Effectiveness of moxibustion alone on lumbar disc herniation: a Meta-analysis of randomized controlled trials
2023-02-15YAOYaoZHAOZhenniCHENFengqinLENGYufeiPANGXiangtianXUXiaoSUNZhiling
YAO Yao,ZHAO Zhenni,CHEN Fengqin,LENG Yufei,PANG Xiangtian,XU Xiao,SUN Zhiling
YAO Yao,ZHAO Zhenni,PANG Xiangtian,SUN Zhiling,School of Nursing,Nanjing University of Chinese Medicine,Nanjing 210023,China
CHEN Fengqin,Office of Academic Affairs,Nanjing Normal University of Special Education,Nanjing 210038,China
LENG Yufei,Auxiliary Teaching Center,Shanghai Jiao Tong University School of Medicine,Shanghai 200025,China
XU Xiao,School of Nursing,Zhejiang Chinese Medical University,Hangzhou 310053,China
Abstract OBJECTIVE: To evaluate the available evidence from randomized controlled trials (RCTs) of moxibustion alone for lumbar disc herniation (LDH) treatment.METHODS: A systematic search of 10 databases (until August 30,2021) was used to identify studies that reported the response rate,visual analogue scale (VAS)score,Japanese Orthopedic Association (JOA) score,and Oswestry Disability Index (ODI) score.Study selection and data extraction were independently performed by two reviewers.Cochrane criteria for risk of bias were used to assess the methodological quality of the trials.The Grading of Recommendations Assessment,Development,and Evaluation Methodology (GRADE)were also used to test the quality of the result evidence.RESULTS: Nineteen RCTs,including 1888 patients,met the inclusion criteria.Five studies showed no difference between moxibustion and acupuncture on response rate[risk ratio (RR)=1.07,95%CI (0.98,1.16),P=0.11].Meanwhile,six studies suggested that there is no significant difference between moxibustion and acupuncture on VAS score [mean difference (MD)=-0.43,95% CI (-0.91,0.05),P=0.08].Eight studies implied that there is no significant difference between moxibustion and acupuncture on JOA score [MD=0.84,95% CI (-1.27,2.96),P=0.44].Two studies indicated that moxibustion may have equivalent effects for treating LDH in the VAS score in comparison with drug therapy[MD=-1.16,95%CI (-2.63,0.31),P=0.12].The evidence level of results was determined to be very low to low.CONCLUSIONS: Based on the existing evidence,moxibustion may not be suitable for treating LDH alone,but it may be applied as an adjuvant treatment.Furthermore,well-designed RCTs with high quality and larger samples are still needed to evaluate the efficacy and safety of moxibustion alone for LDH treatment.
Keywords: moxibustion;lumbar disc herniation;randomized controlled trial;systematic review;Meta-analysis
1.INTRODUCTION
Lumbar disc herniation (LDH),which is characterized by low back pain,numbness,and pain of lower limbs,is a common disease in orthopedics.At present,the incidence of LDH is 20%-30%.1Considering changes in lifestyle,the prevalence of LDH has increased dramatically to the extent in which young people are experiencing it as well.2LDH has also affected the quality of life of patients and increased the economic burden of the social health care system.3At present,the majority of patients with LDH undergo non-surgical treatment,4and 80%-90% receive mild rehabilitation after conservative treatment (nonsurgical treatment).5
Notably,non-surgical treatment in Western Medicine primarily uses oral non-steroidal anti-inflammatory drugs and epidural steroid injection,which may be only marginally effective for short-term relief of pain with potentially long-term side effects,such as hepatic and renal toxicity and gastrointestinal discomfort.6In addition,the cost-effectiveness of this type of treatment is unclear.7Meanwhile,Traditional Chinese Medicine(TCM) has attracted increasing attention because of its superior effect and minimal side effects.8As a TCM external treatment,moxibustion is considered as a major TCM therapy together with decoction and acupuncture,and it is widely used because of its convenience,efficacy,and cheapness.Moxibustion has become an important method for the treatment of LDH,and its curative effect is remarkable.9
In particularly,it is important to systematically assess and meta-analyze the effect of moxibustion for LDH.In evaluating the efficacy and safety of moxibustion for LDH treatment,a systematic review10has included trials using moxibustion combined with other western or TCM therapies as the intervention method in the experimental group.However,it fails to assess the efficacy of moxibustion alone for treating LDH.With the widespread use of moxibustion,its effect has also received attention.However,a systematic review or meta-analysis that assesses the efficacy of moxibustion alone on LDH is lacking.Therefore,this study aims to critically assess the efficacy and safety of moxibustion without combining with other therapies in treating LDH.
2.METHODS
This Meta-analysis was performed on the basis of the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines.11
2.1.Data sources
A systematic literature search was used in the following databases from their inception to August 30,2021,with no restrictions on language and publication: the Cochrane Library,Web of Science,PubMed,EMBASE,EBSCO,the China National Knowledge Infrastructure(CNKI),Wanfang data,Oriental Medicine Advanced Searching Integrated System (OASIS),National Discovery for Science Leaders (NDSL),and Japan Science and Technology Information Aggregator,Electronic (J-STAGE).These searches were performed using the following keywords: “lumber disc herniation,”“lumbar disc herniation,”“lumbar disc protrusion,”“LDH,”“intervertebral disc displacement,”“moxibustion,”“moxibustion therapy,”“moxibustion,”“moxa,”“random,”“randomly,”“randomized controlled trial,” and “placebo.” The search strategies for the abovementioned 10 databases are shown in Appendix S1.For a comprehensive search,the references of included articles and relative reviews were manually searched.Two investigators independently searched and imported the identified literature into the EndNote software to delete duplications,and they selected potential articles by reviewing the titles and abstracts.The full texts of the selected articles were assessed on the basis of the inclusion and exclusion criteria.
2.2.Inclusion criteria
The included studies were published randomized controlled trials with parallel design,including those in the form of dissertations and conference papers.
P (population): Patients with LDH regardless of gender,age,ethnicity,education,and economic status who meet the diagnostic criteria were included in the study.12-14
I (intervention): trials that compared moxibustion with any other treatment were included.Studies of moxibustion combined with other therapies were excluded.
C (comparison): trials that compared moxibustion with any intervention method in control group were included.O (outcomes): the outcome included the total response rate,which was based on diagnostic and therapeutic criteria for diseases and syndrome patterns of TCM or the guiding principle of clinical research on new drugs of TCM.12,13In addition,the visual analog scale (VAS)score served as an outcome measurement in this review,15which was used for a total of 0-10 points,where 0-10 indicates different degrees of pain,0 indicates no pain,and 10 indicates maximum pain.Meanwhile,the Japanese Orthopedic Association (JOA) back pain evaluation questionnaire was included.16It is used to assess pain,the ability to conduct daily life and work,functional impairment,and particular clinical examinations.In addition,the other outcome measures included the Oswestry Disability Index (ODI),17which is a questionnaire survey and assessment method for each of the nine aspects,including lifting,walking,sitting,standing,pain intensity,self-care,sleep disturbance,social life,and travel.
2.3.Data extraction
Two reviewers (CHEN Fengqin and YAO Yao)independently performed data extraction based on predefined criteria,including the authors,publication date,sample size,population information,intervention regimens,follow-up duration,outcomes,and adverse events.In the case of insufficient data,we would send an e-mail to the author requesting for more information.
2.4.Risk of bias assessment
The risk of bias was determined by two independent reviewers (ZHAO Zhenni and YAO Yao) in accordance with the Cochrane Handbook for Systematic Reviews of Interventions,18,19and it included the following items: (a)random sequence generation (selection bias),(b)allocation concealment (selection bias),(c) blinding of participants and personnel (performance bias),(d)blinding of outcome assessment (detection bias),(e)incomplete outcome data (attrition bias),(f) selective reporting (reporting bias),(g) and other bias.The evaluation of these items was rated as “low,”“high,” or“unclear.” Divergence was resolved through discussion.If two reviewers were unable to reach an agreement,then the third and fourth reviewers (SUN Zhiling and XU Xiao) were consulted for a final decision.
2.5.Statistical analysis
Meta-analysis was performed using RevMan 5.3.Dichotomous outcomes were reported as risk ratio (RR)and continuous data as weighted mean difference(WMD).Notably,χ2test andI2test were utilized to measure the heterogeneity among studies.A fixed-effect model was adopted ifI2< 50% andP> 0.1;otherwise,a random-effects model was used.When the clinical heterogeneity between the two studies was substantial,only descriptive analysis was performed.The potential publication bias was tested by using an inverted funnel chart when the number of RCTs in meta-analysis was more than 10.In addition,the causes of heterogeneity were identified,and the leave-one-out method was used for sensitivity analysis.19If high heterogeneity still could not be explained,then the results should be carefully interpreted.Sensitivity analysis was performed using STATA 16.0 software (Stata Corp.2019,College Station,TX,USA).
The quality of the evidence for each outcome was assessed on the basis of the Grading of Recommendations Assessment,Development,and Evaluation (GRADE)software.Detailed GRADE guidance was used to evaluate the risk of bias,imprecision,inconsistency,indirectness,and publication bias,thereby downgrading the level of evidence.20,21The level of evidence can be upgraded in case of a large effect size,evidence of doseresponse gradient,or all plausible confounding factors reducing an apparent effect.Two reviewers (LENG and PANG) separately conducted assessment.Any disagreement was resolved through discussion and consultation with a third author (SUN) until a consensus wasreached.We described the quality of evidence as follows:High-quality evidence: consistent findings were obtained among at least 75% of trials with no limitations of study design,consistency,direct and precise data,and known or suspected publication biases.We are confident that the real result is close to the estimation of the effect.
Moderate-quality evidence: one of the domains is not met.We have some confidence in the estimation of the effect.The true effect is likely close to the estimation of the effect,but it may also be substantially different.
Low-quality evidence: two of the domains are not met.Our confidence in the effect estimate is limited.The true effect may be substantially different from the estimate of the effect.
Very-low-quality evidence: three of the domains are not met.We have very little confidence in the effect estimate.The true effect is likely to be substantially different from the estimate of effect.
No evidence: no trials were identified that addressed this outcome.
3.RESULTS
3.1.Study selection
A total of 1422 potential studies were identified through an initial database search.After removing 645 duplicates and 680 articles by screening title and abstract,97 fulltext articles were downloaded and assessed.Of these articles,78 were excluded for failing to satisfy the inclusion criteria.Finally,19 RCTs with 1888 participants were included for systematic review.22-40A flow chart of the study selection process is presented in Figure 1.
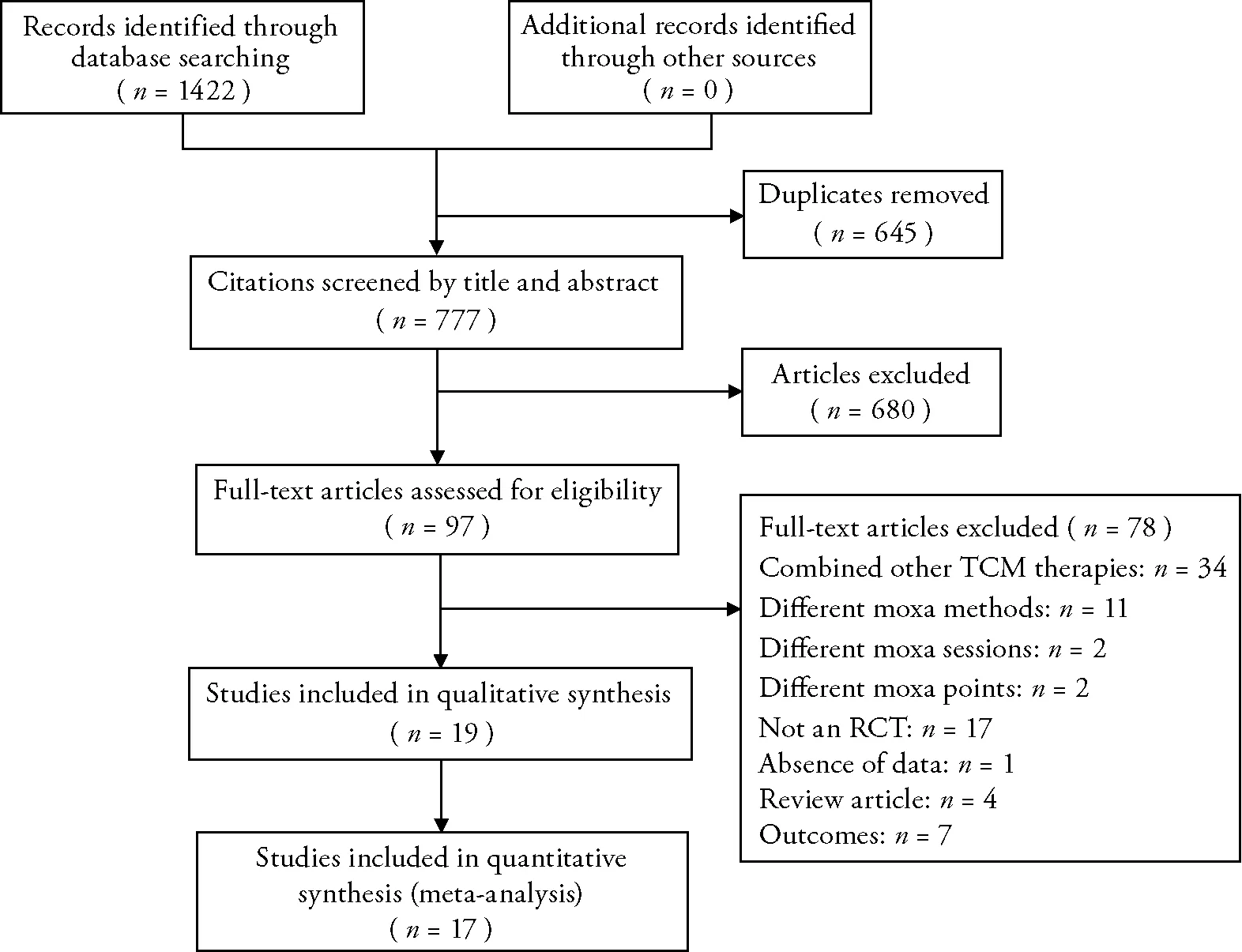
Figure 1 Flowchart of the study selection process
3.2.Study characteristics
All included trials were conducted in China.The sample sizes ranged from 40 to 456.Four RCTs adopted a threearm parallel group design,25,33,37,38and 15 trials used a two-arm parallel group design.
Intervention is different from group.The experimental groups were treated with moxibustion alone.In the control groups,interventions included drug therapy,25,26,37,38,40conventional therapy,22,23acupuncture,25,27-36acupuncture plus TDP irradiation,39and fixed-point rotation reduction.24The characteristics of the participants,intervention details,adverse events,and outcome measures are presented in Table 1.
3.3.Risk of bias
Based on the Cochrane criteria,the risk of bias assessment is presented in Figure 2.Among 19 studies,15 trials utilized a random table for randomization,24-28,30,32-40and the other four trials did not provide the methods of sequence generation.22,23,29,31Only one reported trial used a central randomization system to conduct allocation concealment,38whereas the remainder did not provide concealment methods.One trial mentioned single blindness,but it did not specify who was blinded,31and one trial used the blindness of the assessor.38Two studies mentioned dropouts without detailed information of handling.31,36
3.4.Subgroup analysis
Of the 19 studies,seven trials used response rate;nine studies used the VAS score;13 trials used the JOA score,and three trials used ODI to evaluate the effects of moxibustion for LDH.
3.5.Response rate
Seven RCTs reported response rates for moxibustion as the outcome measurement.24,25,28,30,31,36,39Given the clinical heterogeneity,subgroup analysis was performed on the basis of different control interventions.In addition,five trials compared moxibustion with acupuncture and demonstrated no significant difference between these two interventions [RR=1.07,95%CI(0.98,1.16),P=0.11,I2=0%].25,28,30,31,36A single trial implied that no statistical significance of moxibustion was observed in improving the response rate compared with drug therapy[RR=1.26,95%CI(1.00,1.58),P=0.05].25One trial suggested that moxibustion had no statistically significant effects on the response rate compared with acupuncture plus TDP irradiation [RR=1.08,95%CI(0.97,1.21),P=0.17].39Another single trial indicated that moxibustion had no statistical significance on the response rate compared with fixed-point rotation reduction [RR=1.22,95%CI(1.00,1.49),P=0.05].24By contrast,the overall results suggested that moxibustion had a marked beneficial effect in improving the response rate when compared with four different treatments [RR=1.11,95%CI(1.04,1.19),P=0.001,I2=0%] without high heterogeneity (Figure 3A).
Furthermore,subgroup analysis was conducted on the basis of the definition of the response rate.Here,six RCTs utilized the diagnostic and therapeutic criteria for diseases and syndrome patterns of TCM to evaluate the response rate.24,28,30,31,36,39In comparison to the control interventions,subgroup analysis results revealed that moxibustion had significantly favorable effects in improving the response rate [RR=1.10,95%CI(1.02,1.18),P=0.01,I2=0%].Meanwhile,one trial with two groups utilized the guiding principle of clinical research on new drugs of TCM to assess the response rate.25Compared with the control interventions,moxibustion had a significantly better overall effective rate [RR=1.17,95%CI(1.02,1.35),P=0.03,I2=2%].In general,metaanalysis indicated no significant differences between these two criteria in evaluating the response rate (Figure 3B).
3.6.VAS score
Nine RCTs utilized the VAS score as a measure of the effects for LDH treatment.23-25,27,29,30,34,35,40Meanwhile,six studies reported equivalent effects in reducing pain between moxibustion and acupuncture [MD=-0.43,95%CI(-0.91,0.05),P=0.08,I2=91%].25,27,29,30,34,35Two trials exhibited equivalent effects of moxibustion compared with drug therapy for the VAS score [MD=-1.16,95%CI(-2.63,0.31),P=0.12,I2=96%].25,40Notably,one RCT showed superior effects of moxibustion on pain reduction compared with conventional therapy [MD=-0.64,95%CI(-0.87,-0.41),P<0.000 01].23In addition,a single trial indicated that moxibustion had a significant pain relief effect on LDH compared with fixed-point rotation reduction [MD=-1.05,95%CI(-1.22,-0.88),P< 0.000 01].24The overall results indicated that moxibustion can significantly relieve pain when compared with four different treatments [MD=-0.70,95%CI(-0.99,-0.41),P<0.000 01,I2=90%] with severe heterogeneity (Figure 3C).
3.7.JOA score
Thirteen RCTs adopted the JOA score as a measure to assess the effects of a particular therapy on improving LDH,24,26-30,32-35,37,38,40and the heterogeneity among these studies was also high.Subgroup analysis suggested that moxibustion had no significantly favorable effects with regard to the JOA score compared with acupuncture [MD=0.84,95%CI(-1.27,2.96),P=0.44,I2=90%].In comparison with drug therapy,moxibustion had no statistical significance in improving the JOA score [MD=4.15,95%CI(0.05,8.26),P=0.05,I2=96%].Moreover,a single trial indicated that moxibustion had statistically significant favorable effects on the JOA score in comparison with fixed-point rotation reduction [MD=8.69,95%CI(5.08,12.30),P< 0.000 01].24The pooled results indicated that moxibustion had no statistically significant favorable effects on the JOA score when compared with the three different treatments [MD=2.08,95%CI(-0.08,4.24),P=0.06] (Figure 3D).In particular,two trials were not included in Meta-analysis,whose outcomes were measured using a modified edition of the JOA score.37,38One trial demonstrated that moxibustion had significantly favorable effects in improving the JOA score compared with drug therapy plus acupuncture.38Another study also illustrated that moxibustion immensely improved the status of patients suffering from LDH compared with drug therapy plus acupuncture.37


3.8.ODI
Three RCTs adopted ODI as an outcome.22,24,25In comparison with acupuncture,the subgroup analysis results revealed equivalent effects of moxibustion in improving the ODI score [MD=-1.16,95%CI(-3.75,1.43),P=0.38].In addition,moxibustion had better efficacy in relieving dysfunction caused by LDH compared with drug therapy,conventional therapy,and fixed-point rotation reduction.In general,the Meta-analysis results significantly demonstrated the superior effect of moxi-bustion on the ODI score compared with control inter-ventions with high heterogeneity [MD=-8.78,95%CI(-12.73,-4.83),P< 0.0001,I2=94%] (Figure 3E).

Figure 2 Risk of bias graph and summary
3.9.Adverse effects
Of the 19 included studies,three studies reported adverse events,whereas 16 did not mention any adverse events.Two trials stated that moxibustion had no adverse events.28,38One trial reported five patients who developed dry and thirst in the moxibustion group but returned to normal after hydration.26
3.10.Sensitivity analysis
Sensitivity analysis was conducted to evaluate the robustness of Meta-analysis by using STATA 16.0 (Stata Corp.2019,College Station,TX,USA).Given the heterogeneity of intervention comparison,we conducted sensitivity analysis on the results of each subgroup but not on the subgroups with only 1 to 2 studies.Sensitivity analysis was presented in the form of forest maps (Figure 4).All studies were within reasonable intervals,and sensitivity was acceptable.
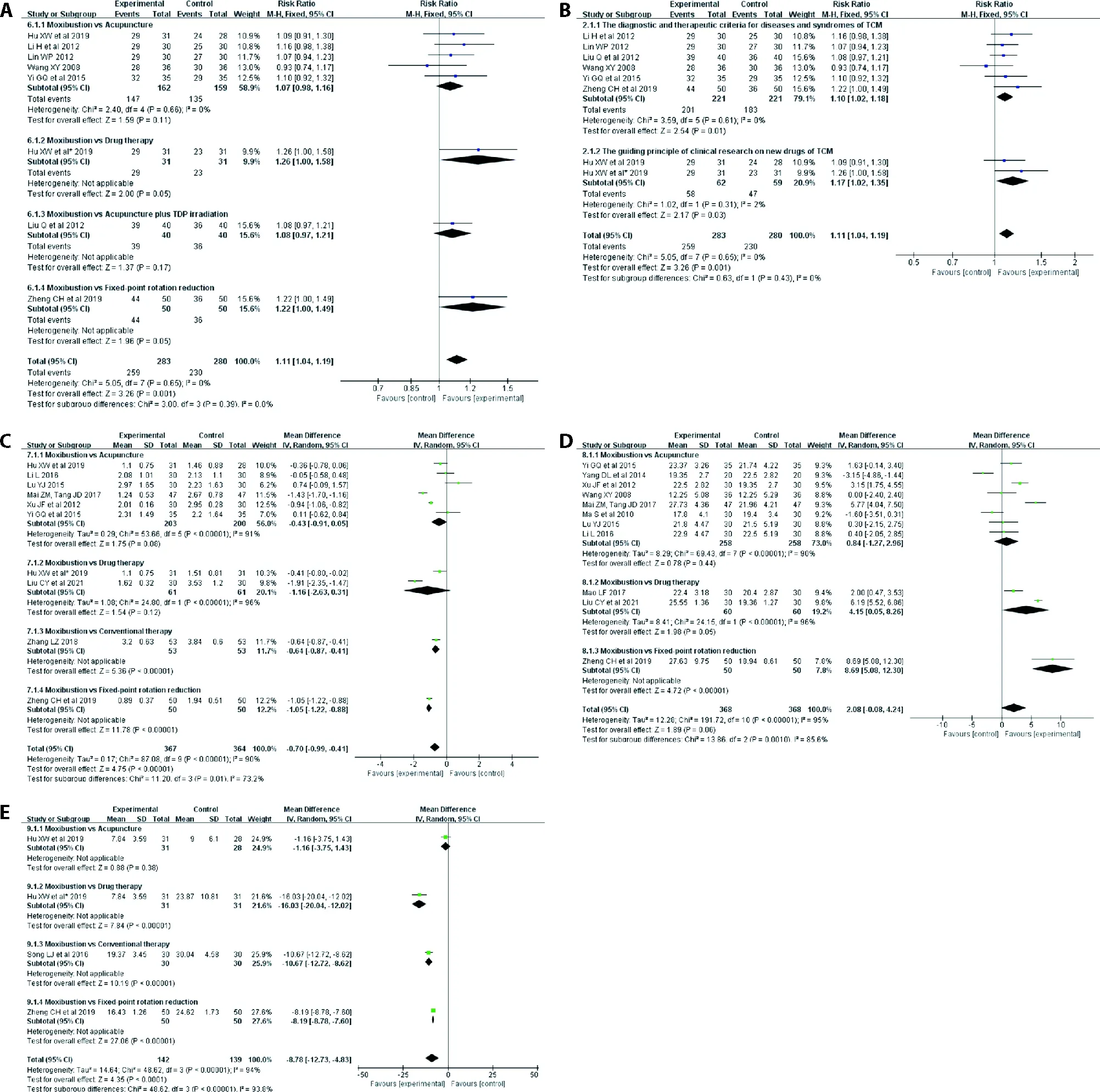
Figure 3 Results of the Meta-analysis
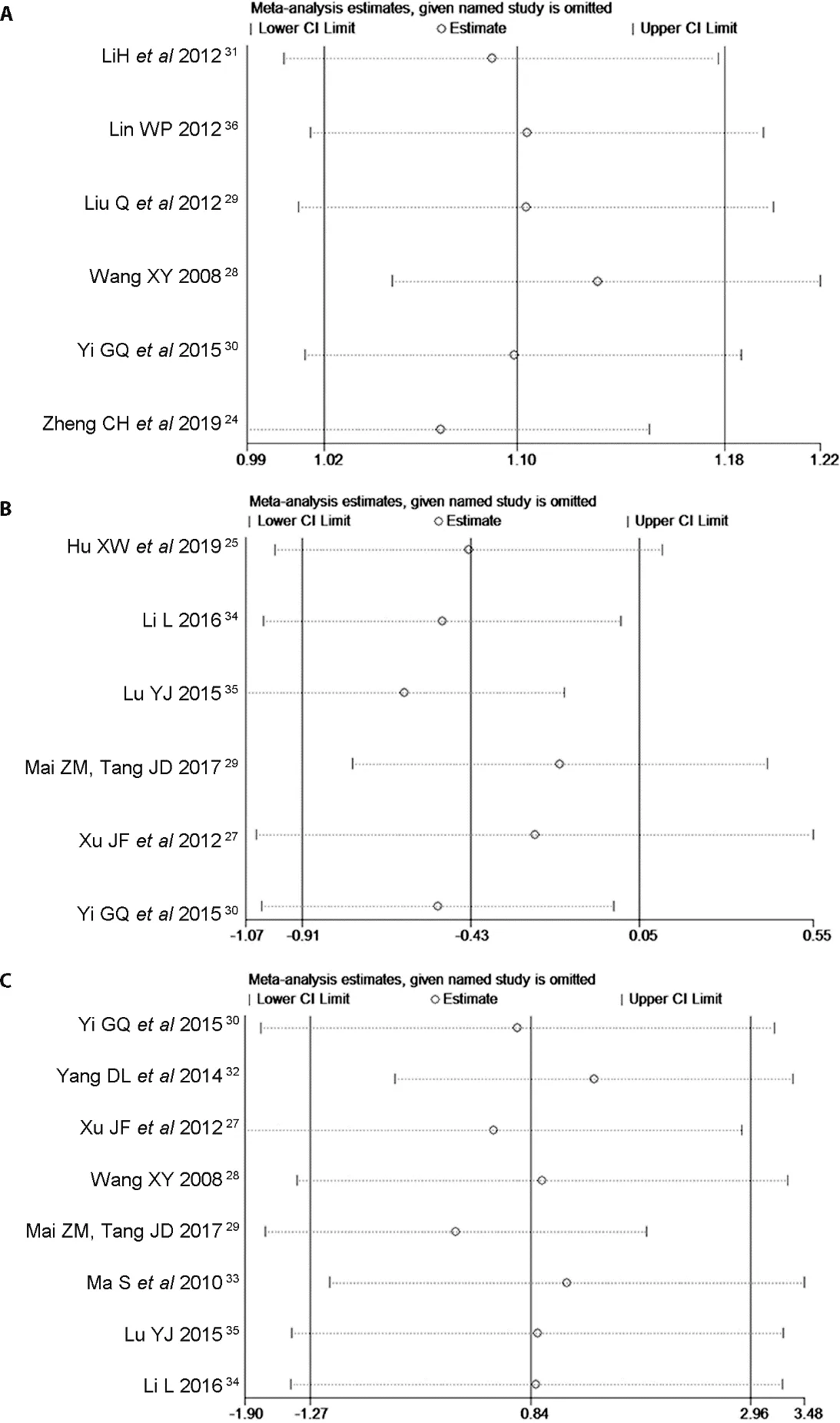
Figure 4 Sensitivity analysis
3.11.Publication bias
Based on the response rate,we used a funnel plot to have qualitative analysis of publication bias.Based on the visual assessment,no significant evidence of publication bias was identified.This result may be related to the fact that fewer than 10 studies were included.The publication bias of studies is depicted in Appendix S2.
3.12.Quality of evidence
The evidence level of the results from the 19 studies that measured moxibustion was determined to be very low to low (Table 2).The level of evidence was downgraded because of the study design and risk of bias (the generation of random sequence,blindness,and allocation concealment are not clear),inconsistency of results(unreasonable heterogeneity),and the imprecision of the included studies (the number of the participants was too small).
4.DISCUSSION
4.1.Principal findings
This systematic review and Meta-analysis evaluated the response rate,pain management,and functional improvement of moxibustion in the treatment of LDH.We evaluated 19 RCTs involving 1888 patients.All studies utilized moxibustion alone in experimental groups.Meanwhile,the control group intervention included acupuncture,drug therapy,conventional therapy,acupuncture plus drug therapy,acupuncture plus TDP irradiation,and fixed-point rotation reduction.In addition,four trials did not disclose the details of random sequence generation,and another fifteen RCTs used random tables for randomization.Notably,only one trial was reported to have used allocation concealment and blinding of outcome assessment.Two studies mentioned dropouts without reporting detail information.
Based on the abovementioned observations,the findings of our review indicated that moxibustion may have equivalent effects for treating LDH on all of the four outcome measurements when compared with acupuncture.When moxibustion was compared with drug therapy,the ODI score indicated that moxibustion had more favorable effects,but the VAS score suggested no difference between these two therapies.Moreover,when moxibustion was compared with acupuncture combined with TDP irradiation,no significant difference was identified in the response rate.However,compared with conventional therapy,moxibustion had significantly favorable effects with regard to its VAS score and ODI score.When compared with fixed-point rotation reduction,moxibustion had considerably favorable effects in improving the VAS score,JOA score,and ODI score.Notably,only one study was found in some subgroup analyses,which may lead to inaccurate results.Sensitivity analyses showed that our results were robust.The funnel plot suggested no significant publication bias.Therefore,these findings require an expanded sample.In addition,the evidence level of these results was determined to be very low to low,which indicated that these positive results should be interpreted with caution.Moreover,the safety of moxibustion for LDH treatment remains unclear because of the lack of studies that provide sufficient details of the adverse events.

Meta-analysis evaluating the efficacy of moxibustion on LDH treatment concluded that moxibustion is more effective than acupuncture,41which is different from our results.We found that they included trials that used acupuncture and moxibustion as the experimental group.Moreover,they did not adopt subgroup analysis based on different interventions in control groups,which may increase the unreliability of the results.Furthermore,our review used four outcome measurements to evaluate the effect of moxibustion for LDH,which was not available in previous systematic reviews.
Subgroup analysis was conducted to settle the heterogeneity among studies.Nevertheless,the results of subgroup analysis failed to explain the heterogeneity,which may be due to the experimental design.During literature screening,moxibustion therapies varied in implementation forms (such as moxibustion methods,treatment duration,selection of moxibustion points,and sessions) and lack of standards,which may limit the application and spread of moxibustion in clinical practice.Previous studies that focused on moxibustion for LDH,low back pian,and rheumatoid arthritis treatment also had high heterogeneity.10,42,43Based on these findings,further studies must focus on factors affecting the therapeutic effect of moxibustion.
In our review,the results demonstrated that all the outcomes had no statistical difference between moxibustion and acupuncture.Therefore,the therapeutic effect of moxibustion on LDH may be comparable to acupuncture.As an important means of TCM,acupuncture has been widely recognized.Recently,a meta-analysis has identified the superior effect of acupuncture on LDH,2which indicated that acupuncture had a more favorable effect in treating LDH than lumbar traction,ibuprofen,diclofenac sodium,meloxicam,dexamethasone plus mannitol and mecobalamin,mannitol plus dexamethasone,loxoprofen,etc.Therefore,as a non-invasive treatment,moxibustion may be more acceptable to patients than acupuncture.
With the increasingly more extensive application of moxibustion,its mechanism has gained increasing attention.Notably,modern medicine believes that moxibustion can prevent and treat diseases with the function of anti-inflammation and immune improvement.44Based on a study of a LDH rat model,45moxibustion can effectively decrease the neurological function score of model rats and improve lower limb function while reducing the level of serum inflammatory cytokine IL-1β.It can also inhibit the infiltration of inflammatory cells in nerve root tissues and surrounding tissues and reduce the damage of chemical inflammation to nerve roots.One hypothesis emphasizes the fact that moxibustion is a result of warm stimulation,which stimulates and regulates the function of the nervous system by stimulating skin receptors.46In particular,heat produced by moxibustion activates local specific receptors,heat-sensitive immune cells,and heat shock proteins to initiate the warming and dredging function and produce various total effects.The warming stimulation signals and subsequent effects through nerve and body fluid pathways induce the effect of further specific target organs and body systems.47However,no systematic moxibustion treatment mechanism is identified at present,and more research on moxibustion treatment mechanisms is needed in the future.
4.2.Strengths and limitations
Our study was the first Meta-analysis that evaluated the efficacy of moxibustion alone for LDH treatment.We reviewed related literature in English,Chinese,Japanese,and Korean databases.In addition,four outcome measurements were used to evaluate the efficacy of moxibustion alone for LDH treatment,which was not available in previous systematic reviews.The GRADE profile was also adopted to test the quality of result evidence,which made the results more reliable.However,this study also had several important limitations that need to be discussed.First,the majority of the included studies were of low quality.Notably,most of the included studies failed to provide the details of sequence generation,allocation concealment,blinding methods,adverse events,and withdrawals or dropouts.In addition,considering that few trials required a long-term followup,analyzing the long-term effects of this treatment was impossible.Therefore,this study only presented the short-term curative effect of moxibustion on LDH treatment.
Based on the limitations,this study indicated that welldesigned,multi-center randomized controlled trials were warranted to establish the efficacy of moxibustion on LDH treatment.Moreover,further research should be conducted to determine the long-term effects of moxibustion.
In conclusion,based on the existing evidence,moxibustion may not be suitable for treating LDH alone,but it may be applied as an adjuvant treatment.Furthermore,well-designed RCTs with high-quality and large samples are necessary to evaluate the efficacy and safety of moxibustion alone for LDH treatment.
5.ACKNOWLEDGEMENTS
Thank you to all the participants and clinical researchers involved in the publications cited in this review.Thank you to all the peer reviewers who contributed to the continuous improvement of this article.The authors are also immensely grateful for the financial support provided by the National Natural Science Foundation of China and the Nanjing University of Chinese Medicine.
杂志排行
Journal of Traditional Chinese Medicine的其它文章
- Effects of the Huangkui capsule (黄葵胶囊) on chronic kidney disease: a systematic review and Meta-analysis
- Efficacy of acupuncture therapy for post-stroke fatigue: a systematic review and Meta-analysis
- Efficacy of luteolin on the human gastric cancer cell line MKN45 and underlying mechanism
- Tilianin extracted from Xiangqinglan (Herba Dracocephali Moldovicae) inhibits apoptosis induced by mitochondrial pathway and endoplasmic reticulum stress in H9c2 cells after oxygenglucose deprivation/reoxygenation
- Comparing the effects of three decoctions for coronavirus disease 2019 on severe acute respiratory syndrome coronavirus 2-related tolllike receptors-mediated inflammations
- Astragaloside IV ameliorates insulin induced insulin resistance in HepG2 cells through reactive oxygen species mediated c-Jun Nterminal kinase pathway
