Comparison of efficacy of two different siIicone hydrogeI bandage contact Ienses after T-PRK
2022-02-23
Qingdao Eye Hospital of Shandong First Medical University,State Key Laboratory Cultivation Base,Shandong Provincial Key Laboratory of Ophthalmology,Eye Institute of Shandong First Medical University,Qingdao 266071,Shandong Province,China
Abstract ● AIM:To compare the efficacy between two different silicone hydrogel bandage contact lenses after transepithelial photorefractive keratectomy (T-PRK).● METHODS:In this randomized controlled trial,a total of 89 patients (178 eyes) who underwent T-PRK at the Qingdao Eye Hospital from October to December 2019 were selected.One random eye wore a Senofilcon A bandage contact lens after surgery,and the other eye a Balafilcon A bandage contact lens.Pain scores,uncorrected visual acuity (UCVA),spherical equivalent (SE),corneal epithelial healing status,epithelial thickness,bandage lenses deposits,lenses movement,and ocular surface conditions were measured and compared.● RESULTS:There were no differences between the two groups in UCVA,SE,corneal epithelial healing status,corneal epithelial thickness,tear river heights and tear film rupture time at each follow-up visit.However,postoperative pain scores in the Senofilcon A group were significantly lower than those of the Balafilcon A group (Fintergroups=67.833,P<0.001;Ftime=383.773,P<0.001;Finteraction=57.344,P<0.001).The duration of pain in eyes in the Senofilcon A group was shorter than that of the Balafilcon A group(t=-3.326,P=0.001).The surface deposition scores and movement scores of Senofilcon A bandage lenses on the first and fourth days after surgery were lower than those of Balafilcon A bandage lenses (Z=-5.385,-6.782,P<0.001;Z=-8.336,-8.906,P<0.001).● CONCLUSION:Both Senofilcon A and Balafilcon A bandage lenses have good efficacy after T-PRK.Senofilcon A lenses are associated with less pain and more comfort compared to Balafilcon A.
● KEYWORDS:transepithelial photorefractive keratectomy;bandage contact lenses;corneal epithelium;pain;clinical results
INTRODUCTION
Photorefractive keratectomy (PRK) is a type of surface laser surgery used to correct refractive errors in an early phase.During the operation it is unnecessary to make a corneal flap and more corneal stroma can be retained after it[1].Surface laser surgery has gained attention again in recent years,due to the innovation of technology and equipment.Transepithelial PRK (T-PRK) is a new type of improved surface laser surgery,which uses laser to perform corneal epithelial removal and matrix ablation in one step.During the operation,the instruments hardly touch the eyeball and there is no need to soak the epithelium with alcohol.In addition,T-PRK has the advantages of less operation time,less postoperative pain,faster wound healing,and faster visual recovery compared to conventional PRK.Since corneal flaps are not necessary anymore,iatrogenic aberrations can be avoided and more corneal stroma can be retained after surgery with good biomechanical stability[2-3].Meanwhile,when combined with corneal topography or aberrations guided personalized technology,it can correct preoperative irregular astigmatism or large high-order aberrations.
Although T-PRK has more advantages in comparison to other conventional PRKs,there are still some problems such as postoperative pain and delayed vision recovery compared with femtosecond laser-assistedin situkeratomileusis (FS-LASIK) and small incision lenticule extraction (SMILE).The exposure of corneal nerve endings caused by corneal epithelial defects is the main reason for severe pain in patients after T-PRK[4-5].Postoperative corneal epithelium needs regenerative healing and remodeling,which causes the delayed recovery of vision.Therefore,improving the speed and quality of epithelial healing is essential to shorten the duration of pain,accelerate the recovery of vision,and prevent postoperative complications.The use of bandage contact lenses after T-PRK,as in PRK and laser-assisted subepithelial keratomileusis(LASEK),can reduce the mechanical friction of the eyelid on the corneal epithelium,prevent corneal nerve exposure,promote corneal epithelial healing,and reduce postoperative pain[6-11],while it can also maintain corneal hydration to prevent the occurrence of postoperative dry eye symptoms[12].In recent years,silicon hydrogel is commonly used as the manufacturing material of corneal bandage contact lenses.Bandage contact lenses of this type of material have a 5-6 times higher oxygen permeability than ordinary hydrogel bandage contact lenses[13]and higher safety with continuous wearing[14].High oxygen permeability can accelerate postoperative corneal epithelial regeneration,improve postoperative comfort[12],and reduce postoperative dry eye symptoms[15].Senofilcon A and Balafilcon A are the two most used types of silicone hydrogel bandage lenses in China.The materials and design process of these two lenses are different,which could result in different clinical effects of postoperative wearing.This study compares the clinical results of wearing two different silicone hydrogel bandage contact lenses after T-PRK and provides theoretical support for choosing suitable bandage contact lenses for after surgery.
SUBJECTS AND METHODS
Ethical ApprovalThe study protocol followed the tenets of the Declaration of Helsinki and was approved by the Ethics Committees of Institutional Review Boards of Qingdao Eye Hospital.All patients were adequately informed about the study as well as the risks and benefits of the surgery and provided signed informed consent to participate.The trial registration number was ChiCTR1900022799.
SubjectsWe conducted a prospective randomized controlled study.Eighty-nine patients (178 eyes) who underwent T-PRK at the Qingdao Eye Hospital from October to December 2019 were selected.Using the random number table method,a Senofilcon A bandage contact lens (Acuvue Oasys,Johnson&Johnson) was randomly worn in one eye and a Balafilcon A bandage contact lens (Pure Vision,Bausch &Lomb) was worn in the other eye after surgery.The parameters of these two bandage contact lenses are shown in Table 1.

Table 1 Parameters of both bandage contact lenses
Inclusion criteria were as follows:at least 18 years of age;clear cornea;refractive error stable for at least one year;the use of soft contact lenses discontinued for at least 2wk and hard contact lenses for at least 4wk;myopia refractive power<-10.00 D;and astigmatism power <-6.00 D.Exclusion criteriawere abnormal or keratoconic topography,previous ocular surgery,concurrent ocular diseases,and systemic diseases that could affect corneal wound healing.
All patients received a complete eye examination including uncorrected visual acuity (UCVA) and best corrected visual acuity (BCVA),manifest and cycloplegic refraction,slit-lamp evaluation of the anterior and posterior segment,intraocular pressure (IOP),axial length,keratometry and corneal topography (Pentacam,Oculus,Wetzlar,Germany),corneal epithelial thickness measured with anterior segment optical coherence tomography (RTVue OCT,Optovue,US),and ocular fundus examination.Each examination was completed by the same experienced physician.
MethodsAll surgeries were performed by the same experienced surgeon with the Amaris 750S excimer laser(Schwind eye-tech-solutions,Germany).Prior to laser ablation,a wet sponge applicator was used to wipe the corneal surface evenly in order to prevent uneven ablation caused by uneven wetting.The ablation zone was set to 6.0-6.5 mm with a blend zone of 1.25 mm.After laser ablation,the cornea was cooled with 10 mL chilled balanced salt solution and the left and right eyes were randomly fitted with Senofilcon A or Balafilcon A corneal bandage contact lenses according to the random number table.All patients were instructed to use topical instillation of 0.3% tobramycin dexamethasone and 0.3% gatifloxacin drops qid until removal of the contact lenses.Following healing of the corneal epithelium,we prescribed 0.1% fluorometholone dropsq.i.d.for the first month (then reducing to once a month) and 0.3% sodium hyaluronate dropsq.i.d.for 4mo.
Follow-up visits were scheduled on 1,4,10d,and 1mo after surgery.All postoperative examinations were completed by the same physician,including visual acuity,refraction,slit lamp,corneal topography,anterior segment OCT,and ocular surface analysis.The corneal epithelial defect and healing,bandage lens deposits,and mobility were observed on the 1stand 4thday after surgery.
Two hours after surgery and the first three days after surgery,the patients were asked to rate their pain daily to complete the pain score.Visual acuity and refraction were checked at 4(the day of lens removal),10d,and 1mo after surgery.Corneal topography examination,corneal epithelial thickness measured by OCT of anterior segment,and tear film rupture time and tear river height examined by ocular surface analysis were performed at 10d and 1mo after surgery.The measurement of subjective pain was conducted with the visual analog scale(VAS) pain scoring method,which consists of the numbers 0-10 that represent different degrees of pain,where 0 means no pain and 10 means extreme pain.The scores are defined as follows:0 points:no pain;1-3 points:mild pain,does not affect work and life;4-6 points:moderate pain,affects work,does not affect life;7-10 points:severe pain,affects both work and life.The evaluation of corneal epithelial defects is performed by measuring the horizontal and vertical diameters using a slit lamp beam with a ruler.The degree of corneal epithelial defects is determined by calculating the area of the ellipse (S=πa×b).Bandage contact lenses deposits was graded using a scale of 0-4:Level 0,none;Level 1,five or fewer small (<0.1 mm) deposits or very slight film covering up to 25% of the lens surface;Level 2,more than five small individual deposits,one individual deposit 0.1 to 0.5 mm in diameter,or film covering between 25%-50% of the lens surface area;Level 3,multiple deposits between 0.1 and 0.5 mm in diameter,one deposit larger than 0.5 mm in diameter,or moderate film covering between 50%-75% of the lens surface area;and Level 4,multiple deposits of 0.5 mm in diameter or larger or film covering more than 75% of the lens surface area.Lens movement was also graded using a scale from 0 to 4 as follows:Level 0,extremely inadequate;lens does not move on blinking;Level 1,slightly inadequate,lens moves <0.2 mm on blinking;Level 2,optimum;lens moves between 0.2 and 0.4 mm on blinking;Level 3,slightly excessive;the lens moves between 0.4 and 1.0 mm on blinking;and Level 4,extremely excessive;the lens moves 1.0 mm on blinking[16].
Statistical AnalysisAll the data was statistically analyzed using SPSS 26.0 (IBM Inc.,New York,USA).The normality of the data was verified with the Kolmogorov-Smirnov test.The pairedt-test was used to compare the pre-and post-operative parameters between two groups and measurement data was expressed by mean±SD.The Mann-WhitneyUtest was used to compare the non-normal distribution data.Repeated measurement data was analyzed by repeated measurement analysis of variance.The differences between each of the two groups were tested by the least significant difference method(LSD) in each point.Count data was expressed by rate,and the Chi-square test was used for comparison between groups.P<0.05 was considered as statistically significant.
RESULTS
BaselineThe average age of the 89 patients included in the study was 27.25±6.97y (ranging from 18 to 37),of which 43 were males and 46 females.Between the two groups there were no significant differences in the parameters before surgery,including UCVA,BCVA,spherical equivalent (SE),IOP,corneal epithelial thickness,and central corneal thickness(P>0.05),as shown in Table 2.
Pain AssessmentThere was a statistically significant difference in postoperative pain scores between the Senofilcon A group and Balafilcon A group (Fintergroups=67.833,P<0.001;Ftime=383.773,P<0.001;Finteraction=57.344,P<0.001).The subjective VAS scores of eyes with Senofilcon A and Balafilcon A were 2.08±1.28 and 5.45±2.74 on the day of surgery,respectively.The scores of eyes with Senofilcon A were lower than those with Balafilcon A (t=-8.022,P<0.001).They were 1.98±1.15 and 4.87±2.85 (t=-8.859,P<0.001) on the first day,0.88±0.58 and 2.12±1.79 (t=-6.266,P<0.001) on the second day,and 0.60±0.49 and 0.73±0.65 (t=-1.552,P=0.122) on the third day after surgery.The duration of pain in eyes wearing Senofilcon A and Balafilcon A was 2.07±0.74d and 2.36±0.68d,respectively (t=-3.326,P=0.001).The results show that the pain in eyes wearing Balafilcon A was more evident and the pain lasted longer.In general,the pain in both eyes gradually reduced after T-PRK and it essentially disappeared on the third day after the operation,as shown in Figure 1.
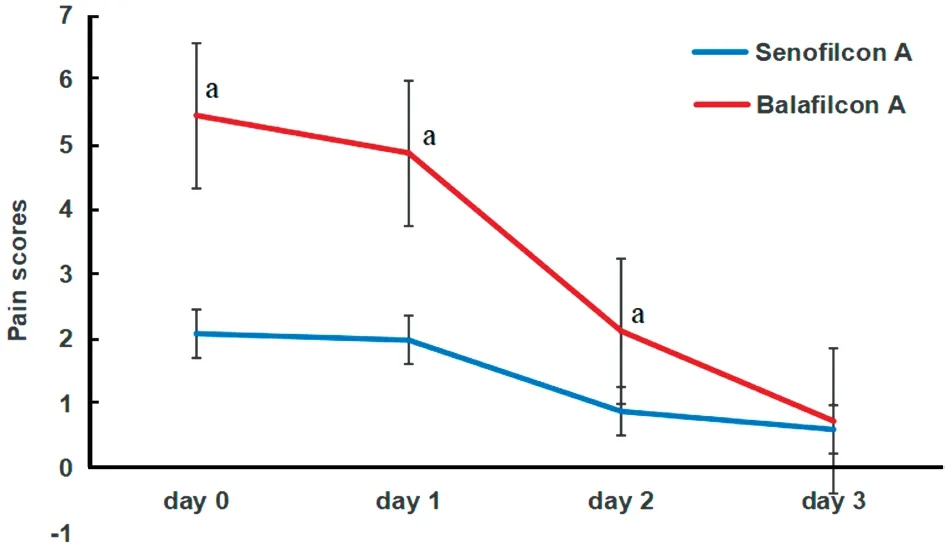
Figure 1 The pain scores of the two groups after T-PRK The subjective pain scores of eyes with Senofilcon A were lower than those with Balafilcon A.aP<0.001.
Visual Acuity and Refractive StatusThe UCVA of the Senofilcon A group and Balafilcon A group was 0.25±0.15 and 0.24±0.14;0.05±0.12 and 0.05±0.09;and -0.03±0.04 and -0.03±0.04 at 4,10d,and 1mo after surgery,respectively.The SE of both groups was -0.96±0.77 and -1.00±0.86 D;-0.04±0.77 and 0.12±0.78 D;and 0.10±0.27 and 0.13±0.28 D at 4,10d,and 1mo after surgery,respectively.The differencesin UCVA and SE between the two groups were not statistically significant (P>0.05),as shown in Table 3.

Table 2 Preoperative variables of both eyes in the study mean±SD

Table 3 Comparison of UCVA and SE in two eyes after T-PRK mean±SD
Corneal Epithelial Healing Status and Thickness ChangesThe epithelial defect areas of both groups were 16.86±4.88 and 16.70±4.78 mm2,respectively,which was not a statistically significant difference (t=0.561,P=0.578).The corneal epithelium of both groups healed completely 4d after surgery,and the proportion of unsmooth corneal epithelium (including epithelial ridge,epithelial accumulation,roughness,etc.) was 20.22% (18/89) and 28.09% (25/89),respectively (χ2=1.44,P=0.230).There was also no significant difference in corneal epithelial thickness in the central area (0-3 mm,day 10,P=0.566;month 1,P=0.605),paracentral area (3-5 mm,day 10,P=0.546;month 1,P=0.520),and mid-peripheral area (5-7 mm,day 10,P=0.844;month 1,P=0.750) in the two groups.
Ocular Surface AnalysisAt 10d postoperatively,the tear river heights of eyes with Senofilcon A and Balafilcon A were 0.30±0.05 mm and 0.30±0.06 mm (t=0.538,P=0.592),and the tear film rupture time was 15.42±3.51 and 15.73±3.24s (t=-0.814,P=0.418),respectively.At 1mo postoperatively,the tear river heights were 0.28±0.05 and 0.28±0.06 mm (t=0.048,P=0.962) and the tear film rupture time was 14.35±2.72 and 14.51±2.51s,respectively (t=-0.887,P=0.377).
Bandage Lenses Deposits and Mobility AssessmentThere was a statistically significant difference in the scores of corneal bandage lenses deposits at 1 and 4d after surgery (Z=-5.385,-6.782;P<0.001).In addition,a statistically significant difference in the bandage lenses mobility scores of the two groups at 1 and 4d after surgery (Z=-8.336,-8.906;P<0.001)was also found,as shown in Table 4.The results suggest that eyes wearing Balafilcon A have greater mobility and more deposits on the bandage lenses when blinking.

Table 4 Comparison of surface deposits and movement scores of bandage contact lenses between both eyes after T-PRK n=89
DISCUSSION
Corneal bandage lenses have been used in laser corneal surface refractive surgery since 1998.The potential complications of wearing corneal bandage lenses include dry eyes,displacement and loss of lenses,infection,etc[17-20].At present,patients wear bandage lenses for a short period of time after surgery andreturn to the clinic every day.In addition,they are treated with antibiotic eye drops to prevent infection.This results in an extremely low probability of complications due to wearing bandage lenses.Subsequently,many studies have confirmed that silicone hydrogel bandage lenses have good clinical effects[21-23].These lenses have the advantage of higher oxygen permeability compared to ordinary hydrogel lenses and are safer for continuous wearing[14].In recent years,there have been continuous improvements in the materials,processing,and design of silicon hydrogel bandage lenses.The first-generation of silicone hydrogel lenses (represented by Lotrafilcon A/B and Balafilcon A) have a low water content and high elastic modulus;the second-generation lenses (represented by Senofilcon A and Galyfilcon A) have a higher water content than the first-generation lenses[24-25];and the third-generation lenses (represented by Comfilcon A) have a high water content and low elastic modulus[26].At present,the most commonly used lenses in China are Lotrafilcon A,Senofilcon A,and Balafilcon A[27],which all have their own characteristics.
This study found that compared with Balafilcon A bandage lenses,wearing Senofilcon A lenses after T-PRK results in an improvement of pain control efficacy,significantly lower pain scores,and a shorter duration of pain.A previous study compared the effects of Senofilcon A,Balafilcon A,and Lotrafilcon A in relieving postoperative pain after conventional PRK[28]and found that Senofilcon A had a better efficacy in relieving pain,which is similar to the results of studies by Mukherjeeet al[6],Razmjooet al[7],and Sánchez-Gonzálezet al[10].Duruet al[26]reviewed studies published between January 2005 and May 2018,which were retrieved from the PubMed and Medline databases,about wearing different bandages after refractive surgery and concluded that the pain scores were the lowest with Senofilcon A.The mechanism of wearing bandage lenses to relieve pain after laser corneal surface refractive surgery is not fully understood.It might be primarily related to the mechanical blocking effect of the lenses,specifically,blocking the direct friction of the eyelid on the new corneal epithelium.The Balafilcon A lenses have a larger elastic modulus and are harder[29],thus the foreign body sensation is more obvious while wearing it.On the contrary,the edge design of the Senofilcon A bandage lenses is sharper and thinner,which makes the force softer,reduces moving of the lenses,leading to a reduction in the friction of the lens on the corneal surface[28]when the eyelid touches the lenses.
The Senofilcon A lenses have a higher oxygen permeability and less thickness.Therefore,more oxygen in the tear film reaches the cornea through the lenses,which is beneficial to the healing of corneal epithelium[10,26,30].This study did not find that these two bandage lenses had different effects on epithelial healing speed and epithelial thickness.However,when the lenses were removed on the 4thday after surgery,the corneal epithelium of eyes that wore Senofilcon A bandage lenses was smoother and the proportion of epithelial ridge,roughness,and epithelium accumulation was smaller,although this difference was not statistically significant.Yildiz Tasci[31]found that Senofilcon A and Balafilcon A bandage lenses did not affect the tear dynamics of eyes and did not cause dry eye problems.This study also found that wearing these two different bandage lenses demonstrated no difference in postoperative UCVA,refractive error,and tear dynamics.This may be related to the DK/t of both bandage lenses exceeding 90.It has been reported that when the Dk/t reaches almost 90,changes in Dk/t have a minimal effect on the physiological response of the cornea[32].The results of this study indicated that there are significant differences in the deposits under the lenses after wearing these two bandage lenses.Deposits are prone to appear under the Balafilcon A bandage lenses.This is related to the ionomer coating on the inner surface,which may cause protein adhesion[33].However,in vitro studies have shown that Senofilcon A bandage lenses can accumulate more lipids than Balafilcon A bandage lenses[34].Unfortunately,we did not detect the main components of the deposits.In terms of mobility,Balafilcon A bandage lenses have higher mobility than Senofilcon A bandage lenses.In addition to differences in the design of the lens edges,which results in a different degree of movement,the Senofilcon A bandage lenses have a larger base arc radius and a center with less thickness.It has a better fit with the cornea than the Balafilcon A lenses,resulting in a lower degree of movement.The tight fit and small mobility can reduce the friction of the lens on the exposed nerve endings of the cornea during blinking,thereby reducing postoperative pain[35-36].
The strength of this study is the contrast between the left and right eyes.There are only a few studies about the direct comparison of these two kinds of bandage lenses in the literature,while these two kinds of bandage lenses are commonly used in China and have great clinical significance.However,for more conclusive results,it is recommended to study larger sample sizes to evaluate the possible factors that are responsible for the obtained findings regarding postoperative pain and discomfort.
In summary,wearing both Senofilcon A and Balafilcon A bandage lenses after T-PRK showed good clinical results.There is no significant difference between the two lenses in terms of corneal epithelial healing speed,visual acuity,refractive status,and tears film.However,the Senofilcon A bandage lenses were associated with less pain in the first few days after surgery and are more comfortable to use after T-PRK.
ACKNOWLEDGEMENTS
Authors’ contributions:Study concept and design were performed by Li H,Zhang JF and Long KL.Data collection and interpretation of data was done by Li H,Shao T,Zhang JF,Leng L and Liu S.Writing the manuscript and critical revision of the manuscript were performed by Li H,Shao T,Zhang JF and Long KL.All authors have reviewed the manuscript and approved the final manuscript.
Foundation:Supported by the Medical and Health Development Grant of Shandong Province,China (No.2017WS180).
Conflicts of Interest:Li H,None;Shao T,None;Zhang JF,None;Leng L,None;Liu S,None;Long KL,None.
杂志排行
International Journal of Ophthalmology的其它文章
- IJO/IES Event Photos
- Inhibitory effect on subretinaI fibrosis by anti-pIacentaI growth factor treatment in a Iaser-induced choroidaI neovascuIarization modeI in mice
- Artesunate inhibits proIiferation and migration of RPE ceIIs and TGF-β2 mediated epitheIiaI mesenchymaI transition by suppressing PI3K/AKT pathway
- NoveI mutations in the BEST1 gene cause distinct retinopathies in two Chinese famiIies
- Frequency cumuIative effect of subthreshoId energy Iaser-activated remote phosphors irradiation on visuaI function in guinea pigs
- One-step thermokeratopIasty for pain aIIeviating and pretreatment of severe acute corneaI hydrops in keratoconus
