariate analyses[77,78,81-84].
Regarding ICC, TB was shown to be correlated with stage, hilar invasion, grade, venous invasion,lymph node metastasis, and positive surgical margins, which are important parameters for determining the behavior of these tumors.Moreover, when ICCs were analyzed according to growth patterns, it was noted that 80% of mass-forming tumors had high TB.In contrast, this ratio was 16% and 2.3% in periductal infiltrating and intraductal growing subtypes, respectively[85].In addition, the prognostic role of TB has been described[77,80,81,85].Budauet al[84] analyzed TB using a three-tier grading system: high, intermediate, and low.While patients with low TB had the most favorable recurrence survival, high TB was associated with the most unfavorable outcomes.
Similarly, TB correlated significantly with the overall survival of patients in univariate and multivariate analyses (P< 0.001).In addition, their data demonstrated that in ICC, TB is significantly independent of the area of investigation (intratumoral or peritumoral).These findings indicate the possibility that TB assessment in preoperative tissue biopsies and in cases that would not be suitable for resection could be used to predict tumor behavior.Nevertheless, the evidence for intratumoral TB is still weak.
In another study, TB was observed to be a powerful prognostic factor for RFS and OS in ICC[80].In patients stratified into negative and positive TB status, the median time to recurrence in cases with positive TB was 10.26 mo.This was significantly shorter than that of subjects with negative TB (35.57 mo), and the difference among median survival times was significant (P< 0.001).Furthermore, the results of the same study indicated that TB was a decisive and powerful prognostic factor for OS (HR:4.547).Although these findings need to be supported by further large-scale studies, they suggest that TB may be an important prognostic parameter in these tumors.
Tanakaet al[80] presented an interesting finding about TB in ICC in an elegant study.When they evaluated TB by dividing ICC into two subgroups, Type 1 (hilar) and Type 2 (peripheral), according to the combined scores of mucin productivity and immunoreactivity of S100P, N-cadherin, and neural cell adhesion molecule, this parameter was determined to be a decisive prognostic factor in Type 2 but not in Type 1.They suggested that some differences exist in the biological behavior of these subtypes and pointed out that despite the prognostic importance of TB in ICC, its pathogenetic role in biliary tract carcinomas might differ by anatomic location.However, this finding needs to be supported in further studies.Nevertheless, the results of TB studies in ICC are similar and support the suggestion that TB is a relevant prognostic factor in the histopathological evaluation of these tumors.
Generally, different scoring methods have been used to investigate TB in cholangiocarcinomas.In a few studies, unlike the recommendation of TTBC, five cells were taken as the cutoff for the definition of TB[77,78,81].The analyses were performed by categorizing the cases as negative vs.positive or low vs.high TB.In most other studies, including ICC cases, patients were assessed following the three-tiered system recommended by the TTBC for colorectal cancer[80,82-84].However, different stratifications were used for further evaluations (Table 2).More recently, in an elegant study, Zlobecet al[86] observed that CRC without TB (TB0) is relatively frequent and provided additional information on tumor behavior, suggesting a new “zero budding”category for TB.There is currently no evidence about the prognostic value of TB0 in cholangiocarcinomas, and it would be interesting to conduct further studies in which this category is addressed separately.

Table 2 Criteria applied for tumor budding in previous studies
Accumulated data indicate that the preferred staining method for scoring TB is HE.Recently, some studies on TB have reported that IHC is superior to HE regarding reproducibility and interobserver agreement in assessing this parameter in CRC.Regarding CCC, Oginoet al[78] obtained TB scores in HE-stained whole-tissue sections and PanCK immunostained tissue microarray (TMA) sections from 266 patients.They observed that the number of tumor buds in HE-stained slides was almost equal to that in PanCK-stained slides from TMA, with a strong correlation between them (R= 0.763,P< 0.001).This finding also supports that evaluating TB in HE-stained sections is a simple and reproducible method.Nevertheless, more studies are needed to standardize the assessment of TB in ICC because grading systems for this parameter vary between different types of cancer.
In CRC, TB, combined with other established biomarkers, may allow us to discriminate between patients who would benefit from oncological resection and patients who will receive adjuvant therapy and to classify different therapeutic options, especially in advanced-stage patients[87].Thus, TB can predict prognosis and regulate treatment options in primary liver cancers.However, the role of TB in the treatment of these tumors remains to be investigated.
CONCLUSION
This review highlights that TB may be a promising prognostic factor for primary liver tumors.However,its clinical value in managing patients should be established in multidisciplinary studies.Evidence also suggests that TB in HCC can identify and reclassify tumors of molecular subtypes with different behavioral characteristics.The differences in the classification of TB in primary liver tumors indicate that a standard and validated method should be established to provide a solid basis for large-scale clinicopathological studies for further evaluation.In addition, the precise determination of the value of budding tumor assessment with multiple further studies may allow us to clarify whether this parameter will be included in pathology report protocols as in CRC in the near future.
FOOTNOTES
Author contributions:Celik MY, Gedik EO, Unal B performed the data acquisition; Bassorgun CI, Unal B and Elpek GO designed the outline and coordinated the writing of the paper; all authors equally contributed to the writing of the paper and preparation of the tables and illustrations.
Conflict-of-interest statement:The authors have no conflicts of interest related to this publication.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Turkey
ORCID number:Betul Unal 0000-0001-7680-1808; Mennan Yigitcan Celik 0000-0001-8769-5156; Elif Ocak Gedik 0000-0003-2618-498X; Cumhur Ibrahim Bassorgun 0000-0003-2440-511X; Gulsum Ozlem Elpek 0000-0002-1237-5454.
Corresponding Author's Membership in Professional Societies:European Society of Pathology, No.11959.
S-Editor:Ma YJ
L-Editor:A
P-Editor:Yuan YY
1Global Cancer Observatory, Lyon, France: International Agency for Research on Cancer, 2018.Accessed: November 22,2018.Available from: http://gco.iarc.fr/today/
杂志排行
World Journal of Hepatology的其它文章
- Ductular reaction in non-alcoholic fatty liver disease: When Macbeth is perverted
- Recent advances in pathophysiology, diagnosis and management of hepatorenal syndrome: A review
- Treatment of liver fibrosis: Past, current, and future
- Role of vascular endothelial growth factor B in nonalcoholic fatty liver disease and its potential value
- Acute pancreatitis in liver transplant hospitalizations: Identifying national trends, clinical outcomes and healthcare burden in the United States
- Lower alanine aminotransferase levels are associated with increased all-cause and cardiovascular mortality in nonalcoholic fatty liver patients
