A Clinical Study:Therapeutic Effects of Repetitive Transcranial Magnetic Stimulation and Cognitive Behavioral Therapy on Cognitive Impairment in Alcohol-Dependent Patients
2022-07-15XiaoHeFANWeiBianYANGChengJiWUDanSUNChangHaoYINHongXuanWANGYingPENGYanZhongGUANXiaoFengZHU
Xiao-He FAN,Wei-Bian YANG,Cheng-Ji WU,Dan SUN,Chang-Hao YIN,Hong-Xuan WANG,Ying PENG,Yan-Zhong GUAN,Xiao-Feng ZHU
(1.Mudanjiang Medical University,Mudanjiang 157011,China;2.Hongqi Hospital Affiliated to Mudanjiang Medical University,Mudanjiang 157011,China;3.The First Affiliated Hospital of Jiamusi University,Jiamusi 154007,China;4.Sun Yat-sen Memorial Hospital of Sun Yat-sen University,Guangzhou 510120,China;5.Collaborative Innovation Center of Development and Application of Northern Medical Herbs,Mudanjiang 157011,China)
Abstract: Objective To observe the effects of repetitive transcranial magnetic stimulation (rTMS) and cognitive behavioral therapy (CBT) on cognitive function in alcohol-dependent patients.Methods Data from 285 alcohol-dependent patients were collected from Mudanjiang Medical University and Sun Yat-sen Memorial Hospital at Sun Yat-sen University between 2019 and 2021.The patients were divided into groups depending on alcohol abstinence and non-abstinence.There were 43 patients in the alcohol consumption (AC) group.The patients in the abstinence group were randomly assigned to treatment regimens with different combinations of rTMS and CBT using the Elton system.There were 49 patients in the TB+C0 group,36 in the TB+C1 group,44 in the TL+C0 group,36 in the TL+C1 group,37 in the TR+C0 group,and 40 in the TR+C1 group.Cognitive function was assessed by using the Montreal Cognitive Assessment Scale (MoCA).Results The proportion of patients with cognitive impairment in the AC group at 24 weeks was higher than that at baseline (P<0.05),whereas the proportion of cognitive impairment in the other groups did not differ significantly over time.The percentage of patients with cognitive impairment at 24 weeks was 52.3% in the TL+C0 group and 47.2% in the TL+C1 group,which was significantly lower than that in the AC group (P<0.05).MoCA scores at different time points in the AC group were significantly higher than those in the TB+C0,TL+C0,TL+C1,TR+C0,and TR+C1 groups,respectively.MoCA scores were significantly higher at 12 weeks compared with the baseline in the TB+C0,TL+C0,TL+C1,TR+C0,and TR+C1 groups (P<0.05),and similar changes were observed at 24 weeks.The MoCA scores in the TL+C1 and TL+C0 groups were higher than those in the TR+C0 group at 12 weeks after the intervention (P<0.05).Furthermore,MoCA scores in each of the TB+C1,TL+C1,TL+C0,TR+C1,and TR+C0 groups were higher than those in the AC group at 24 weeks (P<0.05).Conclusion Alcohol consumption impairs cognitive function,as evidenced by a significantly higher proportion of cognitive impairment after 24 weeks of non-abstinence.Most of the tested treatment regimens improved cognitive function.High frequency rTMS of the left dorsolateral prefrontal cortex (DLPFC) was associated with a greater improvement in cognitive function than that of the right DLPFC in alcohol-dependent patients at 12 weeks of abstinence.There does not appear to be a therapeutic advantage of CBT for cognitive impairment in alcohol-dependent patients.Screening for impaired cognitive function should be seriously considered for patients who engage in heavy drinking,and measures should be taken to reduce the risk of dementia induced by alcohol dependence.
Key words: Alcohol dependence; cognitive function; repetitive transcranial magnetic stimulation; cognitive behavioral therapy
In 2020,the World Health Organization reported that alcohol use disorder (AUD) had been among the top 20 diseases affecting the global burden of disease score for nearly 30 years[1].AUD includes both alcohol dependence and alcohol abuse.Alcohol dependence (AD),commonly known as "alcohol addiction",is a chronic and complex brain disease.It is traditionally divided into psychological dependence and physical dependence,and is associated with many psychological and physical problems.Chronic heavy drinking can induce structural and functional damage in the brain,and alcohol-induced cognitive impairment has been documented in neuropsychological and neuroimaging studies[2].Repetitive transcranial magnetic stimulation (rTMS) of the dorsolateral prefrontal cortex (DLPFC) and cognitive behavioral therapy (CBT) have become increasingly available in recent years,and these treatment options have produced valuable short-term effects[3-4].Current treatments for alcohol dependence focus on the promotion of behavioral and psychosocial adaptation.However,few treatment programs for alcohol dependence have addressed neurocognitive impairment.In this study,we measured the therapeutic effects of both high-frequency rTMS and CBT on cognitive impairment in alcohol-dependent patients.
1 Design and Methods
1.1 Study designWe examined patients with alcohol dependence in the community,inpatient settings,and outpatient settings at Mudanjiang Medical University and Sun Yat-sen Memorial Hospital of Sun Yat-sen University from 2019 to 2021.The inclusion criteria were as follows:(1)compliance with the Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV) "alcohol dependence" diagnostic criteria;(2) age 18~65 years.The exclusion criteria were as follows:(1)presence of acute alcohol withdrawal;(2)history of severe neurological or other psychiatric disorders,brain injury,or severe physical illness;(3)current or recent use of psychotropic drugs;(4) presence of contraindications to transcranial magnetic stimulation (TMS).The elimination criteria were as follows:(1)serious adverse reactions during the study;(2)poor compliance with the treatment protocol;(3)resuming of drinking during the study.
This randomized controlled trial included 354 alcohol-dependent patients,including 69 patients who dropped out of the study or missed assessments.Patients in the control group continued consuming alcohol throughout the study (AC).Patients in the intervention group abstained from alcohol and were randomly assigned the following treatment regimens according to the Elton system:sham TMS combined with sham CBT (TB+C0),sham TMS combined with CBT (TB+C1),rTMS of the right DLPFC combined with sham CBT (TR+C0),rTMS of the right DLPFC combined with CBT (TR+C1),rTMS of the left DLPFC combined with sham CBT (TL+C0),and rTMS of the left DLPFC combined with CBT (TL+C1).There were 43 patients in the AC group,49 in the TB+C0 group,36 in the TB+C1 group,44 in the TL+C0 group,36 in the TL+C1 group,37 in the TR+C0 group,and 40 in the TR+C1 group.
The study was approved by the Hospital Medical Ethics Committee and all subjects and their families were informed and signed an informed consent form prior to the trial.
1.2 Study methodWe delivered rTMS using the Magneuro100(Nanjing Weiss Medical Technology Company Co.,Nanjing,China).The rTMS target was either the left or right DLPFC,and the coil was placed tangential to the scalp.The stimulation intensity was set at 110% of the movement threshold,and the stimulation frequency was 10 Hz.The stimulation pulse was 5 seconds long,and the inter-pulse-interval was 20 seconds.rTMS was delivered for 10 days(5 days per week)with 30 stimulation pulses per day.CBT was delivered over eight sessions(approximately 30 minutes in length)with different themes for individual cognitive-behavioral therapy.WeChat (A social networking software) was used as the vehicle for online psychotherapy.
Cognitive function was analyzed at baseline (just before treatment),8 weeks,12 weeks,and 24 weeks using the Montreal Cognitive Assessment(MoCA) scale.The total score was out of 30.Patients with a score of 26 or above were considered to have normal cognitive function,and those with a score of less than 26 were considered to have cognitive impairment.The patients were classified into three categories according to weekly alcohol consumption:light drinking(<3 standard drinks/week),moderate drinking(male:3~14 standard drinks/week; female:3~7 standard drinks/week),and heavy drinking(male:>14 standard drinks/week;female:>7 standard drinks/week)[5].
1.3 Statistical methodsWe used SPSS 25.0 statistical software for our analysis.We used the Kruskal-Wallis rank-sum test or chi-square test for comparisons between groups according to whether the data were ordered or unordered categorical information.Data with multiple groups were analyzed using Cochran's Q test.MoCA scores were described by M(QR)if the data did not have a normal distribution.Between-groups comparisons were performed using the Kruskal-Wallis rank-sum test,and within-group comparisons were analyzed using the Wilcoxon rank-sum test or the Friedman test.Two-way analyses were corrected using the Bonferroni method.Values ofP<0.05 were considered statistically significant.
2 Results
2.1 General demographic dataA chi-square test of the gender,age group,drinking amount,and drinking history of the alcohol-dependent patients in the seven groups showed no statistically significant between-group differences for any of these indicators respectively(P>0.05).The patients were mainly male,middle-aged,and heavy drinkers(Table 1).

Table 1 Demographic information and alcohol-related data for the seven patient groups
2.2 The proportions of patients with cognitive impairment according to groupThe proportion of alcohol-dependent patients with cognitive impairment at study enrollment ranged from 52.3% to 77.6%.The proportions of patients with impaired cognition were analyzed at baseline,8 weeks,12 weeks,and 24 weeks.We found that the proportion of patients with cognitive impairment in the AC group was 67.4% at baseline and 83.7% at 24 weeks(P<0.05).In the treatment groups,the proportion of patients with cognitive impairment after treatment(at 24 weeks)did not significantly differ from that at baseline(P>0.05).However,in most of the intervention groups,we observed a decreasing trend in cognitive impairment from baseline to 12 weeks,but then an increasing trend from 12 weeks to 24 weeks.
When we compared the groups at different time points,the percentage of cognitive impairment was 52.3% in the TL+C0 group and 47.2% in the TL+C1 group at 24 weeks,which was significantly lower(P<0.05)than that in the AC group at 24 weeks(Table 2).The time-based differences in the proportions of cognitive impairment in the other intervention groups were not statistically significant(P>0.05).Our data indicated that the proportion of cognitive impairment in the group with rTMS of the left DLPFC at 24 weeks was lower than that in the AC group,regardless of whether the intervention group received CBT.
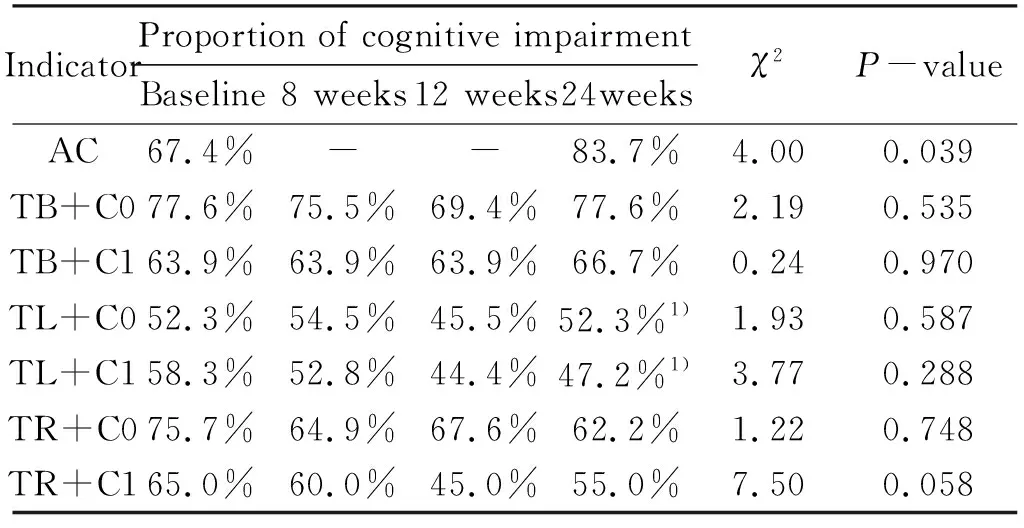
Table 2 Proportions of patients with cognitive impairment according to group
2.3 MoCA scores in the intervention groups at different time pointsUnlike those in the AC group,the MoCA scores in the six intervention groups tended to increase over time after the onset of abstinence.The Wilcoxon rank sum test(Table 3)revealed a significant difference in MoCA scores between the baseline and 24 weeks in the AC group(Z=2.426,P<0.05),indicating that alcohol consumption reduced MoCA scores.
Friedman's test(Table 3)showed that MoCA scores at baseline in the TB+C1 group did not differ from those at 8 weeks,12 weeks,or 24 weeks,implying no significant effects of post-abstinence CBT on cognitive function.Furthermore,MoCA scores in the TB+C1 group at different time points were significantly higher than those in the TB+C0,TL+C0,TL+C1,TR+C0,and TR+C1 groups,respectively.
Post-hoc pairwise comparisons,corrected for significance levels via the Bonferroni method,revealed a significant increase in MoCA scores at 12 weeks compared with that at baseline in the TB+C0,TL+C0,TL+C1,TR+C0,and TR+C1 groups,respectively(P<0.05)(Table 3 and Table 4).Similarly,MoCA scores at 24 weeks were significantly higher than those at baseline in the TB+C0,TL+C0,TL+C1,TR+C0,and TR+C1 groups,respectively.We found significant differences in MoCA scores at 8 versus 24 weeks in the TL+C1 and TR+C0 groups,respectively(P<0.05),and the MoCA scores at 24 weeks were higher than those at 8 weeks.
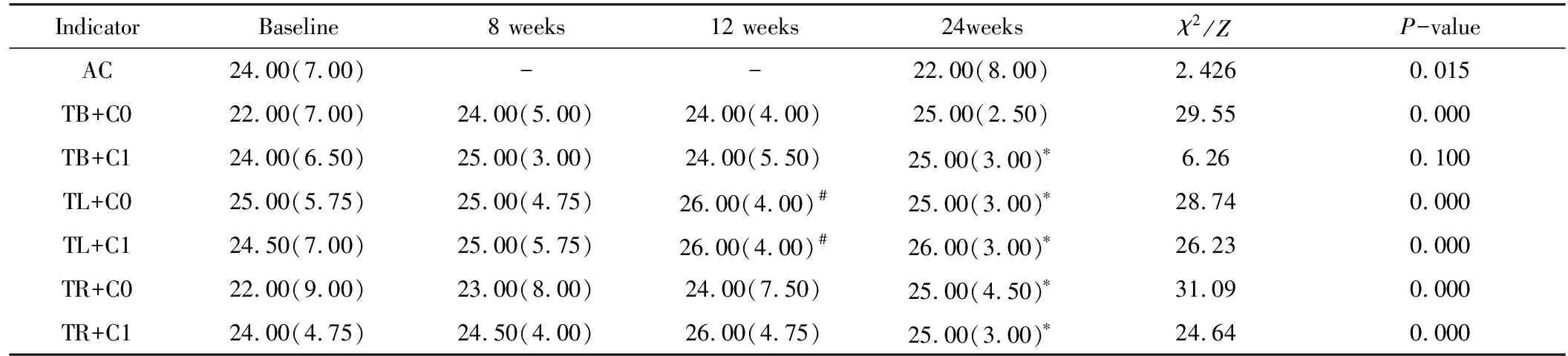
Table 3 MoCA scores in alcohol-dependent patients according to intervention group and assessment time

Table 4 Post-hoc analyses of MoCA scores at different time points
The Kruskal-Wallis rank sum test revealed no significant differences in MoCA scores between the groups at baseline and at 8 weeks(P>0.05).However,we found a statistically significant difference in MoCA scores between the groups at 12 and 24 weeks,respectively(P<0.05).Post-hoc pairwise comparisons using the Bonferroni method and corrected for significance levels revealed higher MoCA scores in the TL+C1 and TL+C0 groups(Table 3)compared with the TR+C0 group 12 weeks after treatment(P<0.05).Furthermore,MoCA scores in each of the TB+C1,TL+C1,TL+C0,TR+C1,and TR+ C0 groups were higher than those in the AC group at 24 weeks(P<0.05).
3 Discussion
The 2016 Global Burden of Disease Study suggested that the safest amount of alcohol intake for good health was no intake.Furthermore,alcohol was considered to be a high risk factor for more than 200 health problems.Accordingly,the viewpoint that moderate alcohol consumption is beneficial for health was revised[6].In the current study,patients in the persistent drinking group exhibited evidence of further impaired cognition after 24 weeks of drinking,whereas abstaining from alcohol intake improved cognitive function.Alcohol might impair prefrontal cortical function,which is associated with judgment,reasoning,abstraction,language,calculation,and other cognitive abilities.If this brain region is damaged,significant mental impairment may occur.A previous study showed that cognitive function improved after 3 months of abstinence from drinking,although other impairments might persist[7].Consistent with this report,we found that most patients in the current study showed improvements in cognitive function after 3 and 6 months of abstinence from alcohol.There is significant recovery in cognitive function during the first 3 months after alcohol cessation,with a trend of relapse thereafter.This suggests that treating of alcohol dependent patients should focus on cognitive function 3 months after stopping drinking and intervene accordingly AUD is involved in early-onset dementia,and 50%~80% of patients with AUD exhibit mild or severe neurocognitive impairment.Accordingly,AUD is a major controllable risk factor for dementia[8-9].In parallel with other studies,the proportion of patients with cognitive impairment in this study ranged from 52.3% to 77.6% at baseline,most of whom were middle-aged and young adults who engaged in heavy drinking.Thus,early screening for cognitive impairment and limiting alcohol consumption in heavy drinkers should be priorities for reducing the risk of dementia.
To date,few studies have examined interventions to improve cognitive function in alcohol-dependent patients,and no efficient interventions are currently recommended for clinical use[10].The application of CBT in the treatment of alcohol dependence focuses on addressing psychosocial factors.CBT could be used to train patients not only to maintain abstinence but also to resist relapse,which could be valuable in preventing relapse and improving patient compliance[3].The results of the current study imply that CBT did not ameliorate cognitive impairment in alcohol-dependent patients.It is possible that impaired cognition in these patients reduced the efficiency of CBT because the therapeutic effect of this treatment is limited by the perceptual ability and executive function of the patients,amongst other factors.
High-frequency(HF)rTMS in the treatment of alcohol dependence may reduce ethanol cravings.A meta-analysis showed that HF rTMS stimulation in the left DLPFC was more efficient than the stimulation of other areas in reducing substance-dependent craving[11].For instance,although the International Federation of Clinical Neurophysiology did not recommend HF rTMS for treatment of alcohol dependence in its 2019 guidelines,HF rTMS of the left DLPFC was recommended for treating nicotine addiction withdrawal[12].Here,we found that HF rTMS of the left DLPFC led to a greater improvement in cognitive function than that of the right DLPFC in alcohol-dependent patients after 12 weeks of abstinence.Furthermore,our data showed that HF rTMS of the left DLPFC significantly attenuated the exacerbation of cognitive impairment at 24 weeks.rTMS of the DLPFC could increase the plasticity of network connectivity in some brain regions,which would be beneficial for cognitive recovery[13].However,another group found that 21 days of HF rTMS in alcohol-dependent patients improved cognitive function only after the application of 5-HT reuptake inhibitors[14].One possible explanation for this discrepancy is differences in rTMS parameters.
In summary,alcohol consumption impairs cognitive function,and the proportion of patients with cognitive impairment increased after 24 weeks of non-abstinence.Most treatment regimens in this study improved cognitive function in alcohol-dependent patients after alcohol cessation,although we observed an increase in cognitive impairment in some patients after a 3-month relief period.HF rTMS of the left DLPFC led to stronger improvements in cognitive function than that of the right DLPFC in alcohol-dependent patients after 12 weeks of abstinence.Our data indicate no therapeutic advantage of CBT for cognitive impairment in alcohol-dependent patients.Screening for impaired cognitive function in patients who engage in heavy drinking should be seriously considered to reduce the risk of dementia induced by AUD.
