Effectiveness of Zhuling decoction (猪苓汤) on diuretic resistance in patients with heart failure:a randomized,controlled trial
2022-07-20CHENYunhuFANLihuaZHANGTaoLIUXueqian
CHEN Yunhu,FAN Lihua,ZHANG Tao,LIU Xueqian
CHEN Yunhu,FAN Lihua,Department of Cardiovascular,Taicang Hospital affiliated with Nanjing University of Traditional Chinese Medicine,Suzhou 215400,China.
ZHANG Tao,Department of Cardiovascular,Changzhou Hospital affiliated with Nanjing University of Traditional Chinese Medicine,Changzhou 213003,China.
LIU Xueqian,Department of Cardiovascular,Taicang Hospital affiliated with Nanjing University of Traditional Chinese Medicine,Suzhou,215400,China.
Abstract OBJECTIVE:To test the effects of Zhuling decoction (猪苓汤) on patients with diuretic resistance in heart failure compared with a group of patients undergoing conventional treatment alone.METHODS:This research was a prospective,randomized,controlled study.From July 2018 to August 2020,96 diuretic resistance patients from the Cardiovascular Research Center of Taicang Hospital affiliated with Nanjing University of Traditional Chinese Medicine (Grade III Hospital of Traditional Chinese Medicine) were enrolled in the study.The subjects were randomly divided into an observation group (48 cases)and a control group (48 cases).Patients in both groups received conventional treatment.In addition,observation group patients received Traditional Chinese Medicine Zhuling decoction.The primary endpoint was the urine output mean difference between Day 1 and Day 7 after treatment.Secondary endpoints were the changes over time in the N-terminal pro-B type natriuretic peptide (NTproBNP),New York Heart Association (NYHA) functional classification,and Minnesota Living with Heart Failure Questionnaire (MLHFQ).The safety and tolerability of the drug were comprehensively evaluated based on adverse drug reactions,as well as laboratory-assisted tests for liver and kidney function and electrolytes.RESULTS:Significant improvements were demonstrated for urine output in the two groups at Day 7,with a 1325 vs 1045 mL difference in favor of the observation group(P=0.018).The observation group also had greater improvements in NT-proBNP and NYHA functional classification changes than the control group.At the 30th day of follow-up,a significant reduction in negative findings on the MLHFQ from baseline was observed in both groups,but the observation group demonstrated a significantly greater reduction than the control group (P<0.001).CONCLUSIONS:Zhuling decoction could be used in combination therapy for patients with diuretic resistance in heart failure in addition to standard treatment.
Keywords:heart failure;diuretic resistance;urine output;treatment outcome;Zhuling decoction;randomized controlled trial
1.INTRODUCTION
Heart failure (HF) is the end stage of many cardiovascular diseases.HF is common in China.A recent registered study from China showed that 1.3%(approximately 13.7 million) of the Chinese adult population aged 35 years or older had HF,1.4% of participants had ejection fractions below 50%,and 2.7%of patients were classified as having "moderate" or"severe" HF.1An estimated 6.5 million adults in the United States are affected by HF,and approximately 1 million people are hospitalized each year.2,3HF continues to be the leading discharge diagnosis in hospitalized patients 65 years of age or older.4The incidence and prevalence of HF increase significantly with age in both men and women.HF causes 300 000 deaths a year,with a 5-year mortality rate of up to 50%,and these figures are expected to worsen by 2030.5The total cost of care for HF exceeds $30 billion per year.
In recent years,great progress has been made in the drug treatment of HF,such as the emergence of some new drugs to improve heart function (such as sacubitril/valsartan,ivabradine,SGLT-2 inhibitors,recombinant human brain natriuretic peptide,levosimendan,and tolvaptan),which can effectively improve the symptoms of HF.However,diuretics represented by loop diuretics are still recognized as the cornerstone of treatment for HF.
However,diuretic resistance (DR) is inevitable in some HF patients,and the exact incidence is unknown.The literature reports that the incidence of DR in HF is approximately 30%.6,7It is estimated that 64.3 million people worldwide suffer from HF.8DR makes HF more complex and serious,consumes more medical resources,and is one of the important reasons why the treatment cost and mortality rate of HF have increased rapidly.There is no specific drug for DR,and the overall effect of its routine treatment is not always satisfactory.
Accurate assessment of DR is a basic clinical requirement.First,urine volume is the core index by which DR is measured,and the water and sodium retention of patients can be reflected by accurately recording the daily 24 h urine volume.Second,the New York Heart Association (NYHA) functional classification can be quickly determined by the severity of asthma.NYHA grade I is the mildest,and NYHA grade IV is the most severe.The Minnesota Living with Heart Failure Questionnaire (MLHFQ) is the most popular HF assessment tool,with 21 items,each with a score on a scale of 0 to 5,with lower scores indicating better quality of life.9N-terminal pro-B type natriuretic peptide (NT-proBNP) is a powerful diagnostic and prognostic biomarker for HF.10The higher the value is,the worse the heart function.These indicators can be obtained in a simple way and can be a powerful tool for rapid assessment of DR disease.
Many efforts have been made to find natural therapies that can effectively improve DR.Traditional Chinese Medicine (TCM) theories with rich experience in the treatment of HF posit that HF and DR belong to the category of diseases such as "edema" and "asthma".11,12Zhuling decoction (猪苓汤),a compound preparation composed of five Chinese herbs [Zhuling (Polyporus),Fuling (Poria),Zexie (Rhizoma Alismatis),Ejiao (Colla Corii Asini),Huashi (Talcum)],was created by Zhang Zhongjing,a famous doctor of the Han Dynasty.It has been used in the clinical treatment of edema for more than one thousand years.Previous research has proven that Zhuling decoction contains rich diuretic components and can significantly increase the amount of urine output in edema patients.However,no randomized controlled study has been reported in DR patients.It is not clear whether Zhuling decoction can improve DR safely and effectively.To this end,this study evaluated the efficacy and safety of TCM decoction (Zhuling decoction)combined with conventional treatment of DR by observing the changes in urine volume,NYHA functional classification,MLHFQ and NT-proBNP in patients with DR.
2.MATERIALS AND METHODS
In this study,a prospective,randomized,controlled study scheme was adopted,and the main objective was to evaluate whether the combination of Zhuling decoction with standardized western medicine in the treatment of DR is more effective than the singular use of western medicine.
2.1.Ethics approval
The study was reviewed and approved by the Research Ethics Committee of Taicang Hospital affiliated with Nanjing University of Traditional Chinese Medicine.All participants signed informed consent to participate in the study.All the physicians in the study had the title of attending physician or above and had passed the standardized training of cardiovascular specialists.
2.2.Study design
A total of 96 subjects from the Cardiovascular Research Center of Taicang Hospital affiliated with Nanjing University of Traditional Chinese Medicine were enrolled between July 2018 and August 2020.The selected subjects were randomly divided into a control group (CO group,48 cases) and an observation group(OB group,48 cases) according to a random number table.Subjects in both groups received the same conventional treatment.The observation group also received Zhuling decoction.
2.3.Inclusion/exclusion criteria
The inclusion criteria were as follows:ages from 35 to 90 years,no sex limitation,no TCM taken 1 month before inclusion,diagnosed with HF according to China's Chronic HF and Treatment Guidelines published in 2018,cardiac function classified as NYHA II-IV,limited (100 mg) furosemide given daily and urine volume less than 0.5-1 mL·kg-1·h-1.In addition,considering the particularity of decoction application,the selected subjects still needed to meet the criteria of Yin deficiency symptom pattern [designed by the expert group of this study,includes at least one primary (red tongue,little or no tongue coating,thready pulse) and one secondary (dry mouth and throat,fever of sensation,dry feces,oliguria)symptom].The exclusion criteria included allergic predisposition,severe mental illness,severe renal failure(serum creatinine > 3 mg/dL),and pregnant and lactating for women.
2.4.Intervention
All subjects received daily water restriction,sodium restriction,rest and other HF health care education.According to the guidelines for the treatment of HF,all subjects received general standard medication such as furosemide (the dose was limited to 100 mg daily for 1 week,and the route of administration was intravenous),aldosterone receptor antagonists,angiotensin-converting enzyme inhibitors/angiotensin receptor antagonists,beta-blockers,and medication that might lead to DR as much as possible.
The two groups of patients were treated with infusion combined with albumin,dopamine,hydrochlorothiazide and other therapeutic methods to relieve DR.In addition,the OB group patients received Zhuling decoction[Zhuling (Polyporus) 10 g,Fuling (Poria) 10 g,Zexie(Rhizoma Alismatis) 15 g,Ejiao (Colla Corii Asini) 10 g,Huashi (Talcum)10 g,Guizhi (Ramulus Cinnamomi)10 g,Chushizi (Broussonetia papyrifera) 10 g,Baizhu(Rhizoma Atractylodis Macrocephalae) 10 g,Yimucao(Herba Leonuri Japonici) 15 g,Huangqi (Radix Astragali Mongolici) 30 g].All TCM was supplied by Suzhou Tianling Chinese Medicines Co.,Ltd.,and met the quality standards of the hospital.Subjects in the OB group took the oral decoction half an hour after breakfast and dinner every day.The TCM was soaked in cold water for 30 min,boiled until the decoction was concentrated to approximately 100 mL,and then taken orally after cooling.The second time,an appropriate amount of cold water was added to the remainder of the first decoction,it was boiled and reduced to 100 mL and then taken orally after cooling.
2.5.Outcome measurements
All subjects were monitored as follows:24 h urine output from Days 1 to 7,NT-proBNP (Radiometer,Denmark),electrolytes,liver function,kidney function,NYHA cardiac function scale on Days 1 and 7,and MLHFQ on Days 1 and 30 (usually after discharge).Any adverse clinical events or adverse reactions were documented throughout the study.
The primary endpoint was the urine output mean difference between Days 1 and 7 after treatment.Secondary outcome measures were the changes over time in the NT-proBNP,NYHA cardiac function ratings and MLHFQ.The safety and tolerability of the drug were comprehensively evaluated based on adverse drug reactions,as well as laboratory-assisted tests for liver and kidney function and electrolytes.
2.6.Sample size estimation
According to the preliminary data of this study,after one week,the urine volume of the OB group could be increased by approximately 1200 mL,and the urine volume of the CO group could be increased by 800 mL,with a standard deviation (SD) of approximately 600 mL.An α (Type I error)=5% and β (Type II error)=0.2 were set,and the sample size was estimated as at least 36 cases per group by the formula.13
2.7.Statistical analysis
Statistical analysis was performed in SPSS 19.0 (IBM Corp.Released 2010.IBM SPSS Statistics for Windows,Version 19.0.Armonk,NY,USA,IBM Corp.)Continuous variables are expressed as the means and SDs or medians and interquartile ranges (IQRs).If the continuous data met the assumptions of a normal distribution and homogeneity of variances,thet-test was used for comparisons between groups.Otherwise,a nonparametric Wilcoxon rank sum test was performed.The nonparametric Wilcoxon rank sum test was used for the ordered data.APvalue < 0.05 was considered statistically significant.All tests were two-sided.
3.RESULTS
The overall research scheme is shown in Figure 1.A total of 96 subjects participated in this study at the center from July 2018 to August 2020.Subjects in the OB group took the decoction orally for at least 7 d and at most 30 d.Three patients in the OB group and 2 in the CO group dropped out before the postdischarge follow-up.The remaining subjects in both groups completed the entire study.The baseline characteristics of the two groups are shown in Table 1.Subjects in the two groups were consistent in terms of sex,age,etiology of HF,average course of HF,complications,liver and kidney function and other aspects before the test.
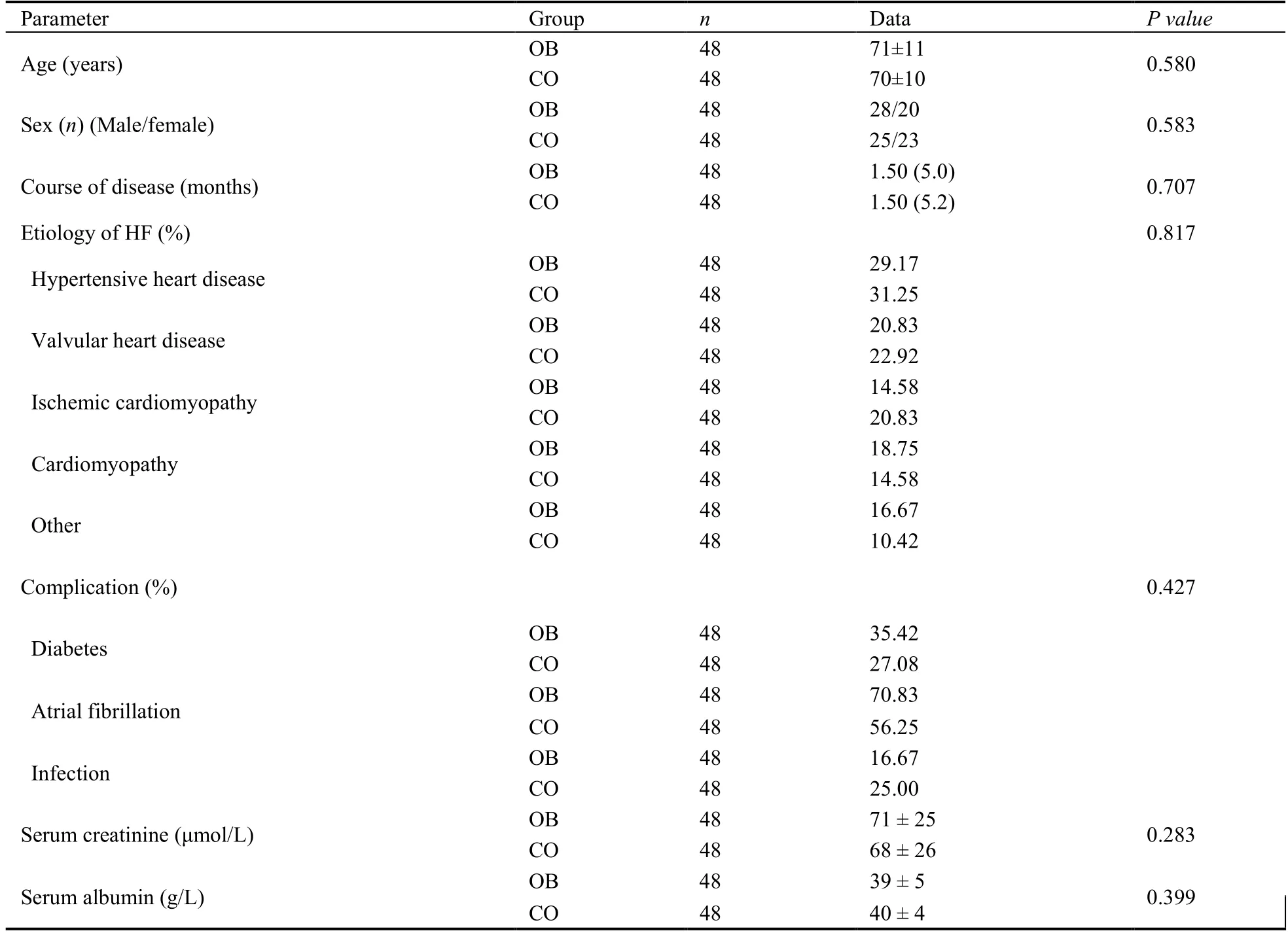
Table 1 Background data [means ± SDs or medians (IQRs)]
3.1.Urine output
The urine output showed no significant difference before treatment between the two groups (P=0.058) and increased significantly after treatment.The OB group started with 295 mL and ended with 1325 mL (difference of 1030 mL),while the CO group started with 315 mL and ended with 1045 mL (difference of 730 mL) [1325(IQR=883)vs1045 (IQR=415) (P=0.018)].There were 34/48 patients in the OB group and 28/48 patients in the CO group whose urine volume returned to more than 1000 mL per day over time (Figure 2).
3.2.NT-ProBNP and MLHFQ
There was no significant difference in NT-proBNP before treatment between the two groups (P=0.105).After 7 d of treatment,the NT-proBNP in both groups were significantly reduced compared with the baseline values.The reduction in NT-proBNP in the OB group was more significant [3780 (IQR=4145)vs830 (IQR=1910) (P< 0.001)].All subjects received MLHFQ scores on the 1st day after enrollment.The first score was obtained at the hospital,and the second (Day 30 after enrollment) was usually obtained by telephone after discharge.During the follow-up,3 patients in the OB group and 2 patients in the CO group dropped out.There was no significant difference between the OB group and the CO group on the first day after enrollment.At the second follow-up,scores in the OB group improved significantly and were better than those in the CO group(P< 0.001) (Figures 3-4).
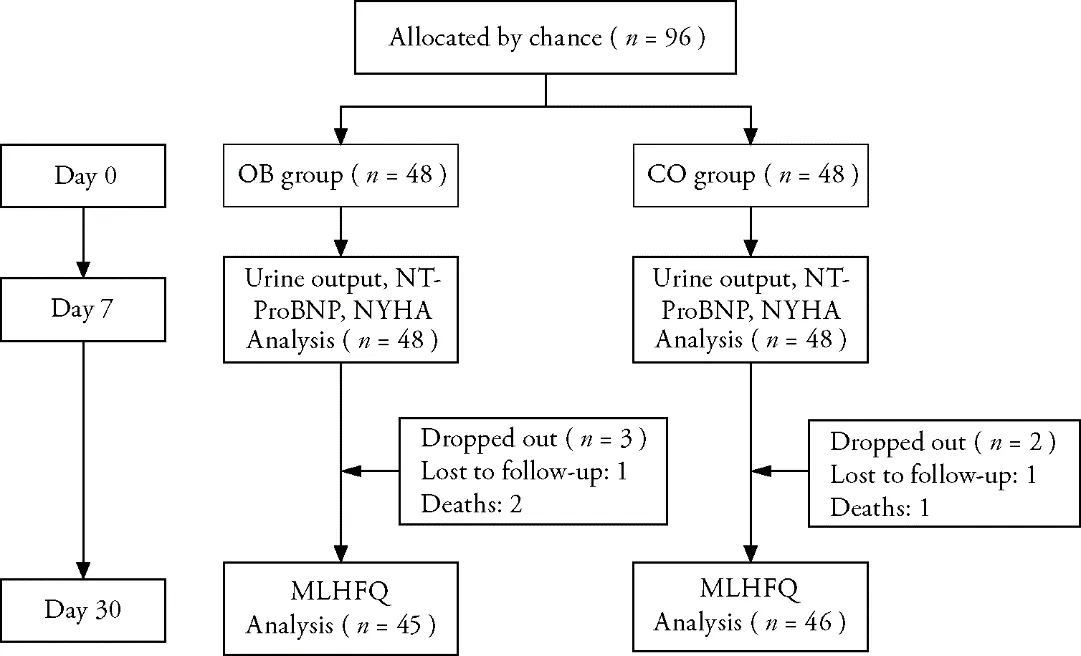
Figure 1 Study design
3.3.NYHA functional classification
There was no significant difference in the NYHA classification distribution between the two groups before the study (P=0.728).After 7 d of treatment,the proportion of NYHA II subjects in the two groups increased gradually,while the proportion of NYHA IIIIV subjects decreased gradually.NYHA improvement in the OB group was better than that in the CO group (P=0.029) (Figure 5).

Figure 2 Trend of urine volume according to group
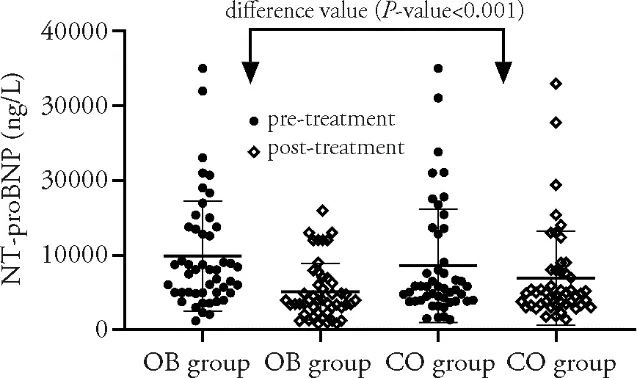
Figure 3 Changes in NT-proBNP before and after treatment in the 2 groups
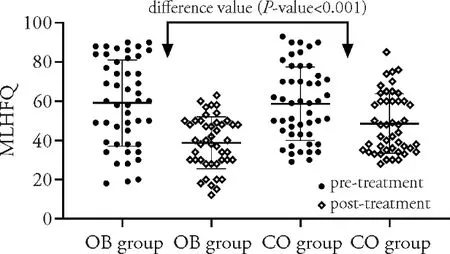
Figure 4 Changes in MLHFQ before and after treatment in the 2 groups

Figure 5 NYHA functional classification results
No important adverse effects were reported during this study.Two patients in the OB group developed mild diarrhea after taking the oral decoction.However,the diarrhea soon improved after treatment such as rehydration.
4.DISCUSSION
The term "diuretic resistance" remains inadequately defined.The most commonly cited definition is "failure to decongest despite adequate and increasing doses of diuretics".14Not all patients with HF develop DR.It has been reported that abnormal blood pressure,increased urea nitrogen,heart ischemia,diabetes and other factors may be predictive factors of DR.15-18
Water and sodium retention are important characteristics in patients with HF,so the removal of excess sodium and fluid is the primary therapeutic target.19,20It is usually necessary to test urinary sodium to reflect the therapeutic effect of diuretics and to determine the prognosis of HF.16,21,22However,these parameters are frequently inaccurate or not collected.In contrast,the urine output parameters of patients with HF are easier to obtainwithout additional economic costs.Changes in urine volume within a short period of time directly affect changes in cardiac function.Therefore,this study focused on observing the changes in urine volume of subjects in the two groups.In addition,NT-proBNP,NYHA functional classification and MLHFQ,effective indicators for evaluating heart function,have a close relationship with mortality and morbidity in HF patients.23After 7 d of observation,the improvement of urine volume and other secondary efficacy indicators in the OB group was significantly better than that in the CO group,suggesting that the application of TCM may improve DR.
The pathogenesis of DR is relatively complex and has not been fully studied.In general,there are multiple mechanisms involved in the occurrence of DR.Diuretic delay into the blood due to intestinal stasis and poor circulation function reduces the blood diuretic peak concentration.24The decrease in albumin absorption and synthesis in patients with HF leads to a significant decrease in the binding rate of diuretics to albumin,and a considerable number of diuretics that are not bound to albumin are lost to the intercellular space,resulting in the loss of diuretic effects.25The use of diuretics has a"postdiuretic sodium retention" effect and leads to a"braking phenomenon".This phenomenon may be due to the activation of the renin angiotensin aldosterone axis,pathological hypertrophy of renal distal convoluted tubular cells and increased sodium reabsorption,which counteract the effect of loop diuretics.26
DR usually needs to be improved by multiple means due to the lack of specific drugs.Many methods have been developed to improve DR over the past decade.These include continuous intravenous administration,increasing the dosage of diuretics,combining diuretics with albumin,blocking sodium uptake in different nephron segments in sequence,infusion of hypertonic saline,reducing intra-abdominal pressure and ultrafiltration.27
Chinese herbs have been used to treat HF effectively for thousands of years.Mainstream TCM scholars believe that HF is a symptom pattern of deficiency in origin and excess in superficiality and is mainly located in the heart,spleen and kidney.Deficiency is mainly responsible forQideficiency andYangdeficiency,while excess is mainly responsible for excessive fluid and blood stasis.In China,it is not uncommon to report the treatment of HF and improvement of DR with Chinese medicinal herbs,Chinese patent medicines or Chinese medicine injections.The most commonly used decoctions are Zhenwu decoction,Qili Qiangxin capsule,Danhong injection,etc.28,29However,the published research has some limitations.First,most clinical studies have small sample sizes or incomplete data.There are few doubleblind,controlled and randomized trials to evaluate the efficacy of TCM in the treatment of cardiovascular diseases.Furthermore,the important principle of TCM clinical treatment is symptom pattern identification,but in the real world,symptom pattern types of diseases are rarely set as inclusion criteria.
The definite role of TCM in the prevention and treatment of cardiovascular diseases is still unclear.Some scholars have explored the internal mechanism of TCM for HF treatment from the perspective of modern medicine.They believe that the application of TCM may change the antifibrotic role,inhibit inflammation,regulate angiogenesis and antioxidant performance,inhibit cell apoptosis and mitochondrial function and regulate energy metabolism and other functions.28
Zhuling decoction has a history of thousands of years in China,and it is still a popular decoction.According to TCM theory,Zhuling decoction has the functions of diuresis,Yinnourishing and heat clearing.It is mainly used for edema,oliguria,fever,thirst and other symptoms caused by water and heat mutually affecting Yin.We have found in clinical practice that a large number of DR patients have obvious dry mouth and decreased coating on the tongue after excessive use of diuretics.This indicates thatYindeficiency symptom pattern accounts for a high proportion of DR patients.In Zhuling decoction,Zhuling (Polyporus),which belongs to the kidney and bladder meridian,is the monarch drug and is specifically used for diuresis.Zhuling (Polyporus)is a kind of medicinal fungus.Its main chemical components are polysaccharides,steroids,amino acids,proteins,vitamins and trace elements.A number of published studies have shown that Zhuling (Polyporus)has significant renal protection and anti-inflammatory and diuretic effects.30-32Therefore,Zhuling (Polyporus)can be considered a natural diuretic.This may partly explain the mechanism of DR improvement.
The side effects of Chinese herbal medicines are usually considered by the outside world to be evaluated and understood.There may be an increased risk of drug interactions and side effects,especially when multiple herbal medicines are used.Although there are scattered reports of acute adverse events caused by herbal medicines,33,34it is safe and effective to apply reasonable doses of quality-controlled Chinese herbal medicines under the guidance of TCM theories.
This study also has some limitations.Different from the modern medical model,TCM emphasizes symptom pattern identification and treatment,which requires the subjects to meet the Yin deficiency symptom pattern standard on the basis of meeting the DR standard.This is the premise under which Zhuling decoction can improve DR.This increases the restrictions on the selection of subjects,making the sample size collected in this study in a relatively short period of time small.Moreover,the CO group did not receive placebo decoction intervention because there is currently no satisfactory TCM decoction placebo.
In conclusion,DR is a common problem in HF patients.On the basis of standardized treatment,the application of Zhuling decoction under the guidance of TCM theory is expected to be a new method to alleviate DR.However,this kind of traditional decoction has not been widely considered,and it needs to be further studied and explored in detail.
5.ACKNOWLEDGMENTS
We thank Professor Shoupeng Chen of Nanjing University of Traditional Chinese Medicine for providing information retrieval services in this experiment.
6.REFERENCES
1.Hao G,Wang X,Chen Z,et al.Prevalence of heart failure and left ventricular dysfunction in China:the China hypertension survey,2012-2015.Eur J Heart Fail 2019;21:1329-37.
2.Virani SS,Alonso A,Benjamin EJ,et al.Heart disease and stroke statistics-2020 update:a report from the American Heart Association.Circulation 2020;141:e139-596.
3.Murphy SP,Ibrahim NE,Januzzi JL,Jr.Heart failure with reduced ejection fraction:a review.JAMA 2020;324:488-504.
4.Benjamin EJ,Virani SS,Callaway CW,et al.Heart disease and stroke statistics-2018 update:a report from the American Heart Association.Circulation 2018;137:e67-492.
5.Heidenreich PA,Albert NM,Allen LA,et al.Forecasting the impact of heart failure in the United States:a policy statement from the American Heart Association.Circ Heart Fail 2013;6:606-19.
6.Gupta R,Testani J,Collins S.Diuretic resistance in heart failure.Curr Heart Fail Rep 2019;16:57-66.
7.Trullàs JC,Casado J,Morales-Rull JL,et al.Prevalence and outcome of diuretic resistance in heart failure.Intern Emerg Med 2019;14:529-37.
8.Global,regional,and national incidence,prevalence,and years lived with disability for 354 diseases and injuries for 195 countries and territories,1990-2017:a systematic analysis for the Global Burden of Disease Study 2017.Lancet 2018;392:1789-858.
9.Morgan K,McGee H,Shelley E.Quality of life assessment in heart failure interventions:a 10-year (1996-2005) review.Eur J Cardiovasc Prev Rehabil 2007;14:589-607.
10.Mueller C,McDonald K,de Boer RA,et al.Heart Failure Association of the European Society of Cardiology practical guidance on the use of natriuretic peptide concentrations.Eur J Heart Fail 2019;21:715-31.
11.Jiang M.The TCM stage-oriented treatment for chronic cardiac insufficiency.J Tradit Chin Med 2007;27:49-54.
12.Liang D,Zhang M.The thinking on TCM differential treatment of congestive heart failure.J Tradit Chin Med 2000;20:44-7.
13.Bacchetti P,Leung JM.Sample size calculations in clinical research.Anesthesiology 2002;97:1028-9;
14.ter Maaten JM,Valente MA,Damman K,Hillege HL,Navis G,Voors AA.Diuretic response in acute heart failurepathophysiology,evaluation,and therapy.Nat Rev Cardiol 2015;12:184-92.
15.Palazzuoli A,Testani JM,Ruocco G,Pellegrini M,Ronco C,Nuti R.Different diuretic dose and response in acute decompensated heart failure:Clinical characteristics and prognostic significance.Int J Cardiol 2016;224:213-9.
16.Testani JM,Brisco MA,Turner JM,et al.Loop diuretic efficiency:a metric of diuretic responsiveness with prognostic importance in acute decompensated heart failure.Circ Heart Fail 2014;7:261-70.
17.ter Maaten JM,Dunning AM,Valente MA,et al.Diuretic response in acute heart failure-an analysis from ASCEND-HF.Am Heart J 2015;170:313-21.
18.Voors AA,Davison BA,Teerlink JR,et al.Diuretic response in patients with acute decompensated heart failure:characteristics and clinical outcome--an analysis from RELAX-AHF.Eur J Heart Fail 2014;16:1230-40.
19.Gheorghiade M,Follath F,Ponikowski P,et al.Assessing and grading congestion in acute heart failure:a scientific statement from the acute heart failure committee of the heart failure association of the European Society of Cardiology and endorsed by the European Society of Intensive Care Medicine.Eur J Heart Fail 2010;12:423-33.
20.Gheorghiade M,Vaduganathan M,Fonarow GC,Bonow RO.Rehospitalization for heart failure:problems and perspectives.J Am Coll Cardiol 2013;61:391-403.
21.Verbrugge FH,Nijst P,Dupont M,Penders J,Tang WH,Mullens W.Urinary composition during decongestive treatment in heart failure with reduced ejection fraction.Circ Heart Fail 2014;7:766-72.
22.Binanay C,Califf RM,Hasselblad V,et al.Evaluation study of congestive heart failure and pulmonary artery catheterization effectiveness:the ESCAPE trial.JAMA 2005;294:1625-33.
23.Goetze JP,Bruneau BG,Ramos HR,Ogawa T,de Bold MK,de Bold AJ.Cardiac natriuretic peptides.Nat Rev Cardiol 2020;17:698-717.
24.Vazir A,Cowie MR.Decongestion:diuretics and other therapies for hospitalized heart failure.Indian Heart J 2016;68:S61-8.
25.Cox ZL,Lenihan DJ.Loop diuretic resistance in heart failure:resistance etiology-based strategies to restoring diuretic efficacy.J Card Fail 2014;20:611-22.
26.Iqbal J,Javaid MM.Diuretic resistance and its management.Br J Hosp Med (Lond) 2014;75:C103-7.
27.Jardim SI,Ramos Dos Santos L,Araújo I,et al.A 2018 overview of diuretic resistance in heart failure.Rev Port Cardiol (Engl Ed)2018;37:935-45.
28.Wang Y,Wang Q,Li C,et al.A review of Chinese herbal medicine for the treatment of chronic heart failure.Curr Pharm Des 2017;23:5115-24.
29.Lin S,Shi Q,Yang F,Wang X,Mao J.Traditional Chinese Medicine injections for heart failure:a protocol for systematic review and network Meta-analysis of randomised controlled trials.BMJ open 2020;10:e037331.
30.Huang JW,Lai CJ,Yuan Y,Zhang M,Zhou JH,Huang LQ.Correlative analysis advance of chemical constituents of Polyporus umbellatus and Armillaria mellea.Zhong Guo Zhong Yao Za Zhi 2017;42:2905-14.
31.Yuan D,Mori J,Komatsu KI,Makino T,Kano Y.An antialdosteronic diuretic component (drain dampness) in Polyporus sclerotium.Biol Pharm Bull 2004;27:867-70.
32.Li H,Yan Z,Xiong Q,et al.Renoprotective effect and mechanism of polysaccharide from Polyporus umbellatus sclerotia on renal fibrosis.Carbohydr Polym 2019;212:1-10.
33.Zakeri MA,Mohammadi V,Bazmandegan G,Zakeri M.Description of ventricular arrhythmia after taking herbal medicines in middle-aged couples.Case Rep Cardiol 2020;6061958.
34.Zakeri MA,Bagheripour MH,Iriti M,Dehghan M.Portal vein thrombosis after the consumption of date seed powder:a case study.Case Rep Med 2021;6668722.
猜你喜欢
杂志排行
Journal of Traditional Chinese Medicine的其它文章
- Efficacy of meridian massage for motor function after a stroke:a systematic review and Meta-analysis
- Antiviral Activity of Medicinal Plants against Human Coronavirus:a systematic scoping review of in vitro and in vivo experimentations
- Fuzheng Kang' ai decoction (扶正抗癌方) inhibits cell proliferation,migration and invasion by modulating mir-21-5p/human phosphatase and tensin homology deleted on chromosome ten in lung cancer cells
- Correlation between slow transit constipation and spleen Qi deficiency,and gut microbiota:a pilot study
- Efficacy of Kushen decoction (苦参汤) on high-fat-diet-induced hyperlipidemia in rats
- Hyperpolarization-activated cyclic nucleotide-gated 2 contributes to electroacupuncture analgesia on lumbar disc herniation-induced radicular pain through activation of microglia in spinal dorsal horn
