不同入路全髋关节置换术治疗GardenⅢ、Ⅳ型股骨颈骨折效果及对肌肉组织损伤、骨代谢的影响
2022-04-02崔涛唐绪军
崔涛 唐绪军




【摘要】 目的:探讨不同入路全髋关节置换术治疗GardenⅢ、Ⅳ型股骨颈骨折效果及对肌肉组织损伤、骨代谢的影响。方法:选择济宁市第二人民医院2018年1月-2020年6月收治的股骨颈骨折行全髋关节置换术(THA)的患者93例,按照手术方式不同将患者分为DAA组45例与PLA组48例,DAA组给予直接前入路THA,PLA组采用后外侧入路THA。比较两组手术相关指标、疼痛及髋关节功能评分、并发症发生情况、肌肉组织损伤及骨代谢指标。结果:与PLA组比较,DAA组手术时间更长、术中出血量更少、切口长度更短,差异均有统计学意义(P<0.05),两组髋臼前倾角及髋臼外展角比较,差异均无统计学意义(P>0.05)。两组术前视觉模拟评分(VAS)及Harris评分比较,差异均无统计学意义(P>0.05);两组术后VAS评分及Harris评分均優于术前,差异均有统计学意义(P<0.05);术后1、3 d,DAA组VAS评分均低于PLA组(P<0.05);术后2周及3个月,DAA组Harris评分均高于PLA组(P<0.05),术后6个月两组Harris评分比较,差异无统计学意义(P>0.05)。两组并发症发生率比较,差异无统计学意义(P>0.05)。两组术前肌酸激酶(CK)、C反应蛋白(CRP)比较,差异均无统计学意义(P>0.05),术后1、3 d,两组CK、CRP较术前均明显升高,且PLA组均高于DAA组,差异均有统计学意义(P<0.05)。两组术前Ⅰ型前胶原氨基前肽(PINP)、Ⅰ型前胶原羧基端肽(PICP)及抗酒石酸酸性磷酸酶-5b(TRACP-5b)比较,差异均无统计学意义(P>0.05),术后3个月两组PINP、PICP、TRACP-5b均优于术前,且DAA组均优于PLA组,差异均有统计学意义(P<0.05)。结论:直接前入路全髋关节置换术治疗GardenⅢ、Ⅳ型股骨颈骨折有利于髋关节功能早期恢复,减少患者疼痛及肌肉组织损伤,改善患者骨代谢。
【关键词】 全髋关节置换术 股骨颈骨折 直接前入路 骨代谢
Effect of Different Approaches of Total Hip Arthroplasty in the Treatment of Garden Ⅲ and Ⅳ Femoral Neck Fracture and the Effect on Muscle Tissue Injury and Bone Metabolism/CUI Tao, TANG Xujun. //Medical Innovation of China, 2022, 19(07): 0-072
[Abstract] Objective: To investigate the effect of different approaches of total hip arthroplasty in the treatment of Garden type Ⅲ and Ⅳ femoral neck fractures and its influence on muscle tissue injury and bone metabolism. Method: A total of 93 patients with femoral neck fracture who underwent total hip arthroplasty (THA) in Jining NO.2 People’s Hospital from January 2018 to June 2020 were selected and divided into DAA group (n=45) and PLA group (n=48) according to different operation methods. DAA group was given direct anterior approach THA and PLA group was given posterolateral approach THA. The operation related indexes, pain and hip function scores, complications, muscle tissue injury and bone metabolism indexes were compared between the two groups. Result: Compared with PLA group, the operation time was longer, the amount of intraoperative bleeding was less and the length of incision was shorter in DAA group, the differences were statistically significant (P<0.05), but there were no significant differences in acetabular anteversion and abduction angle between the two groups (P>0.05). There were no significant differences in preoperative VAS score and Harris score between the two groups (P>0.05); the postoperative visual analogue scale (VAS) scores and Harris scores of the two groups were better than those before operation, and the differences were statistically significant (P<0.05); the VAS scores of DAA group were lower than those of PLA group 1 and 3 days after operation (P<0.05); the Harris scores of DAA group were higher than those of PLA group at 2 weeks and 3 months after operation (P<0.05), there was no significant difference in Harris score between the two groups at 6 months after operation (P>0.05). There was no significant difference in the incidence of complications between the two groups (P>0.05). There were no significant differences in creatine kinase (CK) and C-reactive protein (CRP) between the two groups before operation (P>0.05), but CK and CRP were significantly increased in the two groups 1 and 3 days after operation, and those of PLA group were higher than those of DAA group (P<0.05). There were no significant differences in N-terminal peptide of type Ⅰ procollagen (PINP), carboxyl terminal propeptide of type Ⅰ procollagen (PICP) and tartrate resistant acid phosphatase-5b (TRACP-5b)between the two groups before operation (P>0.05), 3 months after operation, PINP, PICP and TRACP-5b in the two groups were better than those before operation, and those of DAA group were better than those of PLA group, the differences were statistically significant (P<0.05). Conclusion: Direct anterior total hip arthroplasty in the treatment of Garden type Ⅲ and Ⅳ femoral neck fractures is conducive to early recovery of hip function, reduce pain and muscle tissue damage, and improve bone metabolism.
[Key words] Total hip arthroplasty Femoral neck fracture Direct anterior approach Bone metabolism
First-author’s address: Rencheng District People’s Hospital of Jining, Shandong Province, Jining 272100, China
doi:10.3969/j.issn.1674-4985.2022.07.016
随着年龄的增长,股骨颈骨折的发生率呈指数增长[1],尤其在老年人群中,由于骨质疏松性骨密度变化、髋周肌群退化、反应能力退化等原因,在受到撞击等外力作用时易发生骨折[2]。全髋关节置换术(THA)是治疗股骨颈骨折的重要方法,可显著地缓解疼痛和改善功能[3]。关于THA的最佳入路至今仍存在争议,理想的术式应是术中损伤小、术后功能恢复好且并发症少,后外侧入路(PLA)是最常用的入路,但其主要缺点为易发生后脱位[4];直接前入路(DAA)为肌间隙及神经间隙入路,术中医源性肌肉损伤更少,术后恢复更快更好[5-6],但有研究指出其术后并发症发生率更高[7-8]。因此,本研究就DAA与PLA对GardenⅢ、Ⅳ型股骨颈骨折患者手术相关指标、疼痛及髋关节功能评分、术后并发症、肌肉组织损伤、骨代谢的影响展开研究,报道如下。
1 资料与方法
1.1 一般資料 选择济宁市第二人民医院2018年1月-2020年6月收治的股骨颈骨折行全髋关节置换术的患者93例。纳入标准:(1)确诊为股骨颈骨折且为GardenⅢ、Ⅳ型;(2)初次行全髋关节置换术;(3)临床资料完整;(4)配合本研究。排除标准:(1)精神疾病史或沟通障碍;(2)体重指数(BMI)>30 kg/m;(3)合并其他影响本研究的疾病,如神经肌肉病变、既往髋部手术史、感染等。按照手术方式不同将患者分为DAA组45例与PLA组48例。本研究经医学伦理委员会批准同意。患者对本研究知情同意。
1.2 方法 两组均采用全身麻醉。DAA组给予直接前入路THA,患者取仰卧位,髋关节后伸,于髂前上棘外侧及远端2~3 cm处向腓骨头方向作一8~10 cm切口,暴露并“T”形切开髋关节囊,利用拉钩充分显露关节囊内股骨颈并截断,取出股骨头,置入Hoffman拉钩暴露并去除髋臼周围增生赘骨,后植入髋臼假体,患肢内收外旋位置于健肢下方,完全暴露股骨近端,植入股骨假体并安装合适的股骨头,复位髋关节,检查下肢长度、活动度及人工髋关节稳定性后缝合关闭伤口。PLA组采用后外侧入路THA,患者取侧卧位,以大转子顶点为中心在其后外侧做一长10~12 cm的弧形切口,依次切开皮下组织、浅筋膜、深筋膜、臀大肌及外旋肌群,取出股骨头,去除髋臼周围增生赘骨,后植入髋臼假体,髋关节屈曲内收内旋,之后操作同DAA组。两组术后均给予常规治疗并进行相应康复锻炼。
1.3 观察指标及评价标准 (1)手术指标:手术时间、术中出血量、切口长度,X线片测量髋臼前倾角及外展角;(2)疼痛及髋关节功能:于术前及术后1、3 d进行VAS评分,满分10分,得分越高疼痛越严重;于术前、术后2周及3、6个月时评价髋关节功能,采用Harris评分,满分100分,得分越高功能越好;(3)并发症发生情况;(4)肌肉组织损伤情况:术前及术后1、3 d抽取患者晨起空腹静脉血送检验科检测血清肌肉损伤标志物肌酸激酶(CK)及炎症反应标志物C反应蛋白(CRP);(5)骨代谢:术前及术后3个月抽取患者晨起空腹静脉血送检验科检测血清Ⅰ型前胶原氨基前肽(PⅠNP)、Ⅰ型前胶原羧基端肽(PICP)及抗酒石酸酸性磷酸酶-5b(TRACP-5b)水平。
1.4 统计学处理 所得数据采用SPSS 23.0进行统计学分析,符合正态分布的计量资料以(x±s)表示,组内比较用配对t检验,组间比较采用独立样本t检验;计数资料以率(%)表示,比较用χ检验或Fisher确切概率法,P<0.05为差异有统计学意义。
2 结果
2.1 两组一般资料比较 两组年龄、性别、Garden分型等一般资料比较,差异均无统计学意义(P>0.05),具有可比性,见表1。
2.2 两组手术指标比较 与PLA组比较,DAA组手术时间更长、术中出血量更少、切口长度更短,差异均有统计学意义(P<0.05);两组髋臼前倾角及髋臼外展角比较,差异均无统计学意义(P>0.05)。见表2。
2.3 两组VAS评分及髋关节功能评分比较 两组术前VAS评分及Harris评分比较,差异均无统计学意义(P>0.05);术后两组VAS评分及Harris评分均优于术前,差异均有统计学意义(P<0.05);术后1、3 d,DAA组VAS评分均低于PLA组(P<0.05);术后2周及3个月,DAA组Harris评分均高于PLA组(P<0.05),术后6个月,两组Harris评分比较,差异无统计学意义(P>0.05)。见表3。
2.4 两组并发症发生情况比较 DAA组中,2例出现股外侧皮神经支配区域的感觉障碍,PLA组中1例由于活动不当造成髋关节后脱位,神经麻痹2例,两组出现并发症的患者均经对症治疗后恢复,两组均无感染、下肢深静脉血栓等其他并发症发生。DAA组并发症发生率为4.44%(2/45),PLA组为6.25%(3/48),两组比较差异无统计学意义(P>0.05)。
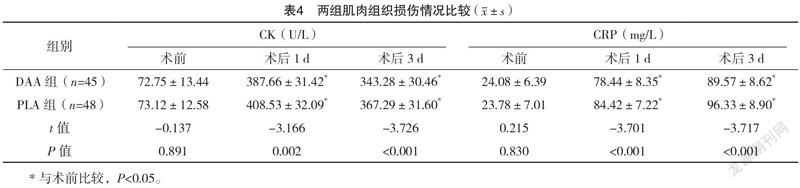
2.5 两组肌肉组织损伤情况比较 两组术前CK、CRP比较,差异均无统计学意义(P>0.05);术后1、3 d,两组CK、CRP较术前均明显升高,且PLA组均高于DAA组,差异均有统计学意义(P<0.05)。见表4。
2.6 兩组骨代谢情况比较 两组术前PINP、PICP、TRACP-5b比较,差异均无统计学意义(P>0.05);术后3个月两组PINP、PICP、TRACP-5b均优于术前,且DAA组均优于PLA组,差异均有统计学意义(P<0.05)。见表5。
3 讨论
对于存在移位的GardenⅢ、Ⅳ型股骨颈骨折,尤其是老年患者,首选人工关节置换术[9]。随着髋关节置换术的普及,手术入路的选择也成为关注的焦点。直接前入路最初由Carl Heuter于1881年提出,由Smith Peterson大量使用推广该技术[10]。在国内DAA发展较晚,且手术难度大、学习曲线长,因此发展受到一定限制[11],但近年来逐渐受到国内学者关注,并逐渐推广应用。
本研究中,PLA组手术时间短于DAA组,可能由于后外侧入路切断了外旋肌群,手术视野显露良好,易于手术操作;而直接前入路为神经肌肉间隙入路,切口小,对组织损伤小,因此术中出血量少,术后疼痛更轻,与以往文献[12-13]研究结果一致。一项Meta分析显示,随访90 d,DAA组髋关节功能恢复更好[6],另有研究显示,术后4周DAA组Harris评分更高,而长期随访两组Harris评分无差异[8,14],本研究亦得出相似结果,术后2周及3个月DAA组Harris评分均高于PLA组(P<0.05),术后6个月两组Harris评分差异无统计学意义(P>0.05),说明直接前入路有利于髋关节功能术后早期恢复。
髋关节脱位是THA的主要并发症,初次全髋关节置换术后发生率为0.3%~10%[3];有研究认为,股外侧皮神经损伤更常见,可能与手术中牵拉时间较长或暴力牵拉有关[15-16]。本研究中DAA组2例出现股外侧皮神经支配区域的感觉障碍,PLA组中1例髋关节后脱位,神经麻痹2例,两组并发症发生率差异无统计学意义,说明直接前入路手术安全性较高。CRP、CK均是组织损伤的重要标志物,CK是反映肌肉损伤程度的重要指标,周甲彬等[17]研究显示,DAA组术后CRP、CK均低于PLA组,与本研究结果一致,而Rykov等[18]则发现两种术式对CRP、CK的影响无差异,分析原因可能与手术熟练度有关。PINP、PICP为骨形成的重要指标,而TRACP-5b为骨吸收重要指标,两组术后上述指标均较术前改善,且DAA组变化更显著,说明DAA组骨代谢更好,分析原因可能为DAA组患者疼痛轻,功能恢复快,有利于患者更早地完成康复锻炼,从而改善早期骨代谢。
综上所述,直接前入路全髋关节置换术治疗GardenⅢ、Ⅳ型股骨颈骨折有利于髋关节功能早期恢复,减少患者疼痛及肌肉组织损伤,改善患者骨代谢。
参考文献
[1] GIERER P,MITTLMEIER T.Femoral neck fracture[J].Unfallchirurg,2015,118(3):259-269.
[2]牛光远.后路小切口髋关节置换术治疗老年创伤性股骨颈骨折对患者骨折愈合速度和血流动力学水平影响[J].国际医药卫生导报,2021,27(1):113-116.
[3] FALEZ F,PAPALIA M,FAVETTI F,et al.Total hip arthroplasty instability in Italy[J].Int Orthop,2017,41(3):635-644.
[4] CHECHIK O,KHASHAN M,LADOR R,et al.Surgical approach and prosthesis fixation in hip arthroplasty worldwide[J].Arch Orthop Trauma Surg,2013,133(11):1595-1600.
[5] AGTEN C A,SUTTER R,DORA C,et al.MR imaging of soft tissue altera-tions after total hip arthroplasty: comparison of classic surgical approaches[J].Eur Radiol,2017,27(3):1312-1321.
[6] MILLER L,GONDUSKY J,BHATTACHARYYA S,et al.Does surgical approach affect outcomes in total hip arthroplasty through 90 days of follow-up? A systematic review with meta-analysis[J].
J Arthroplasty,2018,33(4):1296-1302.
[7] SPAANS A J,VAN DEN HOUT J A,BOLDER S B.High complication rate in the early experience of minimally invasive total hip arthroplasty by the direct anterior approach[J].Acta Orthop,2012,83(4):342-346.
[8] MOERENHOUT K,DEROME P,LAFLAMME G Y,et al.
Direct anterior versus posterior approach for total hip arthroplasty:a multicentre, prospective, randomized clinical trial[J].Can J Surg,2020,63(5):E412-E417.
[9] BASTARD C.Femoral neck fracture[J].Rev Prat,2019,69(10):1124-1128.
[10] GALAKATOS G R.Direct Anterior Total Hip Arthroplasty[J].Mo Med,2018,115(6):537-541.
[11]张旭辉,黎丹东,李坛,等.直接前方入路全髋置换术近期疗效与学习曲线[J].中国矫形外科杂志,2018,26(8):707-711.
[12]孙正阳,郝跃东.对比两种入路行全髋关节置换术对患者的早期疗效观察及肌肉组织损伤的影响[J].中华保健医学杂志,2019,21(6):552-555.
[13]王远周,付昆,马春辉,等.不同入路人工全髋关节置换术对患者术后恢复的影响[J].局解手术学杂志,2021,30(6):525-528.
[14] REININGA I H,STEVENS M,WAGENMAKERS R,et al.
Comparison of gait in patients following a computer-navigated minimally invasive anter ior approach and a conventional posterolateral approach for total hip arthroplasty: a randomized controlled trial[J].J Orthop Res,2013,31(2):288-294.
[15] MARTIN C T,PUGELY A J,GAO Y,et al.A Comparison of Hospital Length of Stay and Short-Term Morbidity Between the Anterior and the Posterior Approaches to Total Hip Arthroplasty[J].J Arthroplasty,2013,28(5):849-854.
[16]陳明,曲彦隆.直接前方入路微创人工全髋关节置换的研究进展[J].医学综述,2017,23(9):1800-1804.
[17]周甲彬,韩桂全,崔冠兴,等.前侧入路与传统后外侧入路人工全髋关节置换术的血清学层面对比研究[J].实用骨科杂志,2018,24(2):134-138.
[18] RYKOV K,REININGA I H F,SIETSMA M S,et al.
Posterolateral vs Direct Anterior Approach in Total Hip Arthroplasty (POLADA Trial):A Randomized Controlled Trial to Assess Differences in Serum Markers[J].J Arthroplasty,2017,32(12):3652-3658.
(收稿日期:2021-07-06) (本文编辑:占汇娟)