Nutritional supplementation on wound healing in diabetic foot: What is known and what is new?
2022-11-24AndreaDaPortoCesareMirandaGabrieleBrosoloGiorgioZanetteAndreaMichelliRobertoDaRos
Andrea Da Porto,Cesare Miranda,Gabriele Brosolo,Giorgio Zanette,Andrea Michelli,Roberto Da Ros
Andrea Da Porto,Gabriele Brosolo,Department on Internal Medicine,University of Udine,Udine 33100,Italy
Cesare Miranda,Giorgio Zanette,Department of Internal Medicine,Clinic of Endocrinology and Metabolism Diseases Azienda Sanitaria Friuli Occidentale,Pordenone 33170,Italy
Andrea Michelli,Roberto Da Ros,Department of Internal Medicine,SC Diabete e Centro Trattamento Piede Diabetico,Monfalcone 34074,Gorizia,Italy
Abstract Non-healing diabetic foot ulcers (DFU) are the most notable and striking complications of diabetes mellitus.More than 25% of nonhealing DFU can ultimately lead to amputation of the lower extremity within 6-18 mo after the first manifestation of the wound.Although wound healing is complex,nutritional status is crucial in soft tissue repair.Malnutrition is highly prevalent and overlooked in patients with diabetes and chronic wounds.Moreover,to date,we do not have clear recommendations or evidence about the use of nutritional supplements for improving wound healing in patients with DFU.In this article the authors briefly analyzed the current evidence on the use of nutritional supplements of proteins or amino acids,fatty acids,probiotics,vitamins,and trace elements in the wound healing process in patients with DFU.
Key Words:Malnutrition;Supplements;Diabetic foot;Diabetes;Wound healing;Nutritional therapy
INTRODUCTION
The Global Burden of Disease study[1],estimated that 131.0 million (1.77%) people worldwide had diabetes-related lower-extremity complications (DRLECs) in 2016,equal to 34% of the diabetes population.Among these patients almost 105.6 million had neuropathy;18.6 million had foot ulcers,and 6.8 million undergone to amputation.Moreover,it is known than 84% of lower extremity amputations are preceded by a foot ulcer[2],however ulcer prevention is still an overlooked opportunity[3].
In patients with diabetes known risk factors for developing ulcers are peripheral arterial disease,peripheral neuropathy,repeated trauma,history of previous ulcers,and/or amputation.Male subjects,patients with a longer duration of the disease and a low socioeconomic level have the highest risk[4-7].
Non-healing diabetic foot ulcers (DFU) are the one of the most relevant and dangerous complications of diabetes mellitus[2].A diabetic foot ulcer is defined as nonhealing in the case of a wound area reduction of less than 50% after 4 weeks of standard care[8].More than a quarter of non-healing DFU may in the end leads to lower extremity amputation within 6-18 mo after the wound’s outset[9].
Although wound healing is regulated by complex mechanisms,the outcome of the process is the complete repair of the damaged tissue.It is known that infection,wound depth,size,and duration negatively impact healing process and are therefore associated with poor outcomes and possible amputation[10].
Nutritional status is crucial in wound healing.The presence of a wound has a negative impact on nutritional status due to the metabolic cost of repairing damaged tissue,in addition to nutrient loss through wound inflammatory exudate.Malnutrition is highly prevalent in patients with chronic diabetic foot wounds[11],and specific micronutrient deficiencies are common and associated with impaired wound healing and increase the risk of amputation in people with DFU[12,13].Malnutrition is known to impair the inflammatory phase of the healing process,reducing fibroblast proliferation and collagen synthesis,increasing the risk of developing infections,decreasing T lymphocyte function,phagocytic activity,complement,and antibody levels[14].Moreover,nutritional defect of polyunsaturated fatty acids (PUFAs) and consequent reduced synthesis of the essential fatty acid-derived resolvins,(crucial regulators of inflammatory phase of wound healing) are particularly deleterious in people with DFU where diabetes itself is associated with an overall decreased production of proresolving lipid mediators[15].
Therefore,nutritional interventions can improve DFU healing.Current Australian guidelines recommend the evaluation of nutritional status when progress towards DFU closure is not made[16] and the use of oral nutritional supplements (ONS) when an oral diet is not sufficient to meet nutritional requirements.However,to date,we do not have clear recommendations or evidence on the use of nutritional supplements to improve wound healing in patients with DFU.
This article aimed to evaluate current evidence regarding the use of Nutritional (Proteins,Aminoacids,Omega 3,probiotics,vitamins,and Trace Elements) supplementation on wound healing in patients with DFU (Table 1).
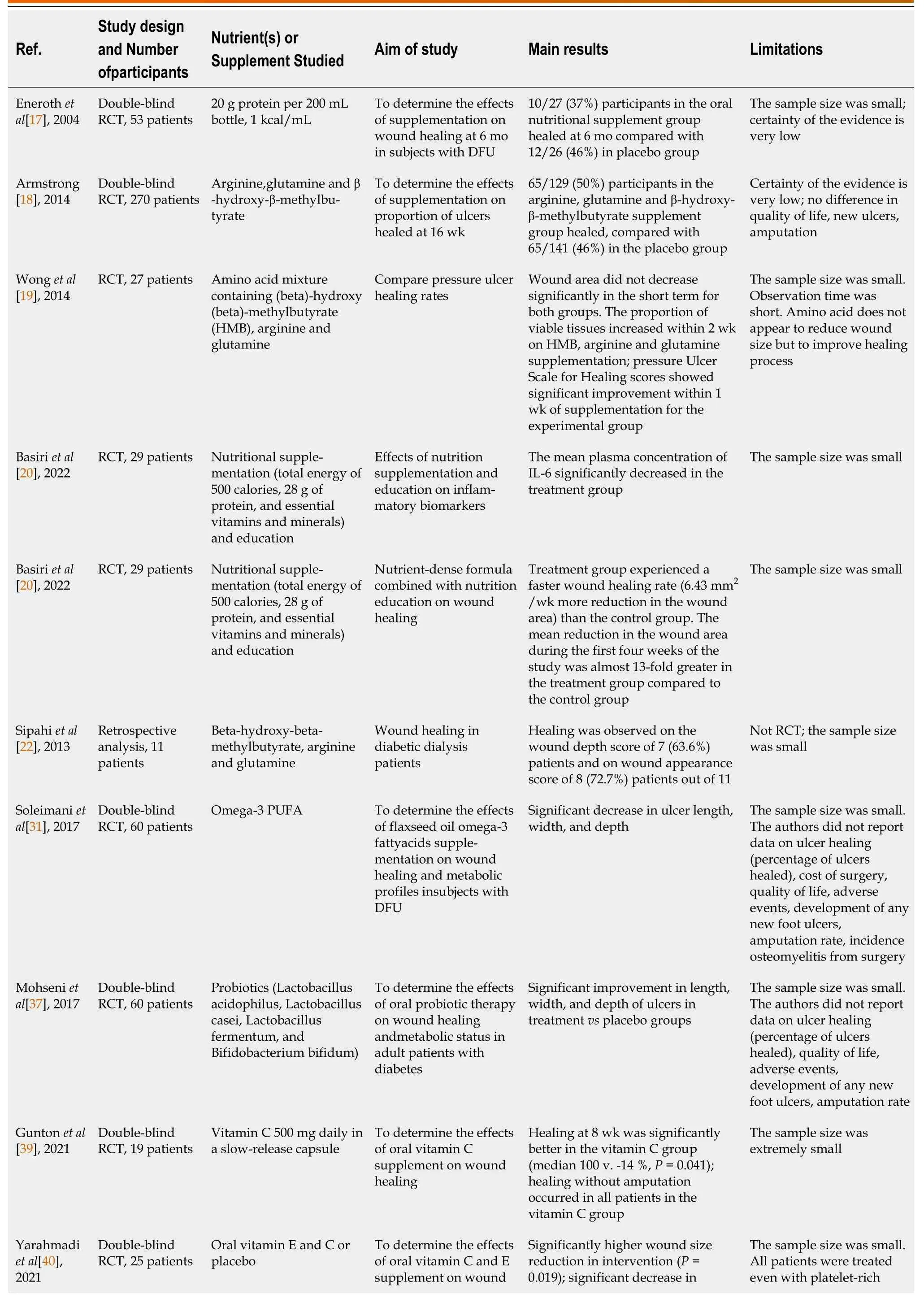
Table 1 Strengths and Limitations of the main randomised controlled trial that evaluated the effects of specific nutritional supplement on wound healing in patients with diabetic foot ulcers
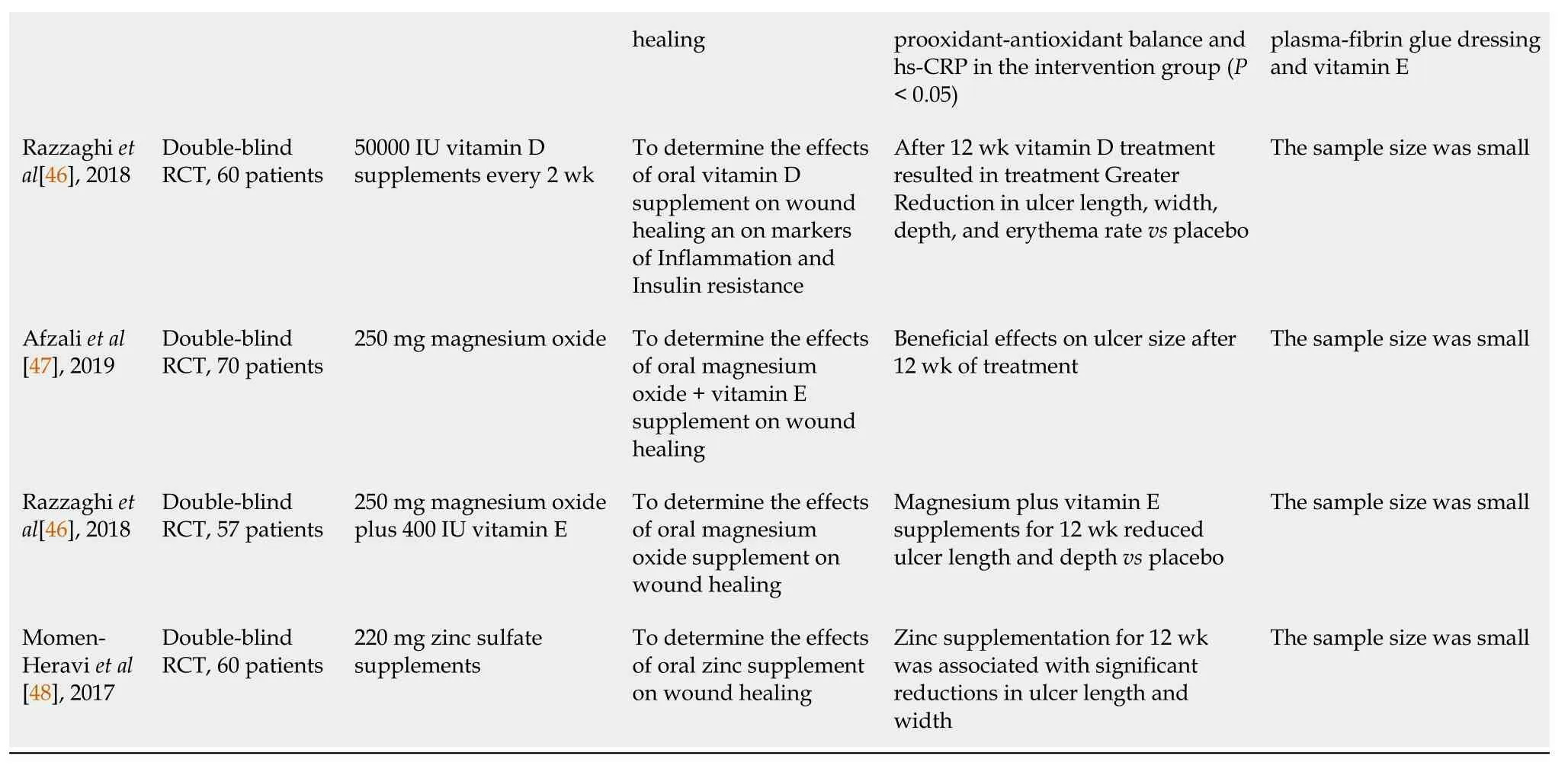
RCT: Randomised controlled trial;DFU: Diabetic foot ulcers;PUFA: Polyunsaturated fatty acids.
PROTEIN AND AMINO ACIDS
Proteins and amino acids are the most frequent nutritional supplementation used to improve the healing of diabetic foot wounds,starting from the evidence of the positive effects of these compounds in wound healing.We identified four randomised controlled trial (RCT) studies that supplemented with protein or amino acid mixture in patients with diabetic foot.Eneroth 2004[17] supplemented 27 malnourished patients with diabetic foot ulcers with 20 g protein per 200 mL bottle and compared them with a placebo (26 patients).It is unknown whether there is a difference in the proportion of ulcers healed at the end of the study period,or an absolute change in individual parameters of ulcer dimensions,or ulcer area,over time,for those treated,or not treated with an ONS.Secondary outcomes too,amputation and adverse events (death),didn’t demonstrate a difference.Armstronget al[18],an RCT with 270 patients,experimented with supplementation with arginine,glutamine,and b-hydroxy-bmethyl butyrate on foot ulcer healing in people with diabetes.No differences were found between groups in wound closure or time to wound healing after 16 wk.Subgroup analysis shows that the addition of arginine,glutamine,and b-hydroxy-b-methyl butyrate in addition to the standard of care can improve the healing of diabetic foot ulcers in patients with the risk of limb hypoperfusion and/orhypoalbuminemia.Wonget al[19],use a mixture of amino acid containing (beta)-hydroxy (beta)-methyl butyrate (HMB),arginine,and glutamine in diabetic patients with pressure ulcers without obtaining wound area reduction,but demonstrates a better proportion of viable tissues on HMB,arginine,and glutamine supplementation group.Recently Basiriet al[20],evaluated the effects on wound healing of a treatment regime based on nutritional education in combination with a nutritional supplement (total of 500 kilocalories,28 g of protein,and essential vitamins and minerals) in a group of patients with DFU getting a faster wound healing rate in treated group.The mean reduction in wound area during the first four weeks was almost 13 times greater in patients treated with nutritional supplement compared to the control group.Moreover,the same authors demonstrated in another publication that nutritional intervention could have favorable effects on controlling inflammation in patients with DFU[21].Finally,we included in this analysis a retrospective study,from Sipahiet al[22] for interesting results in diabetic dialysis patients supplemented with aminoacid (beta-hydroxy-beta-methyl butyrate,arginine,and glutamine) obtaining healing in most of the patients (63.6%).Dialysis always represents a challenge in the healing of the diabetic foot.
In summary,the results of the current studies did not give a clear effect of proteins and amino acids in the healing of diabetic foot wounds,but there is some evidence of efficacy with improvement in the healing process.The nutritional status of the participants was not an inclusion/exclusion criterion in the studies included in the review.As such,the supplement was generally given randomly irrespective of the presence or absence of malnutrition at inclusion),thus,the baseline nutritional status of the participants is independently correlated with the severity of infection,increased risk of poor outcome,poor prognosis after vascular interventions and it even predicts amputation.Furthermore,it is unclear what the minimum duration is required to achieve a measurable impact on the wound once the serum level of a particular nutrient has improved beyond the deficient range.
POLYUNSATURATED OMEGA-3 FATTY ACIDS
Long-chain Omega-3 PUFA and their bioactive metabolites (resolvins,marine,protectin) have long been considered as powerful negative modulators of acute inflammation and/or inducers of its resolution[23],while the role they play in the wound healing process is still largely unknown.Interest is growing in the understanding of the specific effects of PUFA derived metabolites on the cellular and molecular mechanisms involved in the modulation of inflammatory process[24].The most bioactive PUFAs are eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) that can be obtained directly from many dietary sources as fish and algae,or indirectly through the endogenous metabolic conversion of their precursor,as linolenic acid contained in high concentrations in vegetables and nuts.
Data on the effects of omega-3 fatty acids from flaxseed oil on wound healing in human studies are scarce.Additionally,the studies[25-27] that have evaluated the effects of fish oil supplements (rich in omega-3) on wound healing in patients without diabetes have produced mixed results.
Regarding the consequence of omega-3 fatty acids on inflammatory factors,a meta-analysis showed that supplementation with marine-based omega-3 induce a significative reduction of C-reactive protein,IL-6,and tumor necrosis factor α[28].
McDanielet al[26,27,29] showed that supplementing omega-3 for 4 wk in a healthy subjects resulted in increased production of pro-inflammatory cytokines,including IL-1ß at wound sites representing a potential therapeutic option for people with chronic wounds[26-29].
As recommended in the Expert consensus and guidance of the American limb preservation society on nutrition interventions in adults with diabetic foot ulcers,mono and PUFAs,including EPA,DHA,and arachidonic acid should be considered because they contribute to membrane fluidity,membrane and intracellular signals,and modulation of apoptotic pathways[30] (ALPS Nutrition Interventions in Adults with Diabetic Foot Ulcers Expert Consensus and Guidance).
In a double-blind RCT,Soleimaniet al[31] evaluated the effects of daily omega-3 fatty acids from flax seeds for 12 wk in 60 subjects with grade 3 DFU according to “Wagner-Meggitt's criteria”.Participants were assigned to receive 1 g twice daily of omega-3 PUFA or a placebo for 12 wk.A significant reduction in ulcer width,length,and depth and an increase in insulin sensitivity and total antioxidant capacity was observed in the intervention compared to the control group.As reported by Mooreet al[32] the study of Soleimaniet al[31] had several limitations.The sample size was small.The authors did not report percentage of ulcers healed,cost of surgery,quality of life,amputation rate,and incidence of osteomyelitis from surgery.
PROBIOTICS
An emerging treatment line for wound healing is the use of probiotics,defined by the International Scientific Association of Probiotics and Prebiotics as “live microorganisms which when administered in adequate amounts confer a health benefit on the host”[33].
The most common probiotics used as supplements include members of the Lactobacillus spp,Bifidobacterium genera[34],strains from other bacterial species (Propionibacterium acidilactici,Lactococcus lactis,Leuconostoc mesenteroides,Bacillus subtilis,Streptococcus thermophilus) and yeasts (Saccharomycesboulardii)[35].
Perioperative supplementation of probiotics demonstrated accelerated skin healing in diabetic rats,probably due to a reduction of the inflammatory response,increased neovascularization,and increased type I collagen deposition.Supplementation with probiotics also prevents weight loss and improves glycemic control in animal models[36].
In a double-blind RCT,the effects of daily probiotics supplementation for 12 wk were examined in 60 patients with DFU with cellulitis on wound healing[37].Participants were randomly assigned to receive a probiotic capsule or placebo daily for 12 wk.
The study founds improvement in length,width,and depth of the ulcers in patients treated with probiotic supplement compared with placebo.Additionally,compared to placebo,a significant decrease in HbA1c (-0.6% ± 0.5%vs-0.2% ± 0.4%),total cholesterol and CRP levels was observed in treated patients.This study had several limitations: the sample size was small;the authors did not report data on ulcer healing,quality of life,adverse events,and amputation rate.
Studies on probiotic use are limited,for this reason more robust evidence are needed to examine the effects of probiotics on wound healing in patients with DFU.
VITAMINS AND TRACE ELEMENTS
Vitamin C
Vitamin C,also known as ascorbic acid,is a water-soluble vitamin that plays a pivotal role in many biological processes involved in wound healing,including collagen formation,regulation of the immune system,and maintenance of cartilage and bones.
The recommended dietary allowance for adults and older is 90 mg daily for men and 75 mg for women.Deficiency of Ascorbic Acid has been associated with increased severity of DFU in a prospective study of 131 patients with diabetic foot[12].Intriguing data derive from case series of people with diabetes and poorly healing lower limb ulcers in whom there was prompt ulcer healing with vitamin C replacement[38].
Recent evidence from some small randomized controlled trials has raised the idea of a possible benefit of vitamin C supplements on wound healing in DFU.An Australian placebo-controlled randomized trial founds that active treatment with Vitamin C 500 mg daily in a slow-release capsule for 8 wk results in a better percentage reduction in ulcer volume in 7 patients with DFU[39].
With similar findings Yarahmadiet al[40] demonstrate that supplements of vitamin E (200IU/2 d) and C (250IU/2 d) for eight weeks significantly increase wound healing in patients with non-healing DFU by enhancing the wound healing process and reducing oxidative stress in 13 patients treated within platelet-rich plasma-fibrin glue dressing plus[40].
Therefore,although seminal evidence is promising and of interest for future research,more convincing and robust evidence on the role of ascorbic acid in wound healing is required.
Vitamin D
Vitamin D is a fat-soluble vitamin that has long been known to help the body absorb certain calcium and phosphorus;both are essential for the building of bone.Circulating levels of 25 (OHD) are low in patients with DFU[12] or patients with severe peripheral artery disease[41].Furthermore,vitamin D insufficiency has been associated with impaired inflammatory responses,oxidative stress,and wound healing.A meta-analysis of observational studies reports that severe vitamin D deficiency is associated with foot ulceration[42] in people with diabetes.However,evidence of the benefits of vitamin D supplementation in DFU is still lacking.To date,we have only a few RCTs (most of them for the same study group) that evaluated the effects of Vitamin D supplementation on wound healing in DFU.A doubleblind,placebo-controlled,randomized clinical trial,conducted among 60 patients with grade 3 DFU according to “Wagner-Meggitt” criteria,showed that after 12 wk of intervention,compared to placebo,vitamin D supplementation resulted in a significant reduction in ulcer length,width,depth,and erythema rate[43].A very similar study with a comparable number of participants confirmed that a supplement of 60000 IU/weekly of cholecalciferol had a beneficial effect on wound healing when compared with a placebo[44].
More convincing and robust evidence is required on the role of vitamin D supplementation in wound healing.
Trace elements
The nutritional relevance of trace elements has grown rapidly due to a better understanding of their biological functions.They are involved with many enzymatic processes such as catalysis,oxidationreduction,and cellular transport.Therefore,trace elements have a pivotal role in the synthesis and structural stabilization of both proteins and nucleic acid needed for wound healing.In wound healing,the most important trace elements are zinc,copper,chromium,selenium,and magnesium,which are believed to be essential for the regeneration of physiological tissue in humans[45].However,only a few randomized controlled trials have tested the effect of trace element supplements on wound healing in DFU.
Effects of magnesium supplements on wound healing in people with diabetes were evaluated in 2 small randomized,double-blind,placebo-controlled trial.The first[46] was carried out among 70 subjects with grade 3 DFU according to the “Wagner-Meggitt” criteria and subjects treated with 250 mg of magnesium oxide had beneficial effects on ulcer size after 12 wk of treatment.In a similar study 57 patients with grade 3,DFU were randomized to take either 250 mg magnesium oxide plus 400 IU vitamin E (n=29) or a placebo per day (n=28) for 12 wk.Compared to placebo,taking magnesium plus vitamin E supplements reduced ulcer length and depth[47].
Zinc was tough to improve wound healing due to its effects on insulin resistance,inflammation,and oxidative stress.The effect of zinc supplements on wound healing in DFU was evaluated in a randomized,double-blind,placebo-controlled trial conducted among 60 patients with grade 3 diabetic foot ulcers[48].Participants were randomly assigned to take either 220 mg zinc sulfate supplements containing 50 mg elemental zinc or a placebo daily for 12 wk.Compared with the placebo,zinc supplementation was associated with significant reductions in ulcer length and width.
CONCLUSION
Current evidence supports that poor nutritional status is common and associated with the impaired healing process in patients with DFU.However,the number of good quality RCTs evaluating nutritional supplementation in DFU patients is limited with varying effects[30,49,50].Patients with diabetic foot ulcers require good multidisciplinary care to optimize wound healing,but often an important and overlooked aspect of this is their nutritional status.However,evidence for the impact of nutritional interventions on foot ulcer healing in people with diabetes remains uncertain,with studies showing no clear benefit or harm.For this reason,the IWGDF Guidelines on the use of interventions to improve healing of diabetic foot ulcers (2019) recommend not using interventions aimed at correcting the nutritional status of people with diabetic foot ulcers,to improve healing,preferring it as the best standard of care[10].Instead,according to the new Australian guidelines on wound healing interventions to improve wound healing,the nutritional status of the foot ulcer should be reviewed,and adequate daily nutritional needs should be met as part of the best standard of care "to ensure that this recommendation has not been misinterpreted[15].In conclusion more and well-designed studies are needed to better clarify the potential impact of nutritional supplementation on the healing of foot ulcers in people with diabetes.
PERSPECTIVES
Author’s suggestion for future research and design of proper RCT study: (1) Complete evaluation of nutritional status at the beginning,evidence,and agreement on malnutrition,and evidence if the population examined have a specific nutritional defect;(2) guarantee to all patient's real optimal standard therapy;(3) choose uniformity of wound conditions,don’t mix heterogeneous kinds of wounds.Consider that some conditions are time-limited,for example,choosing “infected wounds” we don’t define a homogeneous group,with this definition we could include neuropathic,ischemic,traumatic,or mixed lesions with very different characteristics;(4) adequate duration of supplementation and study too,since mean wound healing of diabetic foot is approximately 3 mo,it is not possible to evaluate healing in a shorter period;(5) evaluate evidence of supplementation with blood samples that demonstrate direct change in parameters;and (6) choose multiple parameters,other than healing,to evaluate the effects of supplementation: Rate of wound reduction,percentage of granulation tissue.
FOOTNOTES
Author contributions:Da Porto A and Miranda C came up with ideas and constructs;Da Porto A,Miranda C,and Da Ros R wrote the manuscript;Michelli A,Brosolo G,and Zanette G approved the main conceptual ideas and made corrections;all authors provided final edits and approved the manuscript.
Conflict-of-interest statement:The authors declare that they have no conflict of interest.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Italy
ORCID number:Andrea Da Porto 0000-0001-9995-0169.
S-Editor:Chen YL
L-Editor:A
P-Editor:Chen YL
杂志排行
World Journal of Diabetes的其它文章
- Risk factor analysis and clinical decision tree model construction for diabetic retinopathy in Western China
- Dietary Nε-(carboxymethyl) lysine affects cardiac glucose metabolism and myocardial remodeling in mice
- Role of defensins in diabetic wound healing
- Combination therapy of hydrogel and stem cells for diabetic wound healing
- Advances in neovascularization after diabetic ischemia
- Orthotic approach to prevention and management of diabetic foot: A narrative review
