高龄腹膜假黏液瘤患者术后发生并发症的影响因素
2022-04-01范喜文王冲张溥许洪斌马瑞卿
范喜文 王冲 张溥 许洪斌 马瑞卿
【摘要】 目的:觀察高龄腹膜假黏液瘤(pseudomyxoma peritonei,PMP)患者术后发生并发症情况并分析其影响因素。方法:选取2008年1月-2019年12月在航天中心医院黏液瘤科接受手术治疗的86例高龄PMP患者的临床资料进行回顾性分析,统计术后并发症发生率。采用多因素logistic回归分析高龄PMP患者术后并发症发生的危险因素。结果:86例高龄PMP患者中有32例患者术后出现并发症,发生率为37.2%。性别、年龄及是否接受腹腔热灌注化疗(hyperthermic intraperitoneal chemotherapy,HIPEC)与高龄PMP患者术后发生并发症无关,差异均无统计学意义(P>0.05)。术后发生并发症者手术未达到根治、既往有腹腔手术史及白蛋白水平<30 g/L比例均高于术后未发生并发症者,差异均有统计学意义(P<0.05)。多因素logistic回归分析显示,手术未达到根治、既往有腹腔手术史、白蛋白水平<30 g/L均为高龄PMP患者术后发生并发症的危险因素(P<0.05)。结论:高龄PMP患者术后并发症发生率较高,且危险因素较多,应对加强对上述因素的监测与干预。
【关键词】 腹膜假黏液瘤 高龄患者 并发症 危险因素
Risk Factors of Postoperative Complications in Elderly Patients with Pseudomyxoma Peritonei/FAN Xiwen, WANG Chong, ZHANG Pu, XU Hongbin, MA Ruiqing. //Medical Innovation of China, 2022, 19(04): 0-030
[Abstract] Objective: To investigate the postoperative complications of pseudomyxoma peritonei (PMP) in elderly patients and analyze the influencing factors. Method: The clinical data of 86 elderly PMP patients who received surgical treatment in Myxoma Department of Aerospace Center Hospital from January 2008 to December 2019 were retrospectively analyzed, and the incidence of postoperative complications was statistically analyzed. Multivariate logistic regression was used to analyze the risk factors of postoperative complications in elderly PMP patients. Result: Postoperative complications occurred in 32 cases of the 86 elderly PMP patients, with an incidence of 37.2%. Gender, age and whether hyperthermic intraperitoneal chemotherapy (HIPEC) were not associated with postoperative complications in elderly PMP patients, and there were no statistical significance (P>0.05). The proportions of surgery without radical treatment, previous abdominal surgery history and albumin level <30 g/L in patients with postoperative complications were higher than those without postoperative complications, with statistical significance (P<0.05). Multivariate logistic regression analysis showed that the risk factors for postoperative complications in elderly PMP patients were surgery without radical treatment, previous abdominal surgery history and albumin level <30 g/L (P<0.05). Conclusion: Elderly PMP patients have a high incidence of postoperative complications and many risk factors, so the monitoring and intervention of these factors should be strengthened.
[Key words] Pseudomyxoma peritonei Elderly patients Complication Risk factor
First-authors address: Aerospace Center Hospital, Beijing 100049, Chinagzslib202204011727doi:10.3969/j.issn.1674-4985.2022.04.006
腹膜假黏液瘤(pseudomyxoma peritonei,PMP)是一种罕见的腹膜恶性肿瘤,PMP以阑尾来源最为常见,年发病率约为(1~3)/106[1]。PMP的临床表现不典型,包括腹痛、腹胀、腹围增大等,其临床特征为弥漫性、进行性的黏液性腹水,但一些患者甚至发病前无任何症状[1]。由于PMP的临床表现有时较为隐匿,所以当患者就诊时黏液腹水可能已遍及全腹,处于疾病晚期,给治疗上带来较大难度。自20世纪80年代以来,细胞减灭术(cytoreduction surgery,CRS)联合腹腔热灌注化疗(hyperthermic intraperitoneal chemotherapy,HIPEC)治疗方案得以应用,极大地改善了PMP患者的预后和生活质量[2]。随着我国逐渐步入老年化社会,老年人的健康问题也日益成为焦点问题,尤其是老年患者,常患有高血压、糖尿病、高脂血癥等基础疾病,一旦罹患其他疾病时,治疗难度大、治疗周期长。就PMP而言,多数患者发病时已是中老年,其中高龄老年患者占有一定比例,以往研究主要关注PMP疾病本身,较少涉及PMP术后并发症,尤其是高龄PMP患者这一特殊人群。因此,本研究回顾性分析行手术治疗的高龄PMP患者的临床资料,探讨高龄PMP患者术后发生并发症的危险因素,现报道如下。
1 资料与方法
1.1 一般资料 选取2008年1月-2019年12月在航天中心医院黏液瘤科接受手术治疗的86例高龄PMP患者的临床资料进行回顾性分析。纳入标准:病理诊断符合PMP;接受手术治疗的患者;年龄≥70岁;临床资料完整。排除标准:卡氏评分<70分;发现肝脏、肺脏等脏器远处转移或伴随其他恶性肿瘤;随访信息严重缺失。所有患者均签署知情同意书,本研究方案获得医院伦理委员会批准。
1.2 方法 临床资料包括患者临床病理资料、围手术期数据、随访信息。每份病理报告请两名专业病理医生做出诊断核对,病理诊断标准及病理类型以PSOGI专家共识为参照[3]。纳入患者均行细胞减灭术,手术方法参照国际通用Sugarbaker腹膜切除流程[4],手术范围包括受累的腹膜和脏器切除。手术肿瘤细胞减灭程度(completeness of cytoreduction,CC)标准如下:CC-0:无肉眼可见残留;CC-1:残留肿瘤<2.5 mm;CC-2:2.5 mm≤残余肿瘤≤2.5 cm;CC-3:残余肿瘤>2.5 cm。其中CC-0/1定义为完全性细胞减灭术,即根治性手术;CC-2/3定义为非根治性手术,即姑息性手术。部分患者视身体耐受情况接受腹腔热灌注化疗,灌注化疗药物选用顺铂60~80 mg。术后所有患者均获得随访,末次随访日期为2020年1月30日。统计患者术后发生并发症情况,比较术后发生并发症患者与术后未发生并发症患者的性别、年龄、是否行HIPEC、手术是否达到根治、既往有无手术史、白蛋白水平。采用多因素logistic回归分析高龄PMP患者发生术后出并发症的危险因素。
1.3 术后发生并发症评价标准 术后并发症包括肠瘘、腹腔出血、切口感染、切口脂肪液化、腹腔感染、下肢静脉血栓形成、尿瘘、肺栓塞、腹壁切口疝。患者术后出现上述任意一项即视为发生术后并发症。
1.4 统计学处理 采用SPSS 25.0软件对所得数据进行统计分析,计数资料以率(%)表示,比较采用字2检验。应用多因素logistic回归分析识别高龄PMP患者发生术后并发症的危险因素并计算相对危险度(OR)和95%可信区间(95%CI)。以P<0.05为差异有统计学意义。
2 结果
2.1 术后并发症发生情况 86例高龄PMP患者手术治疗后,有32例患者出现术后并发症,占比为37.2%(32/86),54例患者未发生并发症,占比为62.8%(54/86)。
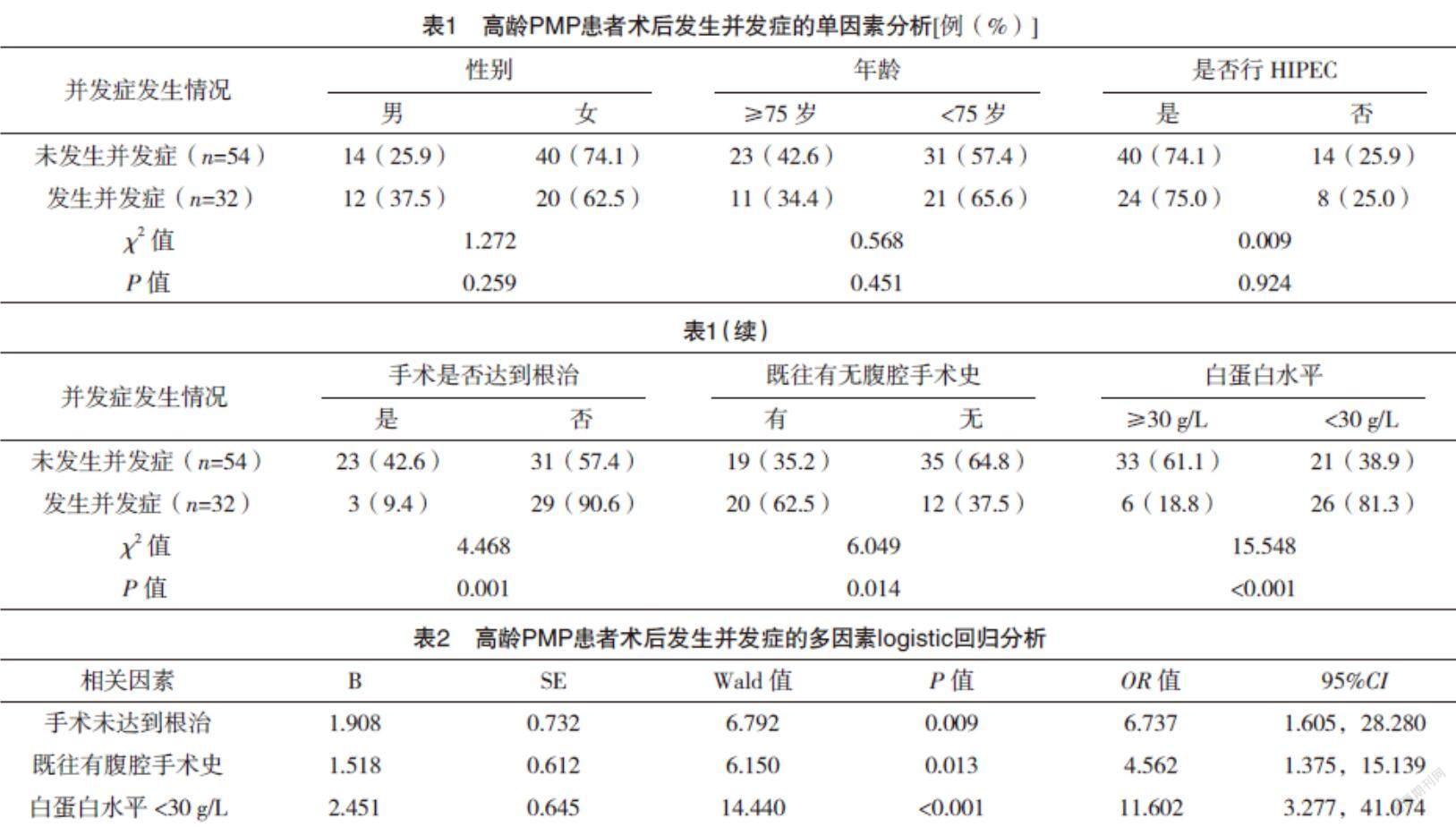
2.2 高龄PMP患者术后发生并发症单因素分析 性别、年龄及是否接受HIPEC与高龄PMP患者术后发生并发症无关,差异均无统计学意义(P>0.05)。术后发生并发症者手术未达到根治、既往有腹腔手术史及白蛋白水平<30 g/L比例高于术后未发生并发症者,差异均有统计学意义(P<0.05)。见表1。
2.3 高龄PMP患者出现术后并发症多因素分析 影响因素赋值如下,手术是否达到根治:是=0,否=1;既往腹腔手术史:无=0,有=1;白蛋白水平≥30 g/L=0,<30 g/L=1。多因素logistic回归分析显示手术未达到根治、既往有腹腔手术史、白蛋白水平<30 g/L均为高龄PMP患者发生术后并发症的危险因素(P<0.05)。见表2。
3 讨论
PMP是由黏液性肿瘤细胞通过在腹腔内种植、再分布所引起的一种临床综合征,阑尾来源的PMP占整体的80%~90%[5-7]。2016年国际腹膜表面恶性肿瘤协作组(peritoneal surface oncology group international,PSOGI)将PMP的病理分为低级别腹膜黏液腺癌(low-grade mucinous carcinoma peritonei)、高级别腹膜黏液腺癌(high-grade mucinous carcinoma peritonei)、高级别腹膜黏液腺癌伴印戒细胞(high-grade mucinous carcinoma peritonei with signet ring cells)[5-7]。CRS和HIPEC通过切除肿瘤及其累计的腹膜和腹腔脏器,从而达到减除肿瘤负荷、延长患者生存期的目的,目前已成为国际、国内公认的PMP标准治疗方案[5-8]。有研究表明CRS+HIPEC治疗后PMP的5年生存率可达50%~95%,10年生存率可达54%~70%[8-10]。gzslib202204011727隨着CRS+HIPEC治疗方案在临床中的广泛应用,其术后并发症问题日渐凸显,如术后肠瘘、吻合口瘘、腹腔内出血、切口感染等,这些并发症的出现不仅使手术疗效大打折扣,更重要的时影响患者预后,严重时甚至威胁患者生命。较早有研究报道,PMP围手术期死亡率为0~18%,并发症发生率为30%~70%[9-11]。同时也有研究表明,造成腹膜恶性肿瘤患者术后预后不良的常见危险因素包括癌变程度、腹膜切除术次数、手术时长、失血量、内脏器官切除数量、吻合口数量和不完全根治减瘤[10-13]。Saxena等[14]通过回顾性分析145例经CRS手术治疗PMP患者的临床资料,得出术后严重并发症的发生率为22%,包括:气胸、肠瘘、腹腔出血、膀胱瘘、呼吸衰竭等,并指出手术时长、回结肠造口、结肠切除及输血等因素与围手术期发生并发症相关,而年龄、性别、是否行HIPEC与并发症发生率之间未见相关性。Youssef等[15]研究结果显示,PMP患者术后严重并发症发生率为7%,3.6%的患者需二次手术。
本研究结果显示,86例高龄PMP患者经手术治疗后,有32例患者术后出现并发症,占比为37.2%(32/86)。本研究共纳入6种因素,分别为性别、年龄、是否行HIPEC、是否达到根治、既往腹腔手术史及白蛋白水平。单因素分析显示,高龄PMP患者术后并发症发病率在性别、年龄及是否行HIPEC等方面并无明显统计学差异,这与Saxena等[14]的研究结果相一致。在发生术后并发症的患者中,手术未达到根治、既往有腹腔手术史的患者占比更高,且该部分患者的白蛋白水平较低。多因素logistic回归分析显示手术未达到根治、既往有腹腔手术史、白蛋白水平<30 g/L均为高龄PMP患者发生术后并发症的独立危险因素(P<0.05)。分析其原因为,临床上非根治性手术患者一般肿瘤负荷较大[16],加之本研究纳入对象为高龄老年患者,手术风险高、难度大,所以该部分患者并发症发生率较高。而对于既往有腹腔手术史的患者而言,既往行腹腔手术一定程度上会造成腹腔内局部粘连,腹腔内结构变化,给二次手术造成一定困难,进而影响并发症发生率。白蛋白水平较低的患者机体免疫差,营养状况不佳,更易于感染病原菌[17],因此切口感染、腹腔内感染、肺炎等并发症发生率较高。术后并发症的发生严重影响手术疗效,造成患者不良预后,因此需根据患者实际病情,制定合理的治疗方案,从而降低并发症的发生率。
综上所述,本研究认为高龄PMP患者术后并发症的独立危险因素为手术未达到根治、既往有腹腔手术史及白蛋白水平较低,应在围手术期制定预防措施,降低并发症发生率。
参考文献
[1] SUGARBAKER P H.PSEUDOMYXOMA Peritonei.A cancer whose biology is characterized by a redistribution phenomenon[J].Annals of Surgery,1994,219(2):109-111.
[2] RIZVI S A,SYED W,SHERGILL R.Approach to pseudomyxoma peritonei[J].World J Gastrointest Surg,2018,10(5):49-56.
[3] CARR N J,CECIL T D,MOHAMED F,et al.A Consensus for Classification and Pathologic Reporting of Pseudomyxoma Peritonei and Associated Appendiceal Neoplasia:The Results of the Peritoneal Surface Oncology Group International(PSOGI)Modified Delphi Process[J].American Journal of Surgical Pathology,2016,40(1):14-26.
[4] SUGARBAKER P H.Peritonectomy procedures[J].Cancer Treat Res,1996,82:235-253.
[5] ELIAS D,GILLY F,QUENET F,et al.Pseudomyxoma peritonei:A French multicentric study of 301 patients treated with cytoreductive surgery and intraperitoneal chemotherapy[J].Eur J Surg Oncol,2010,36(5):456-462.
[6] ALVES S,MOHAMED F,YADEGARFAR G,et al.Prospective longitudinal study of quality of life following cytoreductive surgery and intraperitoneal chemotherapy for pseudomyxoma peritonei[J].Eur J Surg Oncol,2010,36(12):1156-1161.
[7] CARR N J,FINCH J,ILESLEY I C,et al.Pathology and prognosis in pseudomyxoma peritonei:a review of 274 cases[J].Journal of Clinical Pathology,2012,65(10):919-923.
[8] STEARNS A T,MALCOMSON L,PUNNETT G,et al.Long-term quality of life after cytoreductive surgery and heated intraperitoneal chemotherapy for pseudomyxoma peritonei:a prospective longitudinal study[J].Ann Surg Oncol,2018,25(4):965-973.gzslib202204011728[9] CHUA T C,MORAN B J,SUGARBAKER P H,et al.Early-and long-term outcome data of patients with pseudomyxoma peritonei from appendiceal origin treated by a strategy of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy[J].J Clin Oncol,2012,30(20):2449-2456.
[10] ELIAS D,HONORE C,CIUCHENDEA R,et al.Peritoneal pseudomyxoma:results of a systematic policy of complete cytoreductive surgery and hyperthermic intraperitoneal chemotherapy[J].Br J Surg,2008,95(9):1164-1171.
[11] YAN T D,BLACK D,SAVADY R,et al.A systematic review on the effificacy of cytoreductive surgery and perioperative intraperitoneal chemotherapy for pseudomyxoma peritonei.Ann Surg Oncol[J].2007,14(2):484-492.
[12] GUSANI N,CHO S,COLOVOS C,et al.Aggressive surgical management of peritoneal carcinomatosis with low mortality in a high-volume tertiary cancer center[J].Ann Surg Oncol,2008,15(3):754-763.
[13] HANSSON J,GRAF W,PAHLMAN L,et al.Postoperative adverse events and long-term survival after cytoreductive surgery and intraperitoneal chemotherapy[J].Eur J Surg Oncol,2009,35(2):202-208.
[14] SAXENA A,YAN T D,CHUA T C,et al.Critical Assessment of Risk Factors for Complications After Cytoreductive Surgery and Perioperative Intraperitoneal Chemotherapy for Pseudomyxoma Peritonei[J].Annals of Surgical Oncology,2010,17(5):1291-1301.
[15] YOUSSEF H,NEWMAN C,CHANDRAKUMARAN K,et al.Operative findings,early complications,and long-term survival in 456 patients with pseudomyxoma peritonei syndrome of appendiceal origin[J].Dis Colon Rectum,2011,54(3):293-299.
[16] MA R,LU D,WANG B,et al.Complete Cytoreductive Surgery vs.Debulking Surgery for pseudomyxoma peritonei of appendiceal origin:A propensity score-matched study based on a single-center experience[J].European Journal of Surgical Oncology,2021,47(9):2369-2376.
[17] BARATTI D, KUSAMURA S, IUSCO D,et al.Postoperative complications after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy affect long-term outcome of patients with peritoneal metastases from colorectal cancer:a two-center study of 101 patients[J].Dis Colon Rectum,2014,57(7):858-868.
