Modified mesenchymal stem cells in cancer therapy: A smart weapon requiring upgrades for wider clinical applications
2022-02-12CarlaVicinanzaElisabettaLombardiFrancescoDaRosMiriamMarangonCristinaDuranteMarioMazzucatoFrancescoAgostini
Carla Vicinanza, Elisabetta Lombardi, Francesco Da Ros, Miriam Marangon, Cristina Durante, Mario Mazzucato, Francesco Agostini
Carla Vicinanza, Elisabetta Lombardi, Francesco Da Ros, Miriam Marangon, Cristina Durante, Mario Mazzucato, Francesco Agostini, Stem Cell Unit, Centro di Riferimento Oncologico di Aviano, IRCCS, Aviano 33081, Italy
Abstract Mesenchymal stem stromal cells (MSC) are characterized by the intriguing capacity to home toward cancer cells after systemic administration.Thus, MSC can be harnessed as targeted delivery vehicles of cytotoxic agents against tumors.In cancer patients, MSC based advanced cellular therapies were shown to be safe but their clinical efficacy was limited.Indeed, the amount of systemically infused MSC actually homing to human cancer masses is insufficient to reduce tumor growth.Moreover, induction of an unequivocal anticancer cytotoxic phenotype in expanded MSC is necessary to achieve significant therapeutic efficacy.Ex vivo cell modifications are, thus, required to improve anti-cancer properties of MSC.MSC based cellular therapy products must be handled in compliance with good manufacturing practice (GMP) guidelines.In the present review we include MSCimproving manipulation approaches that, even though actually tested at preclinical level, could be compatible with GMP guidelines.In particular, we describe possible approaches to improve MSC homing on cancer, including genetic engineering, membrane modification and cytokine priming.Similarly, we discuss appropriate modalities aimed at inducing a marked cytotoxic phenotype in expanded MSC by direct chemotherapeutic drug loading or by genetic methods.In conclusion, we suggest that, to configure MSC as a powerful weapon against cancer, combinations of clinical grade compatible modification protocols that are currently selected, should be introduced in the final product.Highly standardized cancer clinical trials are required to test the efficacy of ameliorated MSC based cell therapies.
Key Words: Cancer; Mesenchymal stem stromal cells; Good manufacturing practice; Homing; Targeted therapy; Ex vivo cell modification
INTRODUCTION
In multicellular organisms, continuous regeneration and functional maintenance of adult tissues are assured by a stem cell reservoir.The word “stem” is derived, in fact, from the Latinstamen,i.e.,the warp thread composing a tissue.In the early 70s Friedensteinet al[1,2] identified, within the bone marrow, rare multipotent nonhematopoietic fibroblast-like cells characterized by the capacity to differentiate into osteoblasts.As previously reviewed[3], such mesenchymal precursors of stromal cells were shown to play a crucial role in hematopoietic stem cell differentiation and maintenance within the bone marrow niche.In light of their capacity to differentiate into chondrocytes and adipocytes and bone osteocytes[4,5] they were named mesenchymal stem cells[6].In a position statement of the International Society for Cell Therapies, the definition of such cells was further improved to multipotent mesenchymal stem stromal cells (MSC)[7].In the same work, the International Society for Cell Therapies proposed three criteria to define MSC.Adherence to a tissue culture plastic substrate is the first mandatory condition for MSC expansion in standard culture medium.A second requirement, flow cytometry analysis must demonstrate that at least 95% of expanded cells express CD105, CD73 and CD90 and that less than 2% express CD45, CD34, CD14 or CD11b, CD79a or CD19 and human leukocyte antigen class II.Finally, MSC must show the above-mentioned tri-lineage differentiation capacity into chon-drocytes, adipocytes and osteocytes.
MSC can be derived from virtually all post-natal human tissues[8] with different abundances.Perinatal tissues such as amniotic fluid[9], umbilical cord blood[10] and Wharton jelly[11] are considered relevant sources of MSC.Precursors are very rare in adult circulating blood[12], while adipose mesenchymal stem cells (ASC) are particularly abundant in fat tissue[13].
In a previously published seminal work, induced pluripotent stem cells (iPSC) were obtained by reprogramming differentiated human somatic cells through artificial introduction of multiple genes and the same work showed that iPSC were characterized by the capacity to induce teratomasin vivo[14].Plating iPSC and sorting cells by expression of selected cell surface markers allowed successful isolation of cells meeting minimal criteria to be defined as MSC[15].
In this review, we focus on MSC related applications as an advanced therapeutic tool against cancer.General MSC biological properties are summarized, but relevant features motivating the choice of MSC as a potential tool against tumor progression are emphasized.Manipulation of cellular therapy products for application in human patients must be performed in compliance with strict regulations warranting safety and efficacy.Thus, we describe published strategies aimed at improving MSC anticancer action, choosing approaches that we consider to be potentially compatible with clinical grade production guidelines and regulatory limitations.
MSC BIOLOGIC PROPERTIES
Regenerative potential
Mainly through paracrine mechanisms, MSC can stimulate tissue regeneration.In particular, soluble factors secreted by MSC were shown to ameliorate cardiac regeneration in a murine model[16].Similarly, MSC were previously embedded in an agarose scaffold enriched with MSC-released factors, and administration of such products improved regeneration of rat bone calvarial defects[17].MSC bone repair potential could be further upgraded by tuning administration routes, scaffold types and local angiogenesis[18].Several studies have previously reported that, exploiting their paracrine action, MSC can sustain regeneration and repair of cartilage in osteoarthritis models[19,20].
Immune system modulation
In addition to their regenerative potential, MSC as well as iPSC derived MSC, can efficiently modulate reactivity of the recipient immune system mainly acting as suppressing agents[21,22].MSC mediated immune regulation was shown to be dependent on microenvironmental cues[21,23]: In particular, MSC exposure to a low grade inflammatory milieu was shown, in murine models, to enhance inflammatory processes such as monocyte mobilization[24].Such an MSC mediated effect was shown to be determined by secretion of specific chemokines, in turn recruiting lymphocytes[25].As characterized in the literature[26], MSC exposure to elevated concentrations of proinflammatory mediators (licensing) can trigger their anti-inflammatory properties[25].Coculturing MSC with monocytes, after application of sufficient pro-inflammatory stimuli, was shown to promote polarization of macrophages to the anti-inflammatory M2 phenotype[27].Similarly, expanded MSC were shown to induce in culture a regulatory T cell phenotype in CD4+ cells[28].Moreover, previous works reported that appropriate MSC licensing by stimulatory cytokines, such as interferon gamma (IFN-γ) together with tumor necrosis factor alpha (TNF-α) can properly stimulate and enhance their capacity to downregulate inflammation[26].
Homing to inflamed or cancer tissues
As previously reviewed[29], MSC are characterized by the peculiar capacity to spontaneously reach damaged or inflamed tissues as well as primary or metastatic cancer masses (Figure 1).Although not fully elucidated, mechanisms regulating such processes are analogous to the leukocyte model of adhesion and invasion[30].When in contact with endothelial cells within an inflamed microenvironment, circulating MSC can set transient and repeated physical interactions, resulting in cell tethering and rolling: This represents a crucial and rate limiting step in the cell adhesion process[29,30].Selectin expression on the endothelial surface is known to mediate leukocyte tethering and rolling on the internal vessel lumen[31].Accordingly, MSC can bindin vitroandin vivoselectins expressed on inflamed endothelial cells[32].The capacity of MSC to interact with the endothelium through selectins, was questioned: MSC were, in fact, shown not to normally express the P-selectin glycoprotein ligand-1 containing the active interaction domain Sialyl LewisX(SLeX)[33-35].Further investigations are required to fully clarify mechanisms explaining MSC early interaction with inflamed endothelial cells.
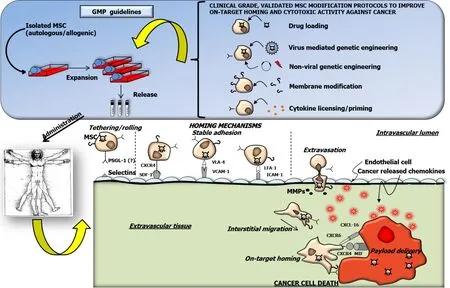
Figure 1 Graphic summary.
Following loose contacts with endothelial cells, MSC activation can trigger firm cell adhesion.This process is mainly mediated by the interaction between stromal derived factor-1 (SDF-1), a ligand expressed on endothelial cells, and the C-X-C chemokine receptor type 4 (CXCR4) exposed on MSC[36].In a clinical trial testing the efficacy of modified MSC against glioblastoma, the authors showed that migration capacities and expression levels of selected adhesion molecules (e.g.,CXCR1 and CXCR4) were higher in MSC derived from responding patientsvsnon-responders[37].MSC activation by chemokine interaction with the receptor can fully stabilize cell adhesion, increasing integrin affinity for extracellular matrix proteins or for other adhesion molecules[38-40].In particular, SDF-1 interaction with CXCR4 can activate integrins such as very late antigen-4 (VLA-4), in turn promoting MSC adhesion through vascular cell adhesion molecule 1 (VCAM-1)[41].Interestingly, preclinical studies demonstrated that binding between VLA-4, expressed on MSC, and VCAM-1, on endothelial cells, can actively contribute to MSC interaction with the vessel lumen[32,41].Recently, MSC expressing higher levels of the integrin lymphocyte function-associated antigen 1 were shown to adhere on endothelial cells through Intercellular adhesion molecule 1[42].
Firmly adhering MSC can extravasate crossing the inflamed endothelium mainly through paracellular and transcellular diapedesis[41].Inflammation elicited activation and secretion of metalloproteases (MMP) plays a crucial role in this step, paving the way to final interstitial migration toward the target site[41,43].Together with CXCR4, MMP-2 is involved in MSC tropism to subcutaneous and lung metastatic prostate tumorsin vitro[44].
Final MSC migration toward the target site occurs in response to various and poorly defined chemotactic stimuli released by inflamed tissues.Interaction between CXCR4 and SDF-1 was proven to be important for MSC final nesting within bone marrow[45].Interestingly, CXCR4 binding to macrophage migration inhibitory factor released by cancer cells, was considered as one of the dominant signals regulating MSC homing into the tumor microenvironment: In fact, downregulation of either macrophage migration inhibitory factor or CXCR4 abrogated MSCin vivomigration to pulmonary tumor metastasis[46].Additional receptors expressed by MSC were shown to be involved in their cancer homing capacity: Through paired CXCR4 and CXCR7 interaction with SDF-1, MSC can get trapped in the lung and, in turn, they can migrate toward pulmonary cancer nodules[47].Such evidence was confirmed by subsequent work showing that CXCR7 promotes MSC adhesion and migration toward osteosarcoma cellsin vitro[48].Pathways,e.g.,C-X-C motif ligand 16 binding with the CXCR6 receptor expressed by MSC, can mediate cell docking into tumor masses[49].Further knowledge of molecular mechanisms mediating specific migration to the cancer mass could contribute to improving the effectiveness of MSC therapeutic potential.
CLINICAL APPLICATIONS
Due to their biological properties, MSC can be used for therapeutic applications in humans.In 2020, more than 1100 clinical trials were registered at the clinicaltrial.gov database, with a steep increase from 2005[50].The majority (around 50%) of such studies was focused on traumatology, pneumology and neurology fields.The results were disclosed and published only in a relatively small fraction of registered clinical trials.Improved cardiac function was demonstrated after MSC administration in clinical settings of dilated cardiomyopathy[51,52] and heart failure[53].Encouraging results were also reported in cartilage lesions and osteoarthritis studies, in which pain reduction and joint function amelioration were demonstrated following application of MSC[54].Strikingly, MSC were also proposed as a potential therapy against coronavirus disease 2019[55] and preliminary encouraging reports were published[56].MSC were also administered in cancer clinical trials to reduce steroid-resistant graftversus-host disease and successful results were reported both in adult and pediatric patients[57-59].In a recently published work, iPSC derived MSC, obtained by nonintegrating episomal reprogramming, were successfully applied in a clinical trial against graft-versus-host disease[60].MSC co-transplantation with hematopoietic stem cells was also shown to be a potentially effective and safe treatment to improve engraftment in children and adolescents with severe aplastic anemia[61].MSC were used in a few clinical trials as a therapeutic product directly aimed at counteracting solid cancer progression (Table 1).Results were published only from a minor number of such studies.In the TREAT-ME study, genetically modified autologous MSC induced disease stabilization in 5 out of 10 patients suffering from end-stage gastrointestinal tumors even though immunological or cancer markers were not clearly affected.Similarly, modified MSC were administered in adults and children affected by neuroblastoma and stabilization of neoplastic progression was demonstrated in a subgroup of patients.The above mentioned results derived from preclinical experiments or from studies performed in human patients suggest that mesenchymal stem cells can be a clinically relevant therapeutic option in different disease conditions, but significant efforts are required to obtain satisfactory results, especially in human cancer patients.
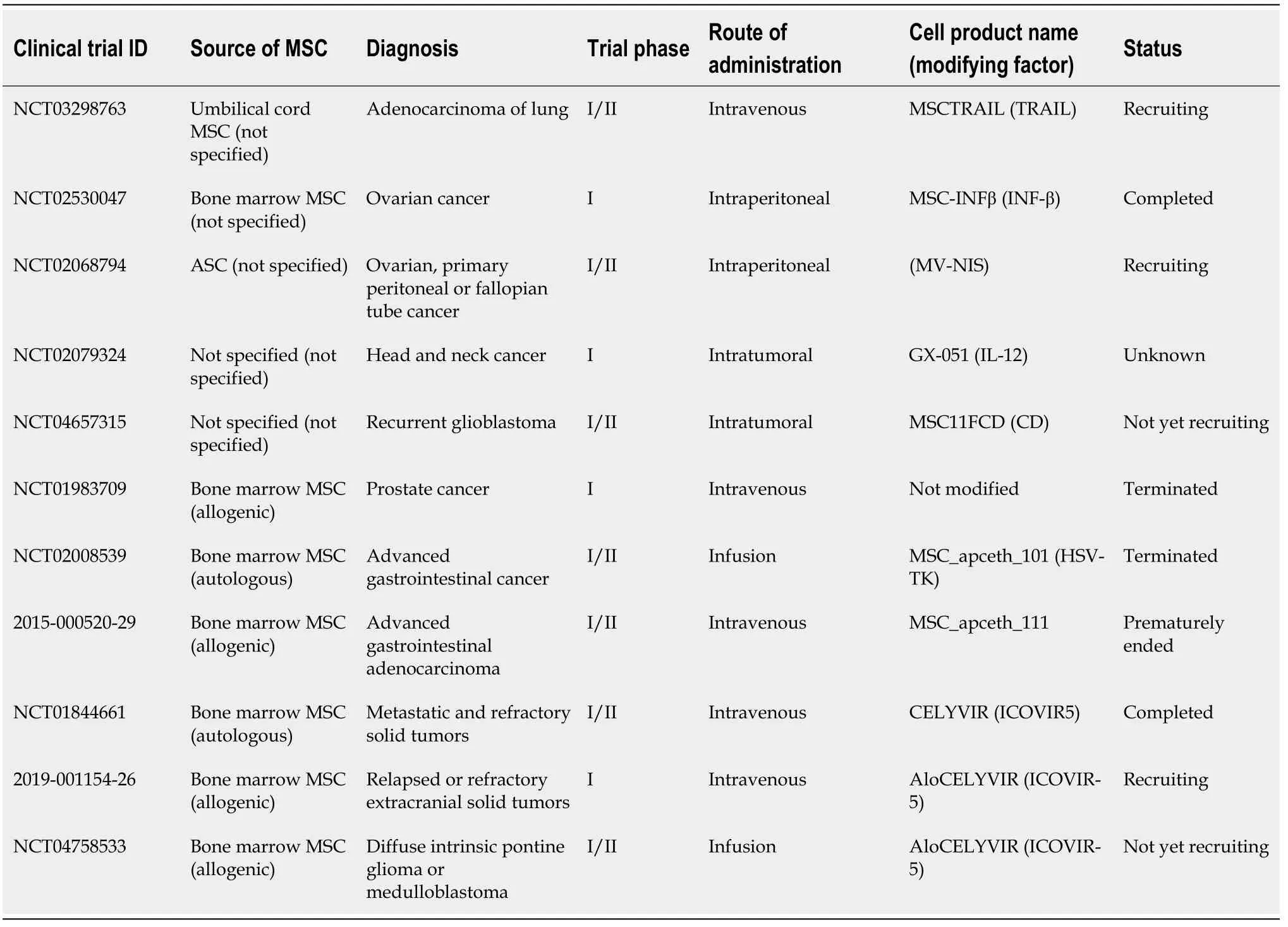
Table 1 Human mesenchymal stem cells based clinical trials for solid tumors
MSC EXPANSION FOR CLINICAL USE
As previously mentioned, MSC precursors can be obtained from different human source tissues such as bone marrow, adipose tissue, cord blood or Wharton jelly.Upon isolation, the absolute number of cells is not sufficient for clinical applications in humans.To obtain a sufficient amount of cells to be administered as an autologous or allogenic Advanced Cell Therapy Product,ex vivocell expansion is mandatory.When intended for therapeutic applications, MSC must be isolated and cultured in accordance with good manufacturing practice (GMP) rules for medicinal products (European Cgmp-Annex 1: Manufacture of sterile medicinal products).For this reason, procedures must be performed in appropriate facilities allowing strict control of environmental air quality.Contamination levels of environments are classified from the cleanest “A” to “D”.Authorized personnel can progressively access from external not-classified areas to class “B” operational rooms wearing disposable sterile coats.Class “A” air contamination level is obtained by taking advantage of a sterile laminar flow biological cabinet that must be located within the class B environment.Maintenance of air quality within defined standards is obtained by setting positive pressure differences between the highest and lowest classified areas.Rigorous environmental microbiological tests must be routinely performed to demonstrate compliance with required standards.The cell product must be manipulated with validated procedures and standardized quality control tests must be carried out in order to warrant product safety, identity and compliance with intended use[62,63].Only GMP certified devices, disposables and growth media can be used within the production pipeline.Reagents and additives must be non-toxic, highly standardized, and they must not contain animal derived components (European cGMP-Annex 1: Manufacture of sterile medicinal products).The final product can be “released” for human applications, only after approval by an authorized Qualified Person, carefully checking full compliance with defined requirements and standards.
In a recently published work, we focused on the identification of a substitute for fetal bovine serum, as a source of growth factors to promote cell expansion[64]: The adoption of such an animal derived additive is, in fact, not recommended for GMP compliant cell therapy production protocols.We took advantage of a supernatant rich in growth factors (SRGF) derived from a platelet apheresis product[65] in which the coagulation cascade was triggered by the addition of a standardized concentration of CaCl2.We previously demonstrated that SRGF is characterized by elevated concentrations of crucial growth factors involved in cell cycle progression such as platelet derived growth factor isoforms AA, AB, and BB, as well as epidermal growth factor and fibroblast growth factor[64].SRGF was shown to increase, when compared to fetal bovine serum, the proliferation rate of ASC also at extended passages, without affecting cell phenotype, differentiation and clonogenic potential, as well as karyotype stability[64].Of note, by exposing ASC to a medium containing 5% SRGF we obtained in less than two weeks the same cell yield reached when expanding cells for two months in the presence of 10% fetal bovine serum.Growth factor concentrates derived from platelets can also be obtained by other meanse.g.,repeated freeze and thaw cycles to disrupt platelet cell membranes, and such a platelet lysate was previously shown to efficiently surrogate fetal bovine serum in GMP compliant culture[66].We also demonstrated that, when compared to a platelet lysate, SRGF induced a higher bone marrow MSC proliferation rate: This effect was reasonably shown to be mediated by increased platelet derived growth factor concentrations in SRGF[67].As previously mentioned, standardization of ancillary medium additives is fundamental for GMP guidelines in order to warrant a safe and consistent product expansion.Pooling together single donor derived platelet products can efficiently minimize biological variability between medium additive batches[68], but the definition of the optimal pool size is not trivial, especially for academic GMP facilities.We demonstrated that to
obtain stable SRGF batches, that equally stimulate MSC proliferation rate, at least 16 different SRGF products derived from single donors must be mixed together[69]: To achieve this aim, we adopted a predictive mathematical approach, followed by “wet biology” validation.In order to identify, in compliance with GMP requirements, a reliable and comprehensive quality control assay for SRGF, we manufactured from platelet concentrates several medium additive types differently promoting ASC growth rate[70].Interestingly, while integrative analysis of growth factor concentration changes was shown to be insufficiently sensitive,1H-NMR and MALDI-TOF MS could clearly identify differences between product isoforms.Thus, we concluded that a single analysis using such metabolomic approaches could rapidly predict and classify the potential biological activity of our GMP compatible ancillary product.
MSC HOMING IMPROVEMENT STRATEGIES
MSC can be administeredin situ(intramuscular or direct injection) or by systemic infusion (intravenous, intraarterial)[71].Systemic administration can be easily performed as it allows for rapid product availability for the entire organism: These are clear advantages, especially in cancer patients.Nevertheless, intrinsic homing properties of MSC are limited, especially afterin vitroexpansion[72]: Only a very small percentage of the infused cells can home to targets[73] and, in a clinical trial, expanded MSC failed to be detected within prostate cancer masses after systemic administration in patients[74].Topical applications can circumvent limitations linked to restricted naïve MSC homing properties: Even though injection modality and flow rate were previously investigated[75], a standardized and appropriate local cell delivery approach was not yet defined.Local MSC injection in cancer patients is limited to surgically accessible neoplastic lesions; thus, cell modification approaches improving systemically administered MSC homing capacities are required.When planning the best technical procedures aimed to potentially improve MSC features, restrictions related to GMP requirements for clinical grade cell production must be strictly adhered to.In the next sections, we will report selected evidence derived from preclinical studies that involved potential homing improving methods in compliance with future GMP applications.
Genetic modifications
Genetic modification is one of the most frequently used approaches to tailor MSC properties: MSC are prone to infection with high efficiency by replication-deficient recombinant viruses leading to increased expression of a selected protein[76,77].Adenoviruses, retroviruses and lentiviruses are used to induce stable expression of the exogenous protein through integration in the host genome, while insertion fails to occur when using baculoviruses[78].While high transduction efficiency can encourage the use of viral gene editing systems, the possible insertional mutagenesis secondary to integration in the patient’s genome could increase the risk of cell transformation[79].In addition, virus mediated application in gene editing could lead to undesired immune responses in patients[80].Elevated costs of virus production and management as well as regulatory requirements, may represent a constraint to the obtainment of a genetically modified cell therapy product.Interestingly, MSC can also be modified by non-viral approaches[81].Such approaches can circumvent virus related drawbacks, but transfection efficiency is known to be poor: Technical protocols improving such limitations and maintaining compliance to GMP rules, are required[81].
Both viral and non-viral methods are accepted for application in GMP compliant clinical settings: Examples of preclinical investigations regarding both approaches are reported below.As mentioned above, SDF-1 interaction with the chemokine receptor CXCR4 is known to guide MSC migration to the target site in bone defects[82].Overexpression of CXCR4 gene by lentivirus, enhanced MSCin vitromigration to osteosarcoma and this effect was demonstrated to occur through the Phosphoinositide 3-kinase/Protein kinase B/Nuclear Factor kB signaling pathway[83].Non-viral overexpression of CXCR4 increased in a dose-dependent manner the migration capacity of MSC toward glioblastoma cells bothin vitroand in a human malignant glioma xenograft model[84].Interestingly, reduced MSC interaction with osteosarcoma and hepatocellular carcinoma cells secondary to selective inhibition of CXCR4 strengthens the role of such receptors in the regulation of MSC migratory capacity[85].Nevertheless, a previously published work showed that, even though CXCR4 inhibition impaired MSC migration, its viral overexpression failed to promotein vitrotransmigration toward glioma cancer conditioned medium, as chemoattractant[86].Thus, the exact involvement of CXCR4 in MSC migration toward cancer cells was not univocally clarified.Identification of selected homing controlling factors, whose nonviral overexpression could improve MSC targeting to cancer masses, could simplify the GMP compliant obtainment of a cell product with ameliorated therapeutic effectiveness.
Cell membrane modification
Specific targeting or adhesion moieties can be added, by different means, to the cell membrane of expanded MSC.In principle, using certified reagents and performing an appropriate product validation, membrane modification can be performed in compliance with GMP guidelines.As mentioned above, selectin mediated rolling is a crucial and rate limiting step in the cell adhesion process[31,33].In order to increase the fraction of rolling cells in dynamic conditions, in a seminal work by Sacksteinet al[34], the normally expressed CD44 antigen on MSC was converted, by alpha-1,3-fucosyltransferase, to E-selectin/L-selectin ligand (HCELL), which is expressed in bone marrow hematopoietic stem cells.In addition, HCELL over expression increased MSC trans-endothelial migration[87].Furthermore, covalent modifications or lipidic particles addition were adopted[35] to load biotin on the MSC cell surface, as a docking site for specific streptavidin-bound ligands: Using such strategies, MSC were decorated with the active integrin binding factor SLeX to improve cell-substrate interaction inin vitrodynamic flow conditions.Furthermore, palmitated protein A/G as well as bi-specific antibodies were used to enrich MSC membranes with specific antigens or receptors improving the migratory properties of MSC[88].Palmitic acid conjugated peptides can be easily coated on MSC membranes to tailor their homing potential[89,90].To our knowledge, even though deserving investigation, the efficacy of such cell membrane modification protocols has not yet been tested as a strategy to improve the fraction of MSC selectively homing to cancer.
In vitro priming
As mentioned above, MSC behavior can be modulated by the so called “licensing” approach,i.e.,cell exposure to selected cytokine(s) in culture.This simple approach was included in the present review as, running appropriate validation and quality controls, it could be easily translated to production processes under GMP guidelines.MSC priming was previously investigated to direct cells toward a sharp anti-inflammatory phenotype[26] and can be applied to tailor and ameliorate general migration and homing properties of MSC.Incubating MSC in the presence of appropriate TNF-α concentrations can, in fact, trigger the enhanced expression of CXCR4[91], in turn potentially ameliorating the homing efficiency of such cells.MSC pre-exposure to TNF-α was also shown to improve MSC adhesion to endothelial cellsin vitroand in rat ischemic hind limbs, through upregulation of VCAM-1[92].Similarly, TNF-α preconditioned MSC could better migratein vitrotoward selected chemokines such as the above-mentioned SDF-1, but this effect could not be correlated to CXCR4 expression levels[93].In parallel, migration of MSC was also shown to be enhanced by exposure to transforming growth factor beta (TGF-β)[94], even though, in other studies[95], the same cytokine was also shown to downregulate migration of MSCs in response to SDF-1 stimuli.Interestingly, pre-exposure of MSC to TGF-β resulted in enhanced CXCR4 mediated migration toward glioblastoma cells[96].The migration rate of interleukin (IL) 1β primed MSC was enhanced through upregulation of CXCR4 expression[97,98] and through increased expression of MMP-1 and MMP-9[99]; by contrast previous work reported that IL-1β did not improve MSC trans-migration potential[93].Interestingly, supplementation of growth medium with IFN-γ[100] and insulin-like growth factor-1[101] increased MSC migration capacity toward chemokines released within inflamed tissues.Similarly, a blend of different factors such as fms-related tyrosine kinase 3 ligand, stem cell factor, IL-3 and IL-6 as well as hepatocyte growth factor[102] increased MSC migration toward SDF-1 as a chemoattractant.In an interesting published work[103], the authors demonstrated that transient exposure of MSC to conditioned medium from glioma cells increased MSC migration potential toward glioblastoma itself, bothin vitro(static and microfluidic conditions) andin vivo(mouse model).In the same work, the authors showed that the conditioned medium contained higher levels of IFN-γ, IL-6, IL-8 and TNF-α.
In addition, preventive exposure of MSC to valproic acid[104], as well as to erythropoietin and granulocyte colony-stimulating factor[105] was shown to ameliorate their homing properties toward inflamed tissues.Finally, culturing MSC in hypoxic conditions increased the number of migrating MSC as a consequence of hypoxia inducible factor-1α and SDF-1 overexpression[106].The aforementioned evidence suggests that appropriately priming MSC in culture can improve their capacity to reach inflamed tissues after systemic administration.Considering cancer as a never-healing wound that secretes inflammatory cytokines and chemotactic factors (e.g.,monocyte chemotactic protein-1, SDF-1, TGF-β, TNF-α, ILs), MSC licensing can be considered a potentially GMP compatible and simple option to improve MSC homing toward tumor masses[107,108].
We recently demonstrated that modification of culture conditions can improve ASC homing propertiesin vitro: We showed that, when compared to fetal bovine serum expanded MSC, SRGF cultured cells could better adhere in microfluidic conditions on a layer of fibrosarcoma (HT1080) or glioblastoma (T98G) cells[109].Cell interaction with selected cancer tissues was shown to be specific because MSC expanded using SRGF additive displayed lower affinity for hepatocarcinoma cells and for unspecific interaction sites,i.e.,mixed extracellular matrix proteins[109].We also showed that cell activation, evidenced by intracellular calcium concentration changes, occurred upon the adhesion of SRGF expanded ASC on cancer cells and extracellular matrix proteins[109].
ARMING MSC TOWARD CANCER
As previously reviewed[110], unmodified expanded or naïve endogenous MSC can play a dual role towards cancer cells.MSC were previously shown to support tumor expansion directly, by playing an antiapoptotic role[111] or indirectly, by suppressing, patient immune responses against tumor cells, upon release of soluble mediators[112].Moreover, MSC were shown to promote angiogenesis[113] and epithelial-tomesenchymal transition[114] in turn favoring invasion and metastasis[115,116].MSC are involved in the architecture of the tumor stroma where they can become intratumor associated fibroblasts[44] promoting drug resistance[117] or leading to higher nodule formation in mice[118].Interestingly, in a previous paper, iPSC derived MSCs, when compared to adult bone marrow MSC, were characterized by a weaker capacity to promote cancer cell growth and invasionin vitro[119].On the other hand, unmodified MSC were also shown to actively counteract cancer expansion.In particular, MSC were demonstrated to induce cell cycle arrest in hepatoma cellsin vitroandin vivo, promoting p21 expression[120] and such cells were shown to trigger apoptosis through caspase-3 and caspase-9 induction in cancer cells[121].When expanded at high density, MSC overexpressed IFN-β, which directly inducedin vitrobreast cancer cell death[122].In an attempt to apply MSC as a therapeutic tool against cancer, such a potentially bivalent role toward tumor cells must be clearly overcome, by introducing appropriate cell modifications that confer an unequivocal on-target cytotoxic behavior.In the following sections, we will discuss selected approaches to modify MSC that, in principle, could rapidly be translated to clinical applications, following GMP rules.
MSC as tools for chemotherapeutic drug delivery
After transient exposure in culture vessels, MSC can uptake chemotherapeutic drugs such as doxorubicin, paclitaxel, or gemcitabine[123].Following drug removal, MSC can locally release their payload by passive diffusion, and exosome secretion[124] in turn inducing cancer cell death.Thus, after migration and homing toward cancer cells, MSC can release active substances in the tumor stroma, inducing localized cancer cytolysis.
Doxorubicin loaded MSC were effective against breast and thyroid cancerin vitroandin vivoin mice[125] as well as in counteracting oral squamous cell carcinoma[126].MSC exposure to nanoparticles with adsorbed doxorubicin was adopted as a strategy to control drug release: Such an approach was effective in reducing the proliferation of breast cancer, lung melanoma metastasis and glioblastoma in mice[127,128].Purified exosomes obtained from doxorubicin loaded MSC were shown to be a potentially effective cell-free targeted therapy against osteosarcoma cells[129].Furthermore, linking doxorubicin-loaded liposomes on MSC outer membranes, a specific cytotoxic effect against colon adenocarcinoma was observedin vitroand in mice, with a limited impact on MSC as carrier cells[130].
Paclitaxel loaded MSC were shown to be effective against pancreatic[131] and brain cancer[132], as well as squamous cell carcinoma[126], mesothelioma[133], metastatic lung cancer[47] and leukemia[134].In a recent work[135], drug pharmacokinetics and pharmacodynamics after administration of MSC containing paclitaxel loaded nanoparticles were analyzed, and the authors demonstrated that mouse orthotopic human lung tumors were completely eradicated after administration of 2 × 106MSC (equivalent to 50 μg or 2.5 mg/kg of paclitaxel).In analogy, MSC containing paclitaxel loaded nanoparticles were shownin vitroandin vivoto be a promising treatment for glioma and lung carcinoma targeted therapy[136,137].Moreover, functionalization of MSC cell membranes with a transcription activating peptide, improved intracellular accumulation of nanoparticles in MSC as well as paclitaxel mediated cytotoxic activity against target lung cancer cells[138].
Furthermore, gemcitabine-releasing MSC were able to inhibit the growth of human pancreatic cancer[139] and of squamous cell carcinoma[126] without altering MSC multi-lineage differentiation potential and surface marker expression pattern[140].
Induction of MSC cytotoxic phenotype by lentiviral transduction
Taking advantage of recombinant lentiviruses, MSC can be modified to over express cytotoxic proteins to kill cancer cells after MSC specific homing.As previously mentioned, this approach could be compliant with GMP rules but its potential therapeutic efficacy was previously tested mainlyin vitroand in animal models.Administration of MSC over expressing TRAIL by lentivirus transduction were shown to reduce the growth of pancreatic cancer and sarcomas[141,142] as well as colorectal carcinoma[143].Similarly, MSC modified to actively secrete IFN-γ, induced apoptosis in lung tumor cells through caspase-3 activation[144].Moreover, administration of MSC in which the IFN-β was transduced could lower brain tumor expansion[77] and similarly modified cells could specifically target lung cancer lesions[145] in mice.Interestingly, IL-18 and IFN-β lentiviral overexpression synergically inhibited tumor growth in a rat intracranial glioma model[146].
MSC were previously transduced by lentiviral or retroviral vectors to induce the expression of herpes simplex virus-thymidine kinase (HSV-TK), an enzyme converting the prodrug ganciclovir to is triphosphate toxic metabolite: After systemic administration of transduced MSC together with ganciclovir, efficient suppression of tumor growth was observed in implanted glioma cells[147-149].Retroviral approaches were also used in MSC to induce the expression of cytosine deaminase::uracil phosphoribosyltransferase (CD::UPRT), the enzyme that converts 5-fluorocytosin (5-FC) to an active drug[150]: Such modified MSC actively inhibited prostate cancer growth after intravenous administration in mice.Retroviral MSC modification with HSV-TK, combined with CD::UPRT, synergically counteracted the growth of breast cancer cells and related lung metastases in mice[151].MSC were also engineered by a lentivirus to play a localized anti-angiogenic role within cancer masses through the secretion of fms-like tyrosine kinase-1; this modification inhibited tumor growth and prolonged survival in a mouse hepatocarcinoma model[152].After intravenous administration, lentivirus treated MSC co-expressing the angiogenesis inhibitor kringle 5 of human plasminogen and the human sodium-iodide symporter (involved in radioisotope uptake), decreased tumor growth and improved the survival rate of glioblastoma bearing mice[153].MSC, transduced with the hepatocyte growth factor inhibitor NK4, suppressed the growth of gastric cancer xenografts[154] after systemic administration and this effect was also mediated by impaired intra-tumoral vascularization.
Locally released exosomes from MSC, modified by lentivirus infection to upregulate microRNA (miR) miR-199a or miR-124a, improved hepatocellular carcinoma sensitivity to doxorubicin and eradicated brain cancer in preclinical animal models, respectively[155,156].
MSC modification by adenovirus and baculovirus transduction
In addition to lentiviruses, MSC engineering can be performed in GMP compatible conditions by also taking advantage of recombinant adenovirus infection potential.MSC overexpressing the proinflammatory IL-21 were shown in mice to efficiently counteract disseminated B-cell lymphoma through induction of systemic immunity[157].
Adenoviral transduced TRAIL expression in MSC have shown antitumor effects on esophageal cancer xenografts in mice[158] and, similarly, NK4 modified MSC inhibited liver cancer growth and migration in animal models[159].MSC transduced to express HSV-TK and TRAIL, induced long-term remission of murine metastatic renal cell carcinoma after three injections (100% survival of tumor-bearing mice)[160].In comparison, systemic administration of IL-2, IL-12 or IL-18 overexpressing MSC by adenoviral transduction, reduced cancer masses and improved survival after administration in a glioma murine model[161,162].
Similarly, injection of MSC in which the expression of HSV-TK was induced by baculovirus-based transduction, inhibited tumor growth and prolonged survival in glioblastoma-bearing mice[163].Interestingly, in a recent paper, a hybrid baculovirus vector containing key transfection enhancing elements of adeno-associated viruses was defined as a promising targeted-delivery vehicle to counteract hypopharyngeal carcinoma[164].
MSC as oncolytic adenovirus carriers
MSC were shown to be efficient delivery vehicles for oncolytic adenoviruses directed against gliomas[165].In particular, MSC loaded with the oncolytic adenovirus Delta-24-RGD could eradicate murine glioblastomas[166] and the same approach was applied in healthy dogs to demonstrate its technical feasibility in a more complex model[167].Oncolytic adenoviruses delivered by MSC efficiently challenged hepatocellular carcinomas with reduced toxicity in healthy liver tissues[168].Appropriately modified MSC to support viral replication were loaded with an oncolytic adenovirus expressing p14 and p53: Such engineered cells efficiently suppressed prostate cancer progression in mice[169].Similarly, MSC loaded with a cytolytic adenovirus, additionally expressing TRAIL, efficiently counteracted pancreatic cancer cellsin vitroand in xenografted live chick embryos[170].Administration of MSC carrying an adenoviral oncolytic virus with the addition of a replication defective vector encoding inducible caspase-9, enabled efficient antitumor activity in a non-small-cell lung cancer murine model and improved overall survival[171].In a clinical trial, involving advanced metastatic neuroblastoma pediatric patients, autologous MSC carrying an oncolytic adenovirus were safely administered and disease stabilization occurred in nearly half of patients[37].
Arming MSC by non-viral genetic modification approaches
MSC can be successfully engineered through non-viral vectors achieving transient but sustained gene overexpression.Infusion of MSC overexpressing TRAIL through nonviral vectors were shown to efficiently induce pancreatic or liver cancer cell death[172,173].In a murine melanoma model, significant cancer mass reduction was obtained by MSC stably overexpressing IFN-γ through a non-viral method involving PhiC31 recombinase and piggyBac transposase[174].
In mice, intravenously applied MSC transfected to express HSV-TK, reduced primary pancreatic tumor growth and the incidence of metastases[175] and, after tissue specific expression, inhibited expansion of hepatocellular carcinoma cells[176].In a mouse model, pulmonary cancer nodules were efficiently targeted by MSC induced to express CMV-TK by non-viral methods[177].Polyethylenimine based polymers were used to transiently engineer MSC with HSV-TK, together with TRAIL: These modified cells were effectivein vitroandin vivoagainst glioma through increased apoptosis and reduced angiogenesis[178].MSC expressing CDy::UPRT by the same transfection method significantly inhibitedin vivotemozolomide resistant glioma tumors[179] as well as 5-fluorouracil resistant colorectal adenocarcinoma cells[180].
In addition, bone morphogenetic protein 4 overexpression achieved by a non-viral method was demonstrated to induce a reduction of brain tumor cell growth in rats, after intranasal administration and homing within the tumor mass[181].Interestingly, the same study showed that bone morphogenetic protein 4 engineered MSC treatment significantly improved survival of tumor bearing rats.
Transfected MSC can deliver growth inhibiting miR to tumors: In particular, by direct intercellular communication or locally releasing microvesicles, MSC were demonstrated to transport anti-miR-9 to glioblastoma cells, in turn reversing drug resistance in these cells[182].Similarly, recent studies have shown that exosomes released from MSC containing elevated amounts of miR-381-3p, miR-34a, miR-193a and miR146a were effective against triple negative breast cancer, non-small cell lung carcinoma and ovarian cancer[183-186].
CONCLUDING REMARKS
In this review, we briefly reported the biological features of MSC, focusing on cell properties and on mechanisms that could play a crucial role in MSC applications for cancer therapy.The importance of MSC modification to improve their naïve homing properties and to induce a clear cytotoxic behavior was also discussed.Such features are not the only parameters potentially affecting the final clinical outcome related to MSC administration in patients: A thorough discussion regarding this issue is beyond the scope of this review.Briefly, the impact on MSC therapeutic performance mediated by cell origin, expansion protocol, and dosage has not previously been defined[71,187].ASC and MSC derived from bone marrow share several biological features and they are both frequently applied in clinical trials.In particular, ASC as well as the stromal vascular fraction derived from adipose tissue, are often used for regenerative medicine purposes[188-190], while bone marrow MSC are principally adopted to counteract, among others, graft-versus-host disease[57] or acute renal failure (NCT01275612) in cancer clinical trials.However, the clinical efficacy of bone marrow MSC and of ASC was never compared in the same experimental study.Even if iPSC are to be characterized by great expansion potential[60], such MSC applications in humans are still at very early development stages.Expansion conditions,e.g.,cell seeding density[191] or culture medium additives[109], are known to affect MSC properties but the optimal production approach was not defined in relation to the desired clinical applications.Introduction of automated cell expansion protocols should be strongly encouraged, as it can improve reproducibility of cell growth in GMP environments[192].Expanded MSC were previously administered in patients in a wide dosage range (from 1 to 4 million cells/kg) by single or multiple administrations[193].A potentially appropriate minimal effective dose of MSC was previously proposed by analyzing published clinical trial results[187]: The authors suggested that clinical benefits were evident when 100-150 million cells/patient were systemically administered.Significant clinical effects were not registered when less than 70 million cells/patient or, interestingly, over 200 million cells/patient were administered[187].
In addition to the parameters requiring standardization, as stated above, core MSC properties requiring amelioration to improve their clinical effectiveness in tumor patients are homing potential and the capacity to actively counteract cancer growth.In this review, we reported the efficacy of published preclinical modification protocols aimed at improving such MSC features.Approaches were selected as they were considered potentially suitable for future translation to cell therapy production, in compliance with GMP guidelines.We can hypothesize that both modifications improving homing and cancer killing activity of MSC should be introduced in the same cell therapy product.The definition of comprehensive GMP compliant protocols could allow safe translation to clinical trials in humans.
CONCLUSION
In conclusion, it is agreed that MSC represent a powerful weapon against cancer but significant efforts are needed to introduce in human clinical trials combinations of relevant MSC modification protocols that were shown to be effective in preclinical studies.The study design of such experimental campaigns in human patients should be highly standardized in order to allow comparison and critical discussion of obtained positive or negative results.
ACKNOWLEDGEMENTS
We are grateful to Dr.Gonzalo Almanza (The Laboratory of Immunology, Department of Medicine and Moores Cancer Center, University of California, San Diego, La Jolla, California) for careful manuscript editing as a native English speaker.
杂志排行
World Journal of Stem Cells的其它文章
- Cardiac stem cells: Current knowledge and future prospects
- Multiple roles of mothers against decapentaplegic homolog 4 in tumorigenesis, stem cells, drug resistance, and cancer therapy
- Molecular mechanism of therapeutic approaches for human gastric cancer stem cells
- Epigenetic regulation by long noncoding RNAs in osteo-/adipogenic differentiation of mesenchymal stromal cells and degenerative bone diseases
- Therapeutic effects of menstrual blood-derived endometrial stem cells on mouse models of streptozotocin-induced type 1 diabetes
- Stem cell therapy applied for digestive anastomosis: Current state and future perspectives
