One-step thermokeratopIasty for pain aIIeviating and pretreatment of severe acute corneaI hydrops in keratoconus
2022-02-23
INTRODUCTION
Keratoconus is a progressive and non-inflammatory ectatic corneal disorder characterized by central corneal thinning,protrusion,and ever-increasing irregular astigmatism
.Acute corneal hydrops (hydrops cornea),which is the severe stage of the disease,occurs in approximately 3%of keratoconus cases and is caused by rupture in the Descemet membrane and endothelium
.Aqueous could enter the corneal stroma and epithelium and cause corneal edema,leading to markedly decreased vision associated with intense pain
.The initial symptom of corneal hydrops is often epiphora,followed by intense photophobia,pain and marked vision loss
.A history of coughing or severe eye friction may be present
.Slit-lamp examination usually shows conjunctiva hyperemia,obvious microcystic edema of the corneal epithelium,and cystoid or fissure-like edema in the stroma
.Edema may involve different positions and areas of the cornea.The degree of acute keratoconus edema can be divided into three grades according to the extent of edema:grade 1,edema limited to a diameter of 3 mm;grade 2,edema limited to a diameter of 3 to 5 mm;and grade 3,edema with a diameter more than 5 mm
.The time of edema regression and the final best-corrected visual acuity (BCVA) of patients were inversely proportionate to the range of edema
.
Most cases of acute keratoconus edema can subside spontaneously within 2 to 4mo
,however,vision and comfort are also important during such a long duration.Persistent corneal edema is also more likely to lead to complications,such as infection,neovascularization,and even corneal perforation,resulting in markedly reduced visual acuity and increased risk of intraocular infection
.Therefore,the purpose of treatment is to promote the regression of edema and reduce or eliminate complications as safely as possible.The treatment of acute keratoconus hydrops includes drugs and surgical intervention such as anterior chamber gas injection,penetrating keratoplasty (PKP),and deep lamellar keratoplasty
.Surgical intervention is necessary for nonresolution of corneal edema to avoid complications and improve visual acuity earlier
.Reducing severe pain as soon as possible is another goal;therefore,intervention is usually performed quickly.At present,acrylic acid and acrylic acid combined with amniotic membrane are rarely used.Although there is a risk of immune rejection,PKP is still a popular method that avoids scars and improves vision
.However,deep anterior lamellar keratoplasty (DALK) has become popular and is generally accepted as the best choice for treating keratoconus
.For acute keratoconus patients with corneal hydrops,however,routine DALK could be difficult because of the potential for perforation caused by Descemet membrane fractures and intrastromal fissures
.PKP treatment after acute keratoconus hydrops involves a higher risk of endothelial rejection and donor graft survival time compared to DALK
.
A simple and effective treatment for hydrops is necessary to explore to reduce the pain and as a preliminary procedure before DALK.Drugs can be used to reduce discomfort symptoms,and air injection in the anterior chamber can be used to accelerate the regression of edema
.Intracameral injection of air or expansile gas has been advocated in the past decade
.However,this procedure must be repeated many times,has low compliance,and involves many complications
.Arentsen
has reported six patients with keratoconus were treated with penetrating keratoplasty following thermokeratoplasty in 1977.As presented in a previous study,anterior chamber paracentesis combined with thermokeratoplasty can provide an opportunity for hydrops cornea patients to undergo DALK
.In this study,we evaluated simplified one-step thermokeratoplasty without anterior chamber paracentesis to relieve intense pain and corneal edema as early as possible to provide more surgical options for patients with severe acute corneal hydrops.Using this method,extremely severe hydrops (grade 3,which involves edema larger than 5 mm in diameter) can be simply controlled within a short time.
SUBJECTS AND METHODS
This retrospective study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Peking University Third Hospital.All study participants provided informed consent.
Princess! youngest princess!Open the door for me!Dost thou not know what thou saidst to meYesterday by the cool waters of the fountain?Princess, youngest princess!Open the door for me!
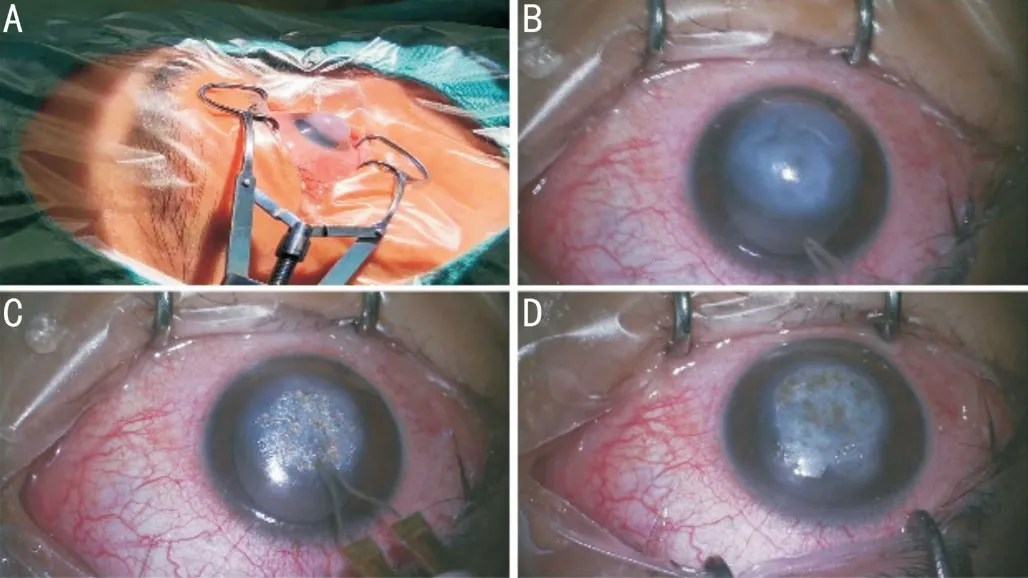
Patients were treated with simplified one-step thermokeratoplasty immediately.After peribulbar anesthesia,usually a mixture of lidocaine 2% and bupivacaine 0.75%,cautery was performed to shrink the central cornea and flatten the raised region.A 3-mm curved probe with the temperature between 90°C and 95°C was applied to the thinnest cone apex and then gradually expanded from the center to the periphery in a spiral manner until the corneal collagen at the cone area shrink due to heat,and the entire corneal edema area was cauterized with a cautery device.The top of the corneal cone formed a mild contracted white scar,the protruding cornea was flattened.If there was still an unburned edema area,repeated the previous process to cover the cone completely.General all areas of corneal edema should be burnt until the curvature of the anterior corneal surface returns to its normal shape.The cauterization range was slightly covered the oedema area and a corneal contact lens was used (Figure 1).The probe was avoided to apply on the same area more than once.Applications should be gentle and short (less than one second).The procedure is shown in the Supplemental Video l.
Just then a strange sound woke her--someone was speaking not very far away; and opening her eyes she found herself in a room she had never seen before, which was certainly not nearly so splendid as those she was used to in the Beast s palace
Benson, who is also 46, and devises grade school curriculums, said she worried her husband would judge her if she continued to eat meat, “but we talked it out and he is not proselytizing36
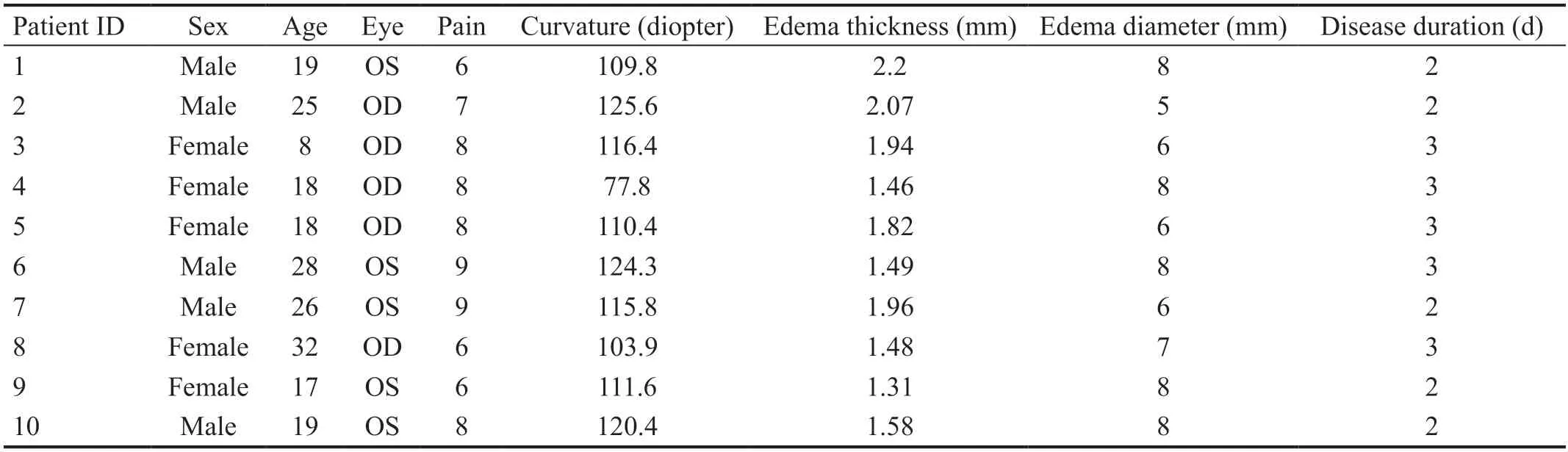
In all patients,five patients were male and the other five were female.The mean age was 21y (standard deviation,±2.17y;range,8-32y).Before thermokeratoplasty treatment,all patients experienced severe pain with a mean VAS score of 7.5(range,6-9).All patients' visual acuity was classified as finger counting.All patients presented obvious corneal hump and serious central corneal swelling (diameter,5-8 mm),and the corneal curvature range was 77.8 to 125.6 diopter (D).ASOCT demonstrated distinct corneal thickening and intrastromal ruptures.All patients were confirmed with Descemet membrane breaks.Descemet membrane detached from the stroma occurring in eight participants.The demographics,VAS scores,corneal parameters and the duration of the acute corneal hydrops of all 10 patients before thermokeratoplasty are shown in Table 1.
RESULTS
Several weeks later,corneal oedema was absorbed completely and Descemet membrane fractures were healed.Modified DALK was performed for eight patients and for two patients without subsequent corneal transplantation.The DALK procedure involved using a Hessburg-Barron vacuum trephine(diameter,7.5 mm) to dissect four-fifths of the thickness of the corneal lamellae.The lamellae were cut off using a knife along the stromal fibers.A full-thickness corneal graft 8.0 mm in diameter with no endothelium was sutured to the recipient using a gradual pressure technique to decrease the occurrence of folds in the central cornea
.Complications during and after surgery,such as Descemet membrane breaks during the operation and recipient opacity,were evaluated.Graft transparency,visual acuity,corneal curvature,corneal opacity,and immunological rejection were recorded for 6 to 12mo after DALK.
The corneal curvature decreased significantly and the average measurements were recorded as 80.62 D and 65.33 D at 1wk and 1mo after treatment,respectively.The absorption of the corneal edema in all patients was visibly,and the average central corneal thickness changed from 0.90 mm at 1wk after treatment to 0.59 mm at 1mo after treatment.The Descemet membrane breaks and stromal fissures narrowed or disappeared over time.One month later,corneal edema almost absorbed and the stroma flat,without obvious scar.At 4 to 6wk,ASOCT pictures showed the disappearance of the Descemet membrane rupture.Compared to the normal,the corneal stroma showed slightly high-density.The effects of one-step thermokeratoplasty for acute corneal hydrops are shown in Figures 3 and 4.
No, said the man; what should I have wished from him? Ah! said the woman, it s dreadful to have to live all one s life in this hut that is so small and dirty; you ought to have wished for a cottage
After thermokeratoplasty,the pain was obviously alleviated,with a mean VAS score of 2.6 (range,2-3) at 1d after treatment.Within 1wk after treatment,the pain had almost disappeared,with a VAS score of 1.2 (range,1-2).However,the pain was not relieved or was even worse on the day of surgery,with a mean score of 8.6 (range,7-10).Changes in pain experienced by all patients before thermokeratoplasty,on the day of surgery,1d after surgery,and 1wk after surgery are shown in Figure 2.


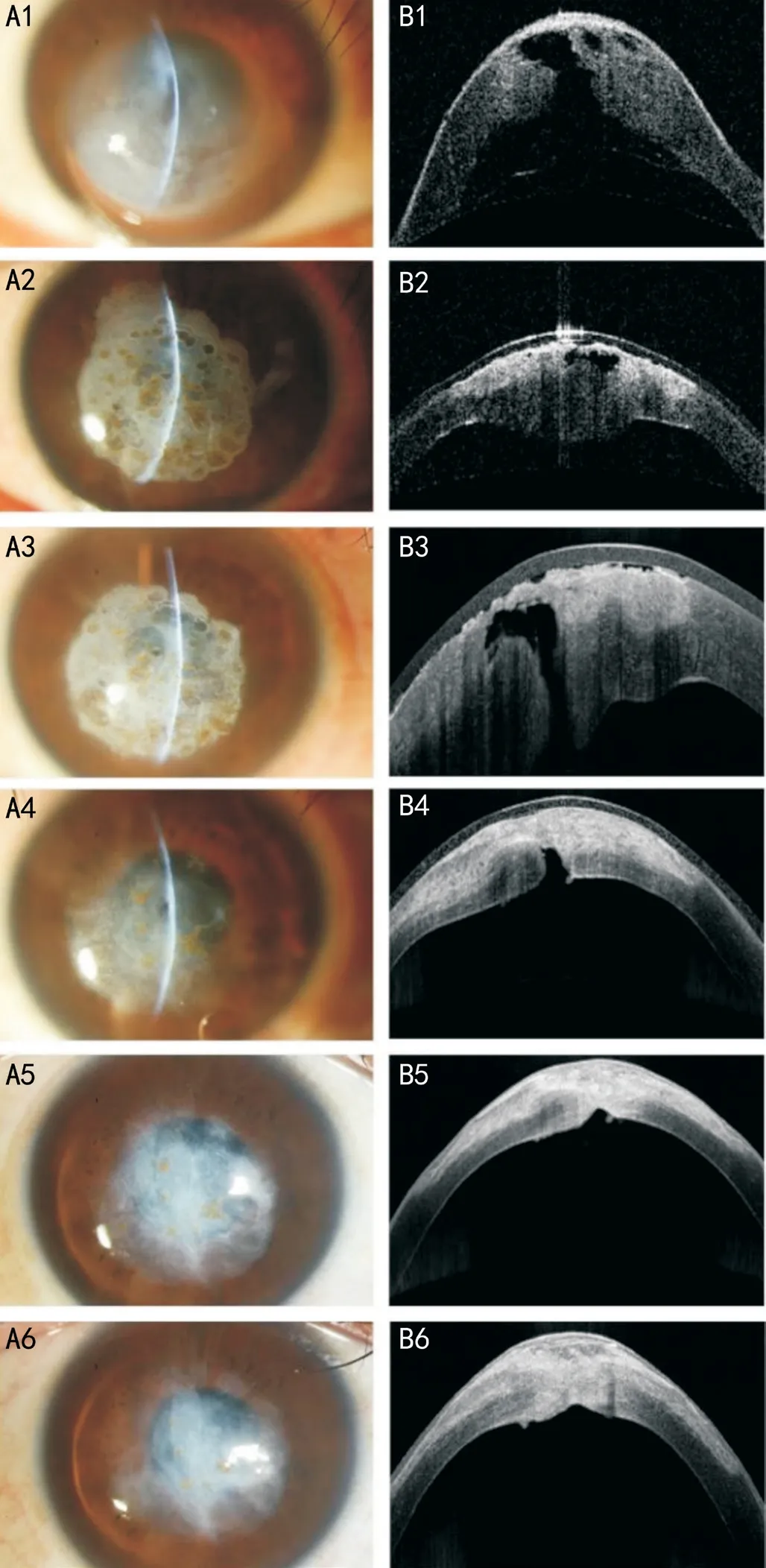
Eight patients were successfully treated with DALK approximately 3 to 6wk after thermokeratoplasty.During the procedure,slight intrastromal ruptures were found,and there were only some stromal layers between the Descemet membrane and the epithelium.After treating with DALK,Descemet membrane break could also be found in some patients.The leakage of aqueous humor from the central recipient was found in two patients without corneal perforation.We did not perform any special treatment for leakage during DALK.The next day after the procedure,no aqueous humor was seen between the interface of the donor graft and the recipient.With medication,the graft became transparent 1wk later.The recipients were completely clear in eight eyes 1mo later,with no haze or folds.Minor opacities similar to fractures of the Descemet membrane were found at the central cornea in five patients.After 6mo,the central opacity in five patients faded or disappeared.After 12mo,the BCVA was increased to 20/30.During the follow-up,no immune rejection was recorded.
Postoperatively,glucocorticoids and 1% prednisolone acetate eye drops were administered four times per day;then,they were tapered every week.Changes in the corneal curvature and thickness and the size and morphology of Descemet membrane breaks were detected by corneal topography and ASOCT weekly after thermokeratoplasty.
You don t know about that, said the youth; I know well enough what it is that lies so heavy on your mind, and I know also of a plan to get the money paid
Two patients did not undergo any subsequent corneal transplantation after one-step thermokeratoplasty because the corneal morphology tended to stabilize and visual acuity recovered to meet the daily activities of patients.During the follow-up lasting 1 to 2y,the thermokeratoplasty scars faded and visual acuity was improved.
DISCUSSION
Keratoconus is the most common ongoing corneal dilatation in adolescents
.The main pathology is reduced corneal intensity and thickness,which can be attributed to the disparate distribution and decreased stromal lamellae
.Acute corneal hydrops is a frequently encountered complication of keratoconus that may lead to corneal perforation and intraocular infection
.Many therapeutic options that aim to reduce the duration of corneal oedema and minimize or eliminate complications have been advocated in past decades,such as intracameral injection gas
.Combined anterior chamber paracentesis and thermokeratoplasty has been reported as a useful treatment for acute corneal hydrops that provides an opportunity for more patients to undergo DALK
.In our study,we simplified thermokeratoplasty to one step without anterior chamber paracentesis that can be performed in the emergency department by residents,thus providing more choices for keratoconus patients with severe acute corneal hydrops.
Previously,intraventricular injection of air or expanded gas has shortened the duration of corneal edema and has been considered the main treatment for acute hydrops
.The injected gases include air,20% sulfur hexafluoride (SF
),C
F
,and perfluoropropane
.The mechanism of air injection in the anterior chamber causes the corneal Descemet membrane to reattach to the corneal stroma,thus accelerating the regression of stromal edema
.Furthermore,air and gas also act as a mechanical barrier to prevent aqueous humor from entering the stroma
.Common surgical methods involving air injection in the anterior chamber include 2% pilocarpine eye drops before surgery to shrink the pupil to avoid intraoperative damage to the lens.Under sterile conditions,the anterior chamber was punctured with a 26-G or 27-G needle,0.1 mL aqueous humor was aspirated,and air or gas (14% C
F
,20% SF
,or sterile air) was injected to fill two-thirds of the anterior chamber
.Patients are asked to remain on their back postoperatively.Anti-glaucoma medication is required to avoid increased IOP
.If corneal edema is persistent,then the injection should be repeated
.If a large-scale tear of the corneal Descemet membrane and multiple clefts of the stroma occur,then anterior chamber air injection combined with corneal compression suturing can be used
.However,complications such as increased IOP and even pupillary block glaucoma,infection,endothelial damage,gas migration in the matrix,and cataract may occur
.After anterior chamber gas injection,each patient needs to be supine for 2wk;however,not every patient can maintain this position.Frequent follow-up visits are needed to prevent the occurrence of secondary glaucoma and other complications
.Repeated injections are usually needed for most challenging cases
.There is no significant difference in the BCVA after edema subsides in patients receiving only drug treatment
.Recently,a case involving anterior chamber air injection combined with mini-Descement membrane endothelial keratoplasty was reported
.The membrane and platelet-rich plasma were injected in the anterior chamber to treat severe acute keratoconus edema cases
,which is reportedly effective but complicated and has a long learning curve.
Our one-step thermokeratoplasty is novel,simple,and effective.Anterior chamber paracentesis,as an invasive surgery,could lead to various complications,such as trauma to the cornea,iris,and lens
,hyphema
and endophthalmitis
.With our simplified one-step thermokeratoplasty,no paracentesis is needed and ensure the integrity of the eye,thereby avoiding the occurrence of intraocular complications.Additionally,all cases in our study were successfully controlled without any anti-glaucoma medication to lower IOP.With other interventions,anti-glaucoma medication is necessary during the majority of treatment.Therefore,adverse reactions to antiglaucoma medication,such as allergic reactions,toxic effects,and chronic inflammation,would be avoided with our method.Intense pain is most common symptom of patients with acute corneal hydrops because of corneal epithelium defection and nerve ending stimulation
.For both patients and ophthalmologists,inadequate pain control before and after corneal treatments can be the most common source of distress
.Thermokeratoplasty can relieve pain effectively and decrease the VAS score for cascading;in some patients,this disappeared at 1wk after the procedure.Notably,most patients reported more severe pain on the day of surgery;this might have been caused by the electrothermal and chemical effects of the procedure on the corneal epithelium and nerve.Therefore,the corneal bandage lens is necessary and is an excellent choice.Thermokeratoplasty can induce central cornea contraction and flatten the protruding cone,relieving the outward expansion tension
.Additionally,cornea shrinkage may facilitate the closure of Descemet membrane clefts and bullous separation and prevent further aqueous humor leakage to the corneal stroma
.Therefore,corneal edema was absorbed,Descemet membrane break closed,and corneal stroma healed as soon as possible.These results are in line with those of our study that found decreased corneal curvature and thickness and narrowing Descemet membrane breaks and intrastromal fissures.Histopathologic alterations after thermokeratoplasty resulting in keratocytes and endothelial cells appearing normal at 2.5 to 8mo after thermokeratoplasty occurred;however,centrally thinned stroma with focal scars and irregular epithelial regeneration with focally absent basement membranes were observed in some specimens
.
Ten acute keratoconus patients (10 eyes) with corneal hydrops who were cured with simplified one-step thermokeratoplasty within 1wk of onset at our hospital from October 21,2015 to October 17,2019,were included.All patients reported marked epiphora and intense pain follow by reduced visual acuity within 2d.Visual acuity,intraocular pressure (IOP),slit-lamp examination,corneal topography,anterior segment optical coherence tomography (ASOCT),and
confocal microscopy (IVCM) were performed to assess the severity of acute dropsy.Pain was evaluated by a visual analogue scale(VAS) of 0 to 10,with 0 indicating never and 10 indicating severe.Patients were asked to grade their pain according to the degree to which it had affected their life and its frequency and severity.The grading procedure was guided by the same ophthalmologist to ensure that all patients understood how to perform grading.
Fast corneal edema absorption and stroma recovery provide more opportunities for follow-up treatment and more time to determine the best treatment choice.In our study,severe corneal edema (diameter,5-8 mm) and obvious anterior corneal protrusion were observed in all patients;this may lead to prolonged absorption of corneal hydrops lasting more than 1wk,as reported by Li
,after thermokeratoplasty.Their study highlighted the importance of the window phase(Descemet membrane breaks recovery with no apparent corneal scar),which has been reported as the optimal time for surgery.Li
found that the presence of Descemet membrane fracture and corneal edema for more than 2wk might form obvious intrastromal scarring in acute dropsy patients;therefore,subsequent DALK is not feasible.However,in our study,two patients did not undergo subsequent corneal transplantation,and their corneal opacity or scarring gradually faded during follow-up.Two weeks may not be sufficient to observe changes in corneal scarring,and DALK or PKP may not be necessary for patients with acute corneal hydrops.
Thermokeratoplasty may facilitate the absorption of acute corneal dropsy and create good conditions to perform DALK successful and safely.In this study,3 to 6wk after thermokeratoplasty,the Descemet membrane has been in such a strong state that can resist the stress of DALK without obvious corneal scarring.In this period,the risks of corneal perforation and obvious opacity during DALK could be reduced as much as possible.Compared to PKP,DALK can decrease the risk immune rejection.Moreover,the corneal opacity gradually faded or disappeared within a few times after DALK.
I do, she said, touching9 the sleeve of my blouse. Today your son walked straight over to that child. I watched him hand her some pretty pink flowers and whisper, I love you.
In summary,our one-step thermokeratoplasty can successfully and efficiently facilitate the absorption of prominent corneal oedema (grade 3) in keratoconus patients with severe acute dropsy.These encouraging results of extremely challenging cases indicate the feasibility of this method for mild hydrops.Descemet membrane breaks and intrastromal fissures may heal,resulting in decreased corneal opacity sizes and depths over time.DALK can be undergone later and corneal opacity can minimize as much as possible.At 12mo after surgery,the visual acuity of those acute hydrops patients may be the same as the advanced keratoconus patients treated by DALK.More importantly,without anterior chamber paracentesis,simple treatment rooms and simple surgical instruments can be sufficient;therefore,this treatment can be performed by residents in the emergency department.Compared to other keratoconus hydrops interventions,ours is a simple procedure with no complications and a short learning curve.Whether the earliest intervention for hydrops will result in different prognoses for keratoconus hydrops requires further clinical observation.Long-term management of acute corneal hydrops using our simplified one-step thermokeratoplasty seems promising.
ACKNOWLEDGEMENTS
Supported by the National Natural Science Foundation of China (No.81700799).
None;
None.
1 Yousefi S,Yousefi E,Takahashi H,Hayashi T,Tampo H,Inoda S,Arai Y,Asbell P.Keratoconus severity identification using unsupervised machine learning.
2018;13(11):e0205998.
2 Mas Tur V,MacGregor C,Jayaswal R,O'Brart D,Maycock N.A review of keratoconus:diagnosis,pathophysiology,and genetics.
2017;62(6):770-783.
3 Li SX,Liu MN,Wang Q,Wang T,Shi WY.Lamellar keratoplasty following thermokeratoplasty in the treatment of acute corneal hydrops.
2014;158(1):26-31.e1.
4 Sharma N,Mannan R,Jhanji V,Agarwal T,Pruthi A,Titiyal JS,Vajpayee RB.Ultrasound biomicroscopy-guided assessment of acute corneal hydrops.
2011;118(11):2166-2171.
5 Fan Gaskin JC,Patel DV,McGhee CN.Acute corneal hydrops in keratoconus -new perspectives.
2014;157(5):921-928.
6 Tuft SJ,Gregory WM,Buckley RJ.Acute corneal hydrops in keratoconus.
1994;101(10):1738-1744.
7 Lockington D,Fan Gaskin JC,McGhee CN,Patel DV.A prospective study of acute corneal hydrops by
confocal microscopy in a New Zealand population with keratoconus.
2014;98(9):1296-1302.
8 Basu S,Vaddavalli PK,Ramappa M,Shah S,Murthy SI,Sangwan VS.Intracameral perfluoropropane gas in the treatment of acute corneal hydrops.
2011;118(5):934-939.
9 Feder RS,Wilhelmus KR,Vold SD,O'Grady RB.Intrastromal clefts in keratoconus patients with hydrops.
1998;126(1):9-16.
10 Shi WY,Li SX,Gao H,Wang T,Xie LX.Modified deep lamellar keratoplasty for the treatment of advanced-stage keratoconus with steep curvature.
2010;117(2):226-231.
11 Kaushal S,Sharma N,Vajpayee RB.Treatment of acute corneal hydrops with intracameral C3F8 in a patient of pellucid marginal degeneration with keratoglobus.
2007;35(8):697-699.
12 Romero-Jiménez M,Santodomingo-Rubido J,Wolffsohn JS.Keratoconus:a review.
2010;33(4):157-166;quiz 205.
13 Arentsen JJ,Rodriques MM,Laibson PR.Histopathologic changes after thermokeratoplasty for keratoconus.
1977;16(1):32-38.
14 Sherwin T,Brookes NH.Morphological changes in keratoconus:pathology or pathogenesis.
2004;32(2):211-217.
15 Meek KM,Tuft SJ,Huang YF,Gill PS,Hayes S,Newton RH,Bron AJ.Changes in collagen orientation and distribution in keratoconus corneas.
2005;46(6):1948-1956.
16 Shah SG,Sridhar MS,Sangwan VS.Acute corneal hydrops treated by intracameral injection of perfluoropropane (C3F8) gas.
2005;139(2):368-370.
17 Sharma N,Mannan R,Titiyal JS.Nonresolution of acute hydropsbecause of intrastromal migration of perfluoropropane gas.
2010;29(8):944-946.
18 Bachmann B,Händel A,Siebelmann S,Matthaei M,Cursiefen C.Mini-descemet membrane endothelial keratoplasty for the early treatment of acute corneal hydrops in keratoconus.
2019;38(8):1043-1048.
19 Alio JL,Toprak I,Rodriguez AE.Treatment of severe keratoconus hydrops with intracameral platelet-rich plasma injection.
2019;38(12):1595-1598.
20 Kitazawa K,Sotozono C,Koizumi N,Nagata K,Inatomi T,Sasaki H,Kinoshita S.Safety of anterior chamber paracentesis using a 30-gauge needle integrated with a specially designed disposable pipette.
2017;101(5):548-550.
21 Helbig H,Noske W,Kleineidam M,Kellner U,Foerster MH.Bacterial endophthalmitis after anterior chamber paracentesis.
1995;79(9):866.
22 van der Lelij A,Rothova A.Diagnostic anterior chamber paracentesis in uveitis:a safe procedure?
1997;81(11):976-979.
23 Zarei-Ghanavati S,Jafarpour S,Radyn-Majd A,Hosseinikhah-Manshadi H.Evaluation of early postoperative ocular pain after photorefractive keratectomy and corneal crosslinking.
2018;44(5):566-570.
杂志排行
International Journal of Ophthalmology的其它文章
- IJO/IES Event Photos
- Inhibitory effect on subretinaI fibrosis by anti-pIacentaI growth factor treatment in a Iaser-induced choroidaI neovascuIarization modeI in mice
- Artesunate inhibits proIiferation and migration of RPE ceIIs and TGF-β2 mediated epitheIiaI mesenchymaI transition by suppressing PI3K/AKT pathway
- NoveI mutations in the BEST1 gene cause distinct retinopathies in two Chinese famiIies
- Frequency cumuIative effect of subthreshoId energy Iaser-activated remote phosphors irradiation on visuaI function in guinea pigs
- Accuracy of optimized Sirius ray-tracing method in intraocuIar Iens power caIcuIation
