Dental mesenchymal stromal/stem cells in different microenvironments— implications in regenerative therapy
2022-01-07IvanaOkioreviHristinaObradoviTamaraKukoljAnelijaPetroviSlavkoMojsiloviDianaBugarskiAleksandraJaukovi
Ivana Okić-Đorđević, Hristina Obradović, Tamara Kukolj, Anđelija Petrović, Slavko Mojsilović, Diana Bugarski,Aleksandra Jauković
Ivana Okić-Đorđević, Hristina Obradović, Tamara Kukolj, Anđelija Petrović, Slavko Mojsilović, Diana Bugarski, Aleksandra Jauković, Laboratory for Experimental Hematology and Stem Cells, Institute for Medical Research, University of Belgrade, Belgrade 11129, Serbia
Abstract Current research data reveal microenvironment as a significant modifier of physical functions, pathologic changes, as well as the therapeutic effects of stem cells.When comparing regeneration potential of various stem cell types used for cytotherapy and tissue engineering, mesenchymal stem cells (MSCs) are currently the most attractive cell source for bone and tooth regeneration due to their differentiation and immunomodulatory potential and lack of ethical issues associated with their use.The microenvironment of donors and recipients selected in cytotherapy plays a crucial role in regenerative potential of transplanted MSCs, indicating interactions of cells with their microenvironment indispensable in MSC-mediated bone and dental regeneration.Since a variety of MSC populations have been procured from different parts of the tooth and tooth-supporting tissues, MSCs of dental origin and their achievements in capacity to reconstitute various dental tissues have gained attention of many research groups over the years.This review discusses recent advances in comparative analyses of dental MSC regeneration potential with regards to their tissue origin and specific microenvironmental conditions, giving additional insight into the current clinical application of these cells.
Key Words: Microenvironment; Dental mesenchymal stem cells; Modulation of regenerative potential; Tissue origin; Hypoxia microenvironment; Inflammatory microenvironment; Clinical application
INTRODUCTION
Bone defects and dental loss connected with either disease or trauma seriously influence the quality of life of the whole population, including emotional, physical, and financial load on the society.For the medical treatment of oral diseases, periodontal treatment, dental implants, and dental protheses are the gold standards[1].Since these oral therapies can only maintain the current state and stop further complications of the disease, failing to influence complete tissue regeneration, new technologies are needed to overcome these limitations at various tissue regeneration steps[2].Currently, tissue engineering represents a promising future approach for recovering the function and integrity of tooth’s hard tissue[3].The microenvironment of dental tissues, containing dental immune cells, blood vessels, extracellular matrix (ECM), numerous secreted soluble mediators, and various stromal cells, essentially influences the healing process of diseased dental tissue[4,5].In terms of regenerative features, mesenchymal stem cells (MSCs) are the most prominent among stromal cells.Their clinical application in the treatment of dental diseases is still at the beginning since the exact mechanism of their therapeutic properties is not yet clear.
MSCs are the population of multipotent stromal cells present in many adults, perinatal and fetal tissues, where they participate in homeostasis maintenance.They were initially isolated from bone marrow and characterized as fibroblast-like cells[6].After a while, their presence has been demonstrated in various fetal and adult tissues, such as peripheral blood, umbilical cord, placenta, adipose tissue, and others[7,8].In the past two decades, a variety of MSC populations have also been procured from different parts of the tooth and tooth-supporting tissues (Figure 1): Dental pulp stem cells (DPSCs), stem cells from human exfoliated deciduous teeth (SHEDs), periodontal ligament stem cells (PDLSCs), dental follicle stem cells (DFSCs), gingival MSCs (GMSCs), and stem cells from the dental apical papilla (SCAPs)[9].These cells are particularly suitable for research, given the easy availability of tissues through noninvasive dental procedures and simple methods for their isolation.According to the International Society for Cellular Therapy, minimal criteria to characterize MSC population consider the positive expression of surface markers CD73, CD90, and CD105 and negative expression of CD11b, CD19, CD79α, CD34, CD31, CD45, and human leukocyte antigen-DR isotype, along with their self-renewal and multilineage differentiation capacity into cells of osteogenic, chondrogenic, and adipogenic lineages[10] (Figure 2).Yet, the defining characteristics of MSCs are inconsistent among researchers.In addition to their regenerative role, MSCs exert immunomodulatory properties by affecting cells of the innate and adaptive immune system through direct intercellular contacts and/or secretion of soluble mediators (Figure 2).Moreover, MSCs express multiple paracrine functions, thus modulating surrounding microenvironment response to numerous autoimmune and inflammatory diseases[11].Previous research has shown that MSCs suppress activation and proliferation of CD4+ helper and CD8+ cytotoxic T lymphocytes, B lymphocytes[12,13], dendritic cells, and natural killer cells[14], while increasing the production of regulatory T-lymphocytes[15].In addition, it has been determined that MSCs modulate microenvironment in the injured tissue by releasing anti-inflammatory and anti-apoptotic molecules[16].
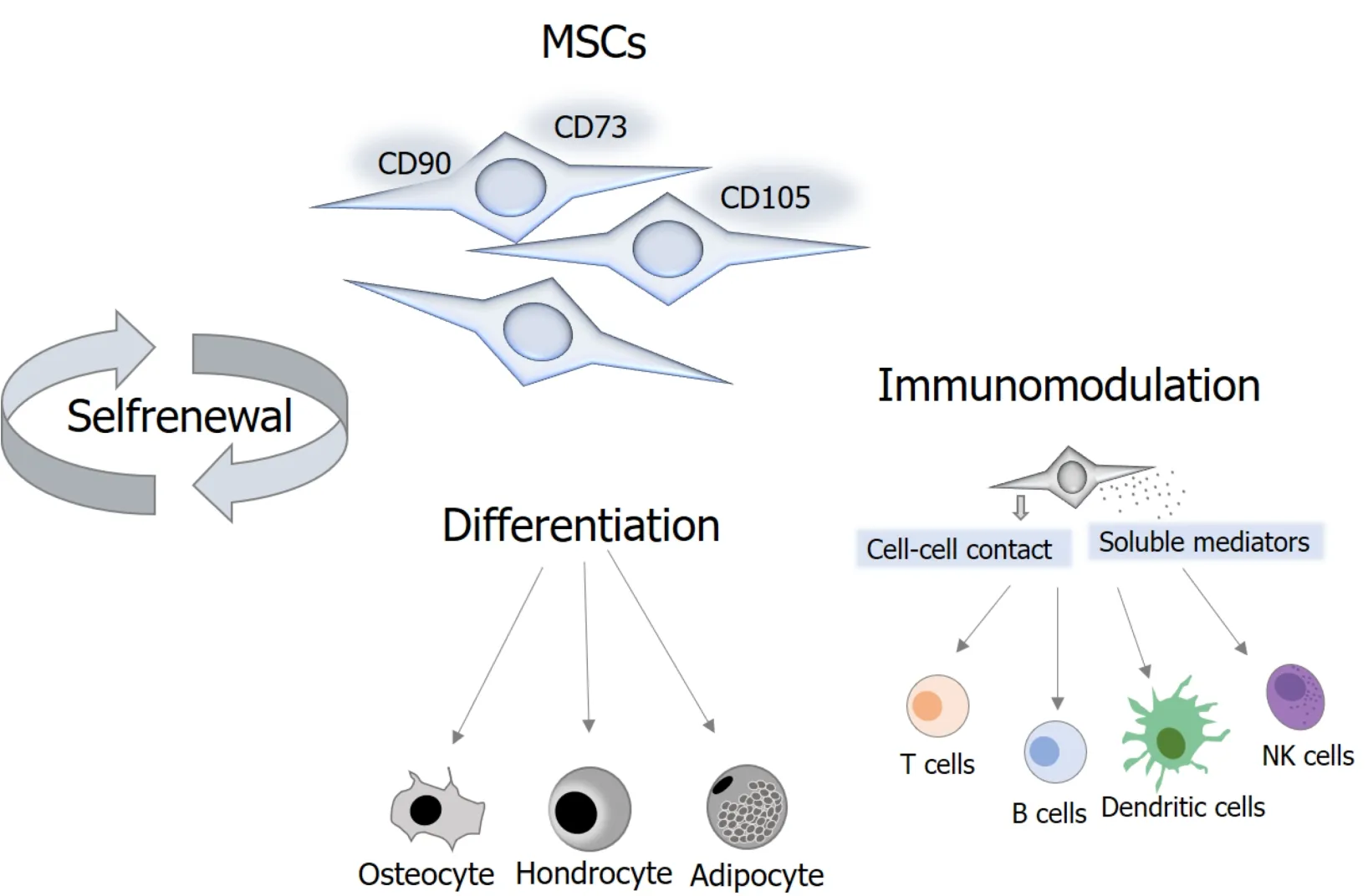
Figure 2 Properties of mesenchymal stem cells.
It is well known that MSCs’ behavior depends on the context of the microenvironment in which they reside and function.These physiologically defined compartments, named stem cell niches, are the sites of external cues integration that determine the fate of MSCs and govern them towards specific functions[17].Therefore, a better understanding of the effects of specific microenvironmental conditions on MSCs’ fate is of great importance for getting a real insight into their biology and optimizing the conditions for their successful use.
Oxygen (O2) represents an important factor in the stem cell niche necessary for cell activity and metabolism.Unlike laboratory standard conditions that correspond to the atmospheric (21%) O2levels, physiological oxygenation in tissues is hypoxic, ranging from 1%-14% with an average of about 5%[18].Response to O2level changes in mammals is mainly regulated by hypoxia-inducible factor 1 (HIF-1)-α, an ubiquitously expressed transcription factor subunit that translocates to the nucleus under hypoxic conditions where it binds to HIF-1β to regulate target genes[19].Different O2levels affect various MSCs features[20,21].Moreover, the hypoxia effects depend on cell type, oxygen concentration, and experimental design; thus, many studies gave contradictory results, especially considering short-term exposure to hypoxia[20].In dental and dental-supporting tissue derived cells, low oxygen levels (1%) increase the formation of reactive oxygen species, leading to oxidative stress, specifically in periodontal ligament (PDL) cells[22].The reactive oxygen species level multiplies when the bacterial inflammation occurs within a hypoxic environment[23].A unique feature of the oral cavity is the presence of plenty of microorganisms such as bacteria, fungi, protozoa, or viruses, organized in the complex communities, termed as oral microbiome.These microorganisms coexist with the host in a symbiotic way.Depending on the mouth area, the microbiome's composition is diverse, with the dental tissues (including teeth and teeth supportive tissues) being the habitat of many microorganisms (dental plaque).As the composition of the oral microbiome changes dynamically[24,25], physiological balance can be disrupted, consequently encouraging the infection development in the host[26,27].
This review provides a detailed summary of currently available data concerning dental MSC regeneration potential in terms of the tissue origin and influence of hypoxic and proinflammatory microenvironments.Furthermore, it analyzes current evidence regarding clinical applicability of dental MSCs.
DENTAL MSCS REGENERATIVE PROPERTIES WITH REGARDS TO THEIR TISSUE ORIGIN
The term dental tissue refers to the tooth and tooth-supporting tissues (periodontium).There are two major constitutive parts of the tooth, a crown (mostly visible part of the tooth) and a root.The crown is formed of three hard tissues, enamel, dentin, and cementum, and one soft tissue, dental pulp[28].Enamel, dentin, and cementum are tissues with limited or no possibility to regenerate[29], while the dental pulp is a loose connective tissue profusely vascularized and innervated.Structurally, dental pulp is divided into three main regions that form a continuum: The peripheral odontoblastic and the sub-odontoblastic layer and the central pulp[30,31].In terms of cellularity, the most common dental pulp cell types are fibroblasts, peripheral odontoblasts, and DPSCs, whereas collagens I and III represent extracellular pulpal matrix key protein components[32].Moreover, the proportion of cellularity to collagen with aging favors collagen[30].
Dental pulp MSCs, with their extensive proliferation and multipotential differentiation capability, have an intrinsic role in dental pulp regeneration potential (Figure 3).They were first discovered by Gronthoset al[33] in 2000 as MSCs derived from the pulp of the permanent, impacted third molars and supernumerary teeth, commonly considered as medical waste.Like other dental MSCs, DPSCs express osteoblastic markers such as alkaline phosphatase (ALP), collagen type I (COL1A1), and osteocalcin (OCN) and are able to differentiate into osteoblast-like cells.Furthermore, DPSCs are essential for postnatal tooth homeostasis through implementation of odontoblasts in the dentin restoration process.When dental injuries or odontoblast apoptosis occur, DPSCs rapidly proliferate, migrate, and differentiate into odontoblast cells.Moreover, being of neural crest origin, DPSCs can differentiate into functionally active neurons and glial cells[34].Importantly, recent studies have revealed that DPSCs reside in neurovascular niche where they secrete an array of angiogenic regulatory factors and generate capillary-like structures demonstrating strong angiogenic ability[35].Overall, neurovascular and MSC-like properties make DPSCs good candidates for bone and tooth regeneration.
Stem cells from the pulp tissue of human exfoliated deciduous teeth (Figure 3), firstly isolated by Miuraet al[36] in 2003, are capable of forming dentin-like structures.Moreover, they show higher proliferative, odontogenic, and osteogenic differentiation potential than DPSCs[37].Furthermore, these cells have a higher doubling time[38] than DPSCs and higher expression of collagens I and III as well as of pluripotency markers such as octamer-binding transcription factor-3/4, sex determining region Ybox-2, and Nanog homeobox[39].SHEDs are also able to differentiate into neural and glial cells under appropriate conditions.Being able to demonstrate regenerative potential even 2 years after cryopreservation[40] and, because of their easy accessibility, SHEDs represent good candidates for bone and tooth regeneration.
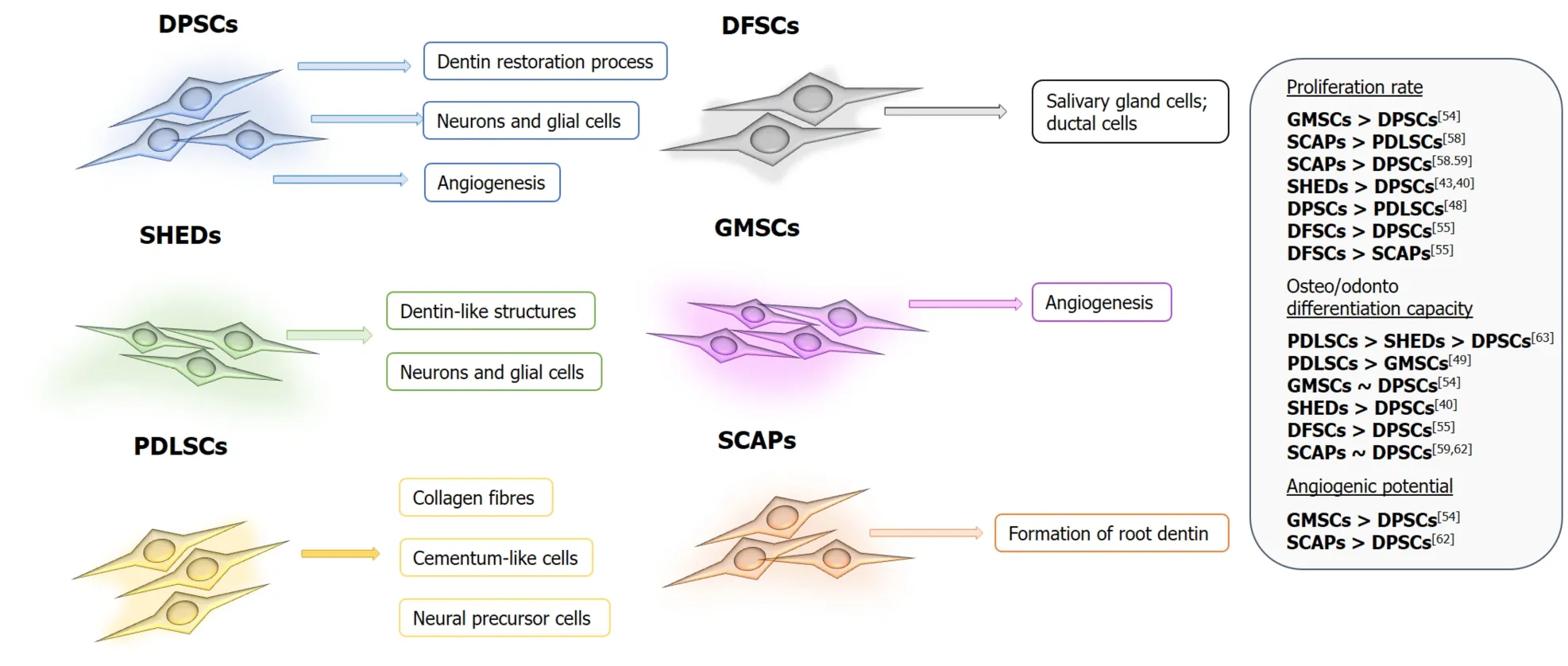
Figure 3 Functional properties and differences among dental mesenchymal stem cells.
However, the possibility of dental pulp tissue regeneration is restricted by several factors.Since dental pulp has collateral blood circulation due to the anatomical organization of the pulp chamber, the efficacy of the immune response to infection is limited[41].Thus, the localization of DPSCs in perivascular and perineural pulp regions and consequent contacts with different microenvironments, along with their high immunomodulatory activity[42], makes them good candidates for modulating the immune response to infection.Furthermore, when comparing cellular density in specific tooth regions of dental pulp tissue from different teeth, higher density was observed in the coronal region of deciduous and premolar teeth compared with supernumerary and third molars.In contrast, a high cell density was observed in the apical region of supernumeraries and premolars compared with third molar teeth[43].Overall, supernumerary dental pulp as source for DPSCs has the best morphometric parameters, and its cell density is comparable to that of deciduous tooth pulp.
Periodontium is a specialized connective tooth-supporting tissue that surrounds the root of the tooth.It has the role of attaching the tooth to the jawbone, amortizing the mechanical pressure that occurs during chewing and speech but also in the formation and resorption of bone tissue.Periodontium involves two soft tissues—PDL and gums, and two hard tissues—alveolar bone and cementum[44].The PDL is a connective tissue with high cellularity and amount of ECM components.As for cellular constituents, PDL consists mainly of fibroblasts, osteoblasts, osteoclasts, cementoblasts, and cementocytes.Other cells present in PDL include epithelial cell rests of Malassez, macrophages, nerve cells, endothelial cells, as well as MSCs.PDLSCs represent a unique population of somatic stem cells of mesenchymal origin with the regenerative potential reflected by self-renewal and multipotent differentiation ability as well as potency for the formation of tissues that support the teeth, including the PDL and cement (Figure 3).On the other hand, the rich ECM of PDL is formed of collagen type I, II, and XII fibers, proteoglycans, and a vast vascular network[45].Interestingly, collagen type I is the most widely used scaffold material for dental pulp regeneration[46], and PDLSCs have shown higher expression ofCOL1A1compared to DPSCs[47].Taken together, these features qualify PDLSCs for use in the regeneration/reconstruction of tooth-supporting tissue in periodontal disease.
Like PDL, the gingival connective tissue also has a rich ECM.Collagen fibers and ground substances make up 60% and 35% of gingival ECM, respectively, and only about 5% of gingival connective tissue consists of various cells like fibroblasts, mast cells, macrophages, and inflammatory cells[48].Structurally and functionally, the gingiva is different from PDL, displaying an even higher collagen turnover rate than PDL and having a distinct composition and organization of ECM.It was noticed that compared to PDL fibroblasts, gingival fibroblasts have a significantly lower level of ALP expression, an increased potential to stimulate epithelial growth, as well as a distinctive property of regulating cytokeratin expression by epithelial cells[49].Furthermore, the gingival tissue is highly vascularized, thanks to the high number of anastomoses[50].Moreover, due to the activities of local microenvironment factors, including transforming growth factor-α, transforming growth factor-β, insulin-like growth factor, nerve growth factor, epidermal growth factor, and fibroblast growth factor, gingiva has a particularly high wound-healing capacity.Other local factors, such as mechanical signals from the ECM to the cells, may be involved as well[49].All of these structural characteristics provide gingival tissue with a great therapeutic potential in regenerative therapy especially in terms of GMSCs.In contrast to MSCs from other sources, GMSCs isolated from the gingival lamina propria are profuse and easily procured cells through minimally invasive cell isolation techniques, which make them suitable cells for regenerative purposes[51].Compared to PDLSCs, GMSCs have a higher rate of proliferation while also exerting a higher capacity to proliferate, migrate, and form angiogenic tubules in comparison to DPSCs (Figure 3)[52].
The alveolar bone is located on the jaw bones that hold the teeth, and it arises in the process of immature tooth root development from the dental follicle (DF), one of the multipotent tissues[53].The DF is made up of MSCs and fibers surrounding the enamel organ and dental papilla of a developing tooth[54].It is a vascular fibrous sac of ectomesenchymal origin.Histologically, DF is characterized by fibrous connective tissue with variable amounts of lining epithelium, including enamel, cuboidal, squamous, and, rarely, respiratory epithelium.The type of lining epithelium seems to be related to the patient’s age[55].DFSCs, originating from this developing tissue, possess higher plasticity than other dental stem cells[56].Recently, isolated DFSCs were also found to have the ability to form salivary gland cells and ductal cells[56] (Figure 3).
Another immature dental tissue is the apical papilla, a tissue only present during root development before the tooth erupts into the oral cavity[57].In comparison to the dental pulp, the apical papilla has less cellular and vascular components[57], and the tissue is more immature since it contains a higher number of MSCs than mature dental pulp tissue.Moreover, the apical papilla performs a key role in the differentiation of odontoblasts into cells capable of secreting the primary dentin matrix[58] .Furthermore, the localization of the apical papilla in the apical root of the tooth can benefit by its apical collateral circulation and thus survive during the pulp necrosis process, which additionally explains why immature teeth with necrotic pulps can undergo completion of root development[59].SCAPs reside in the apical papilla of permanent immature teeth and appear to be the source of odontoblasts that are responsible for the formation of root dentin (Figure 3).Conservation of SCAPs when treating immature teeth may allow the continuous formation of the root to completion.
Overall, among adult tissues easily available through non-invasive dental procedures, SHEDs have a higher doubling time than DPSCs[39].However, PDLSCs showed a significantly higherin vitroosteogenic differentiation potential than both SHEDs and DPSCs (Figure 3), as evidenced by functional studies and gene expression indicating the complex influence of stem cell origin on their regenerative potential[60].
MODULATION OF DENTAL MSCS REGENERATIVE PROPERTIES IN HYPOXIC MICROENVIRONMENT
In the oral cavity, O2levels are shown to range from 0.7% and 3.8% in human periodontal pockets[61] and approximately 3% O2in the pulp tissue of rats[62]; therefore, given the therapeutic potential of dental MSCs, a number of studies have focused on examining their functions in such microenvironments.According to the published data, dental MSCs have been intensively investigated with regard to different O2levels, and detailed outcomes are shown in Table 1.
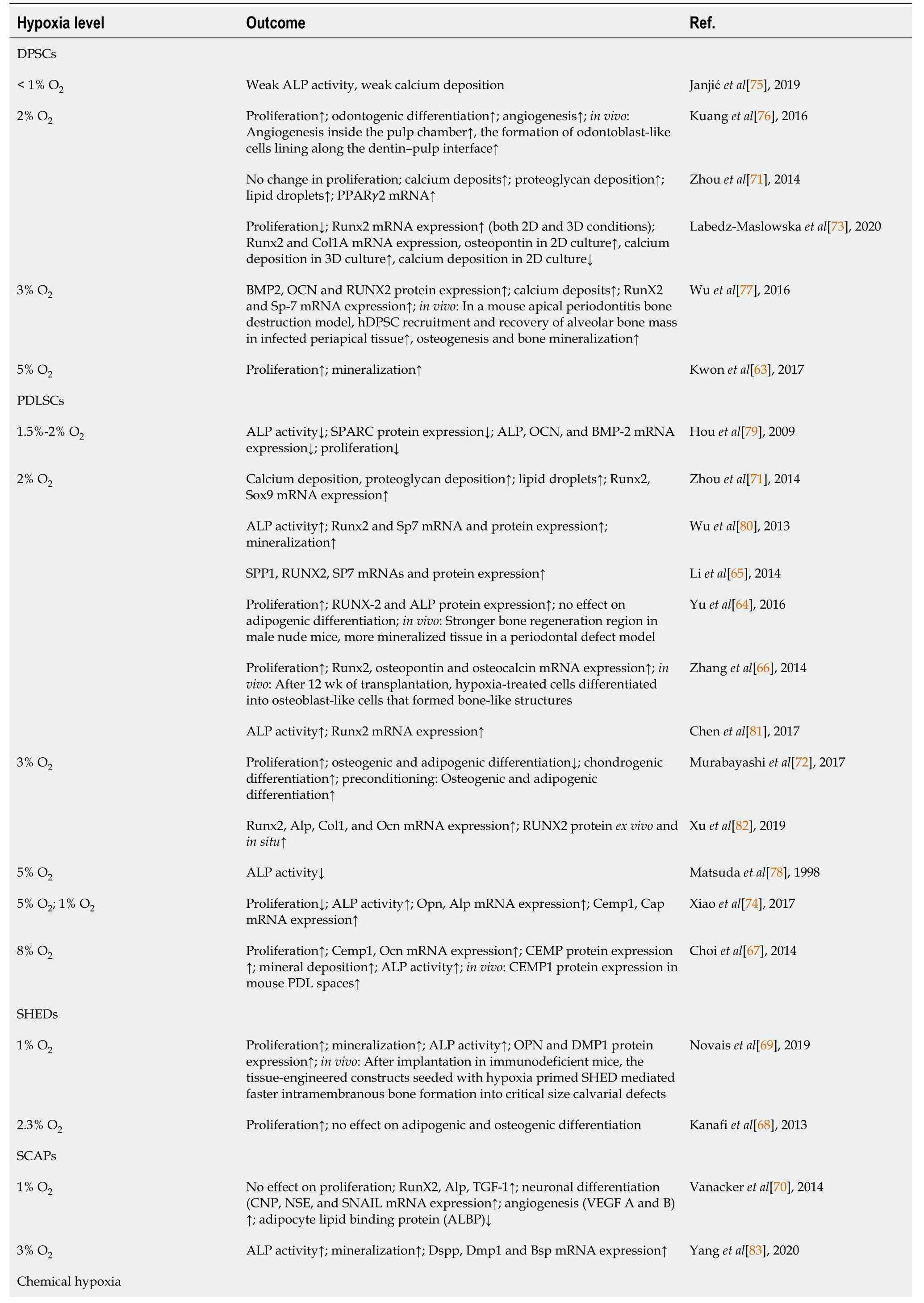
Table 1 Effects of different oxygen levels on regenerative potential of human dental mesenchymal stem cells
Although most studies showed that hypoxia stimulated proliferation of DPSCs[63], PDLSCs[64-67], SHEDs[68,69], and SCAPs[70], some reported it had no[71,72] or a negative effect[73,74].Also, results concerning the influence of hypoxia on differentiation capacity of MSCs derived from dental and dental supportive tissues are diverse.It was shown that under hypoxia, osteogenic differentiation of DPSCs was strongly suppressed compared to normoxia[75]; however, there are studies showing increased osteogenic[63,71], adipogenic and chondrogenic differentiation[71] at low O2levels.In order to mimic the native microenvironment of DPSCs, Labedz-Maslowskaet al[73] grew hydrogel-encapsulated cells in the presence of 2% O2.They showed upregulation of osteogenic differentiation in hypoxic conditions, but calcium deposition was, in the case of two-dimensional culture, more prominent under normoxia.Another study seeded DPSCs into nanofibrous spongy microspheres and showed that their priming at 2% O2prior to implantation significantly promoted the formation of odontoblast-like cells lining along the dentin-pulp interface of mice[76].On the other hand, Wuet al[77] showed that preconditioning of cells at 3% O2enhanced DPSC osteogenic differentiationin vitroand more importantly upregulated their recruitment in mouse apical periodontitis bone destruction model and enhanced osteogenesis and bone mineralization.
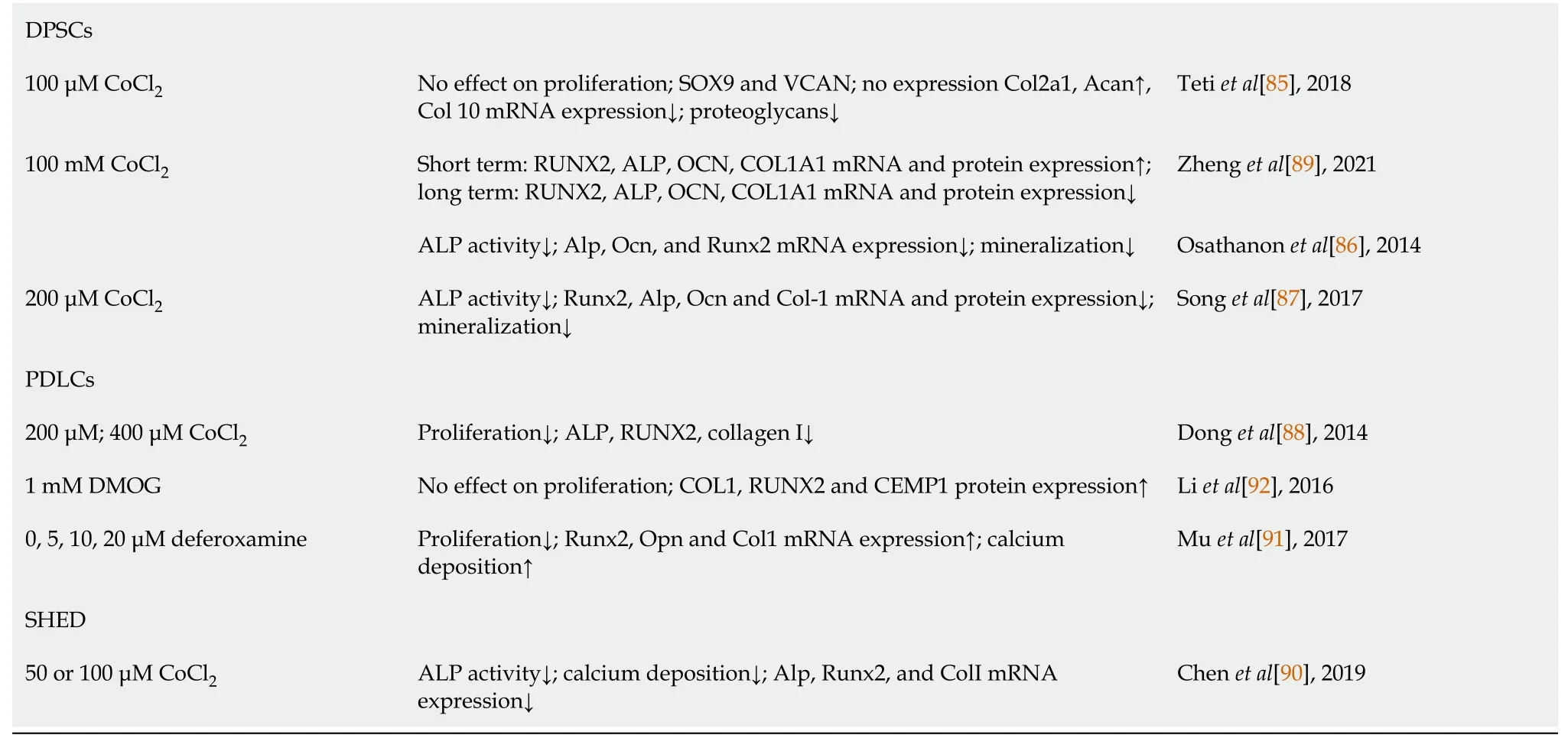
↑ and ↓ represent increasing or decreasing effect, respectively.ACAN: Aggrecan; ALBP: Adipocyte lipid binding protein; ALP: Alkaline phosphatase; BMP-2: Bone morphogenetic protein 2; BSP: Bone sialoprotein; CEMP 1: Cementum protein 1; COL-1: Collagen-1; DMOG: Dimethyloxalylglycine; DMP1: Dentin matrix protein 1; DPSCs: Dental pulp stem cells; DSPP: Dentin sialophosphoprotein; OCN: Osteocalcin; OPN: Osteopontin; PDLSCs: Periodontal ligament stem cells; PPARγ2: Peroxisome proliferator-activated receptor gamma; RunX2: Runt-related transcription factor 2; SCAPs: Stem cells from the dental apical papilla; SHEDs: Stem cells from human exfoliated deciduous teeth; Sox-9: SRY-box transcription factor 9; Sp-7: Osterix; SPARC: Secreted protein acidic and rich in cysteine; TGF- : Transforming growth factor-beta; VEGF: Vascular endothelial growth factor.β
While there is evidence that hypoxia decreased osteogenic differentiation of PDLSCs[65,78,79], it was demonstrated that it can also increase it[66,71,74,80,81] as well as adipogenic and chondrogenic differentiation[71].Interesting observations in some of these studies were that HIF1α promoted osteogenic differentiation of PDLSCs, while HIF1A antisense long noncoding RNA 2 had a negative effect on it[81] and that the stimulative effect of 2% O2on osteogenic differentiation of PDLSCs was mediated by extracellular signal-regulated kinase and even more rapidly and vigorously by p38 mitogen-activated protein kinase[80].The 24 h long pretreatment of PDLSCs under 2% O2increased osteogenesis, whereas cotreatment with tumor necrosis factor (TNF)-α and interleukin (IL)-β significantly reduced this effect, and no significant effects on adipogenic differentiation were observed[64].Importantly, the transplants containing hypoxic pretreated-PDLSCs led to significantly stronger bone regeneration when subcutaneously placed into the dorsal region of male nude mice as well as more mineralized tissue in a periodontal defect model[64].Similarly, PDLSCs grown at 2% O2differentiated into osteoblast-like cells that formed bone-like structures after transplantation into the backs of mice[66].Cultivation of these cells at 3% O2inhibited their differentiation capacity to osteogenic and adipogenic lineages, whereas it enhanced chondrogenic differentiation[72].However, the authors indicated that subsequent switch of 2 wk hypoxic preconditioned PDLSCs to normoxia allowed successful differentiation into osteogenic and adipogenic lineages.In contrast, Xuet al[82] found that 3% O2increased osteogenic markers expressionin vitroand augmented runt-related transcription factor (RUNX) 2 protein expressionex vivoandin situ viaHIF-1α-induced vascular endothelial growth factor, suggesting a positive role for HIF-1α in the early stage of osteogenesis of PDLSCs.Reduced O2tension besides osteogenic, increased cementogenic differentiation capability of PDLSCs[67,74], probablyviathe Wnt/b-catenin signaling pathway[74].It was found that HIF-1 activity is required to stimulate the differentiation responsein vitroand, more importantly, cementum protein 1 expression in mouse PDL spacesin vivo[67].
Although no difference in adipogenic and osteogenic differentiation potential of SHEDs was detected at 2.3% O2in comparison to normoxia[68], significantly higher osteogenesis was documented at 1% O2compared to control in SHEDs incorporated into plastically compressed collagen hydrogels[69].Moreover, after implantation in immunodeficient mice, these hypoxia-primed SHED constructs mediated faster intramembranous bone formation into critical size calvaria defects.Hypoxia significantly increased the osteogenic[70,83], neural, and angiogenic marker expression in SCAPs and suppressed their adipogenic differentiation[70].
When establishing hypoxic conditions in the laboratory, researchers sometimes encounter lots of technical difficulties (e.g., media changes), especially in long-term cultures, and therefore the use of chemical mimetic to induce hypoxic response has been an attractive alternative.Cobalt chloride (CoCl2) stabilizes HIF-1α and HIF-2α under normoxic conditions, and it is the most investigated hypoxia-mimetic agent[84].Supplementation of DPSCs with CoCl2had no effect on cell proliferation and reduced their chondrogenic[85] and osteogenic differentiation[86-88].Interestingly, it was observed that enamel matrix proteins[87] or apigenin, an HIF-1a inhibitor[86], could reverse the effect of CoCl2on osteogenic differentiation.Zhenget al[89] demonstrated that osteogenic differentiation of PDLSCs was activated by short-term exposure to CoCl2but was inhibited following prolonged exposure, which might be mediated by circular RNA circCDK8.CoCl2had the same osteo-reducing effect on SHEDs given the significantly decreased ALP activity, calcium deposition, and osteogenic marker messenger RNA expression[90].It was confirmed that deferoxamine[91] and dimethyloxalylglycine[92] promoted HIF1α expression in PDLSCs, and it was demonstrated that while proliferation was inhibited by deferoxamine, osteogenic differentiation was significantly promoted by both agents.The Wnt signaling pathways might be involved in dimethyloxalylglycine-induced differentiation of cells[92].
These findings provide important insights into capacity of dental MSCs to adapt to physiological conditions of low oxygenationin vitroby changing their regenerative properties.
MODULATION OF MSC REGENERATIVE PROPERTIES IN THE INFLAMMATORY MICROENVIRONMENT
In the human population, dental chronic inflammatory diseases are very common.For example, caries that cause progressive destruction of dental hard tissue[93] are one of the most frequent conditions in the oral cavity[94], particularly in childhood[95], while periodontal diseases—oral infections of tooth supportive tissue (gingivitis and periodontitis)—affect 20%-50% of the world population[96].If left untreated, these conditions can cause significant damage to the oral cavity and consequently cause major problems in the processes of chewing, swallowing, digestion, and speech and create aesthetic problems[93].Therefore, to consider the possibilities for regeneration and recovery of damaged oral tissue, it is necessary to perceive the regenerative potential of dental MSCs in the context of the inflammatory microenvironment.
Viewed from the perspective of physiological or pathological conditions, endogenous, resident MSCs respond to factors present in the immediate vicinity[57].Thus, inflammation caused by caries or periodontal disease may significantly affect regenerative capacity of dental MSCs, including their proliferation, migration, colony forming capacity, and differentiation.However, data related to the properties of MSCs isolated form inflamed dental tissues are not consistent (Table 2).Namely, recent results of Inostrozaet al[97] showed no significant differences between immunophenotype, trilineage differentiation, colony-formation, and proliferation of the DPSCs derived from healthy and inflamed pulp, although immunomodulatory functions of DPSCs from inflamed pulp were altered—showing decreased capacity to suppress CD3 T cell proliferation.Absence of CD34 and CD45 markers, along with high expression of MSC-associated markers between DPSCs extracted from normal and diseased pulp, was also observed in Parket al[98].Besides, in comparison to control cells, DPSCs from inflamed tissue manifested higher osteogenesis (stronger mineralization and expression of osteogenic markersOCNandRUNX2) but lower neurogenesis (decreased expression of neurogenic markers microtubule-associated protein 2, neuronal nuclear protein, and glutamate decarboxylase 6), along with higher level of IL-6 expression.This study also shows the significance of IL-6, as a strong inflammatory factor, to modulate DPSCs function.Namely, the IL-6 treatment of DPSCs derived from healthy tissue stimulated their osteogenic differentiation and reduced neurogenic differentiation, while IL-6 blocking in DPSCs of inflamed tissue annulled their osteogenic/neurogenic capacity[98].
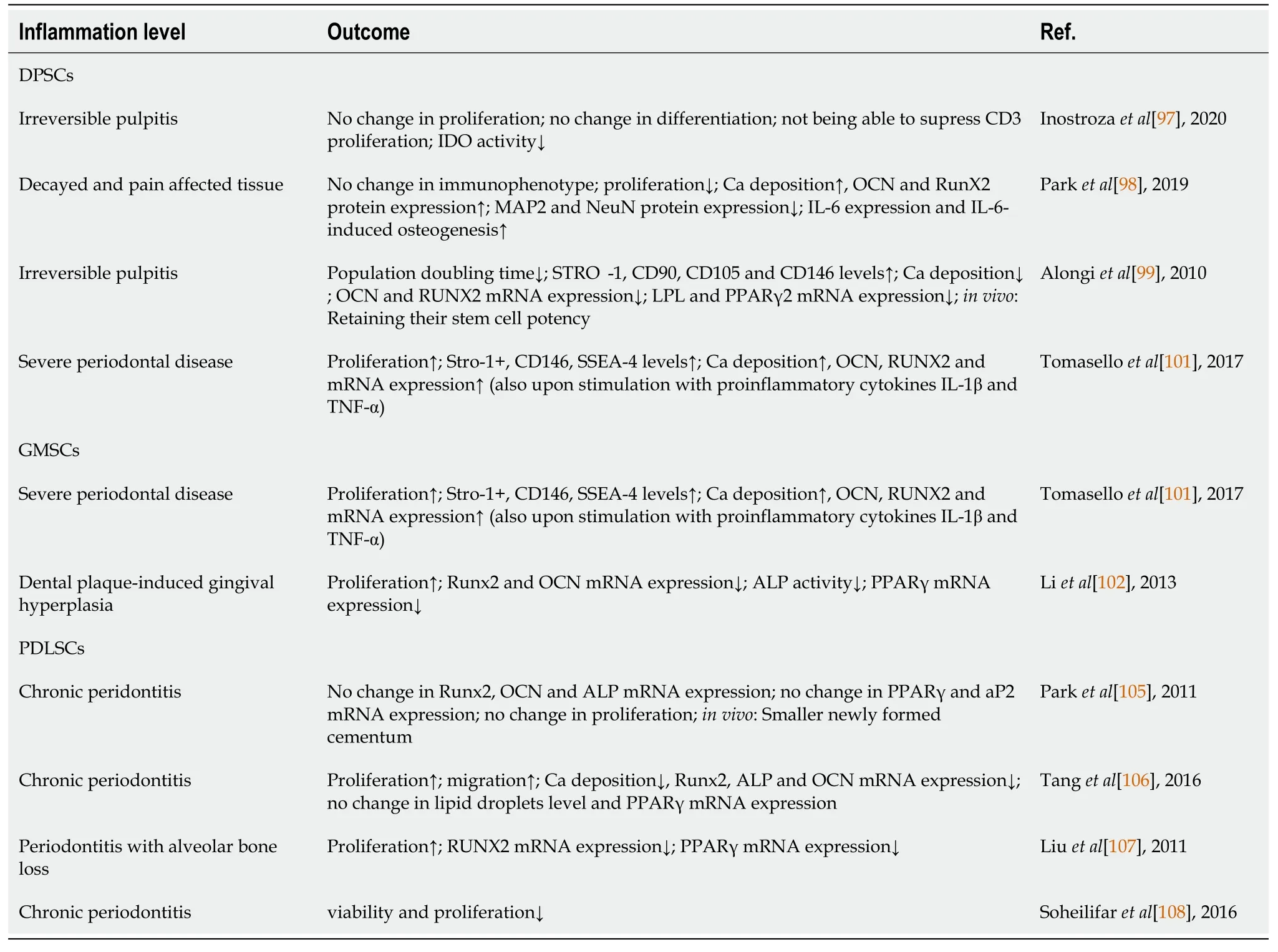
Table 2 Effects of inflammatory microenvironment on regenerative potential of human dental mesenchymal stem cells
Contrary to these studies, compared to the control cells, DPSCs isolated from inflamed pulp expressed higher levels of MSC markers, while their capacity to proliferate was increased with reduced osteo/dentinogenic differentiation potentialin vitro.Still, as well as DPSCs from healthy pulp, DPSCs of inflamed tissue retained their capacity to form pulp/dentin complexes after transplantation into immunocompromised mice,i.e.their regenerative capacity was preserved[99].In the context of optimal dental MSC isolation, Tsaiet al[100] demonstrated that dental diseases represent significant factors that affect MSC isolation and quality, given that successful MSCs yield was less pronounced from carious deciduous tooth or tooth with pulpitis.As for dental MSCs isolated from inflamed tooth supportive tissue, Tomaselloet al[101] showed that DPSCs and GMSCs derived from the tissue affected by periodontitis proliferate faster and possess more pronounced mineralization.Also, no changes in negative MSC marker expression or in high expression of a positive MSC marker (CD29) were detected, while expression of other positive MSCs markers, such as Stro-1, CD146, and stage-specific embryonic antigen-4, was higher in DPSCs and GMSCs of inflamed tissues.In another study, increased proliferation, but with reduced osteogenic and adipogenic differentiation, of GMSCs under inflammatory conditions was observed[102].Also, higher levels of matrix metalloproteinases (MMP)-1, MMP-2, IL-1, IL-6, TNF-α and type COL1A1 were detected in GMSCs collected from inflamed gingival tissues, indicating the potential of inflammatory environment to shift differentiation capacity toward pro-fibrotic phenotype, thus representing possible mechanism of gingival hyperplasia development during inflammation[102].
A recently published article provided a comprehensive review of papers related to the characteristics of GMSCs from healthy and inflamed tissue, altogether suggesting that GMSCs of inflamed tissues could be a reliable source of MSCs when compared to the healthy gingiva[103].Inflammatory environment can also alter properties of PDLSCs[104], however findings are not clear since other publications suggest that there are no significant differences between PDLSCs of healthy and diseased periodontal tissue[105].Enhanced proliferation but reduced differentiation of dental MSCs derived from inflamed tissue has been detected for PDLSCs isolated from diseased tooth supportive tissue[106,107], while the study of Tanget al[106] also demonstrated increased migration of PDLSCs originating from inflamed periodontal tissue.Higher migratory potential with preserved osteogenic/cementogenic and adipogenic differentiation was reported in Parket al[105], and in anin vivotransplantation model, they showed that PDLSCs from inflamed periodontal tissue possess a preserved ability to form new cementum-like tissue and related periodontal fibers.However, similar to the findings of Tsaiet al[100], related to the yield of MSCs derived from diseased tooth, Soheilifaret al[108] reported that viability and proliferation rate of PDLSCs isolated from the periodontitis-affected teeth were significantly lower in comparison to the control PDLSCs.
Having in mind that the regenerative ability of transplanted dental MSCs strongly depend on the donor/recipient microenvironment niche, gaining successful therapeutic effect in diseased microenvironment is the biggest challenge[56].Further understanding the influence of the diseased tissue microenvironment on MSC regenerative potential would help the establishment of healing procedures.
CLINICAL RELEVANCE OF DENTAL MSCS
Numerousin vivostudies on animals and human clinical trials with various types of dental stem cells show a way to encourage novel tissue engineering strategies for therapies of dental diseases[109].However, a long road is still ahead, as clinical trials are in their early phases.Despite abundance of preclinical studies, only a few clinical trials have been completed and published.One of the main reasons that stalls successful clinical application of dental stem cells resides in the fact that the exact mechanism of their therapeutic properties is not yet clear.The other challenges for clinical use of dental stem cells are strict regulations, high costs of cell processing, and lack of uniformity in approaches for isolation, expansion, and application of these cells.The therapeutic efficacy of transplanted dental MSCs is also compromised by the diseased microenvironment of the recipients[56].
DPSCs, as the first discovered dental tissue-derived stem cells, are also the most studied stem cells for dental tissue reparation[110].Even though there are many studies in large animal models showing promising results in dental tissue regeneration, especially in dentin and dental pulp regeneration[110], results of clinical studies are less conclusive.The first study to achieve successful reparation of alveolar bone defect in humans was done by d’Aquinoet al[111].They used autologous DPSCs from third maxillar molars seeded onto a collagen sponge scaffold to fill the space left after the extraction of an impacted mandibular molar from the same patient (7 patients in total).A contralateral extraction site filled with sponge without cells served as a control (a split-mouth study design).Clinical and radiographic assessment after 3 mo and 1 year revealed optimal vertical repair and complete restoration of periodontal tissue[111].In a pilot clinical study, Nakashimaet al[112] demonstrated a safe and efficacious method for complete pulp regeneration in 5 patients with irreversible pulpitis using autologous DPSCs transplanted with granulocyte colony-stimulating factor in atelocollagen into pulpectomized teeth.However, a split-mouth randomized clinical trial on 32 patients, aiming to assess the efficacy of autologous DPSCs delivered in a collagen matrix for post-extraction socket healing, failed to show significant reduction in the socket bone resorption in the treated group compared to control[113].It is noteworthy that, unlike in the other cited studies, in this trial a proprietary medical device and protocol (Rigenera®) for direct isolation of DPSCs from dental pulp was used, without prior expansion in culture.
DPSCs from deciduous teeth are also frequently used in dental tissue regeneration studies.In a randomized control clinical trial, Xuanet al[114] isolated autologous SHEDs from deciduous canine tooth pulp and implanted them in the form of aggregates, into an injured incisor of the patient with pulp necrosis secondary to trauma.Control patients were treated with standard apexification (a procedure that induces tooth root development and closure of the root apex through hard tissue deposition).After 12 mo follow-up, SHED implantation treatment led to regeneration of functional dental pulp with blood vessels and sensory nerves.In another study, Tanikawaet al[115] used SHEDs associated with HA-collagen sponge for closing alveolar defects in patients with unilateral alveolar cleft defects and demonstrated that this therapy leads to bone regeneration with dental eruption and reduced morbidity compared to traditional iliac crest bone grafting and rhBMP-2.
Among other dental stem cells, alveolar bone derived MSCs also represent great promise in regenerative therapy.A pilot clinical trial evaluated treatment of maxillary radicular cysts in 9 patients using autologous alveolar bone-derived MSCs seeded onto a glutaraldehyde-cross-linked autologous serum scaffold and subjected to osteogenic differentiation[116].It demonstrated a significant promotion of bone growth in all MSC-treated cysts.
In addition to osteal defects and pulp necrosis, periodontal diseases make up a large proportion of dental ailments targeted for regenerative therapy.A retrospective pilot study examined feasibility and safety of reconstructing the periodontal intrabony defects in 16 teeth of 3 patients with implantation of autologous PDLSCs mixed with a HA-based bone-grafting material[117].After 32-72 mo follow-up period, clinical examination indicated improvement of probing depth, clinical attachment level, and gingival recession.In a randomized controlled study, Ferrarottiet al[118] used a biocomplex of autologous dental pulp micrografts (Rigenera®) with collagen sponge to fill intrabony defects of 29 chronic periodontal patients randomly allocated to test (n= 15) and control (n= 14) groups[118].This treatment significantly improved clinical parameters of periodontal regeneration 1 year after the procedure.A novel approach using cell sheets of cultured autologous PDLSCs to treat periodontitis was assessed in a case series study involving 10 patients with chronic periodontitis[119].Triple layered PDL-derived cell sheets with PGA mesh were transplanted on the root surface, and βtricalcium phosphate (β-TCP) granules were used to fill in bony defects.In all 10 cases, clinical as well as radiographic endpoint parameters improved 6 mo after the treatment.On the other hand, a randomized clinical trial on 30 patients, with 41 teeth in total, using autologous PDLSCs in combination with grafting materials to treat periodontal intraosseus defects, revealed radiologically and clinically greater, but not statistically significant, regeneration of alveolar bone in cell-treated group compared to control group[120].
A recent pilot trial evaluated the safety and efficacy of autologous PDLSC transplanted with a commercial xenogeneic (porcine) bone substitute as a matrix for the regeneration of intrabony defects of 19 patients with chronic periodontitis[121].The study confirmed the safety of the treatment, but the results have not demonstrated a significant additional clinical benefit compared to control, after 12 mo follow-up.In a randomized clinical trial designed to investigate the use of gingival fibroblasts and GMSCs in the treatment of intrabony periodontal defects, a total of 20 patients with periodontitis were evenly assigned into two groups[122].Experimental group received cultured autologous gingival fibroblasts/GMSCs on β-TCP scaffold, covered by a collagen membrane, and the control group received β-TCP without the cells.After 6 mo, the study showed significant improvement of clinical and radiological parameters in comparison to the control group.
CONCLUSION
Dental tissues represent valuable sources of MSCs for possible use in regenerative therapy, especially of diseases associated with bone defects and dental loss.Given the different structures and compositions of the tissues they reside in, various dental MSCs exhibit diverse biological and functional features.Therefore, in this review, we have summarized the available research evidence concerning the effects of hypoxic and inflammatory microenvironmental factors on dental MSCs differentiation capacity.We can conclude that the existing investigations indicate very important aspects of the recipient microenvironment niche in terms of therapeutic efficacy of transplanted dental MSCs.Moreover, the therapeutic potential of dental MSCs inin vitroconditions mimicking native hypoxic and inflammatory microenvironment can lead to significant development of cell-based therapies.
However, some of the data for the same cell type (especially in hypoxicin vitroconditions) are conflicting, which is a trend noticed for other MSCs as well[20].Therefore, it is important to point out that the biology of MSCs is not yet fully known.As MSC populations exhibit functional heterogeneity and a hierarchy in the terms of proliferative and differentiation potential and metabolic properties of the cells composing the tissues[123], they can behave differently even within the same tissue of healthy individuals.Moreover, the cultivation conditions affect their characteristics, and not all studies covered by this review used the same cell isolation methods and/or the same cell passages.It should be also taken into account that inflammation doesn’t solely contribute to these contradictory findings, given the lack of data on specificity of the inflamed tissues in the terms of proinflammatory factors involved.In addition, the reason for inconsistencies in results related to the same O2levels can be found in different experimental settings such as the duration of the hypoxic treatment.Taken together, we suggest further research in this area, but with synchronized cell isolation methods, cultivation conditions, and experimental designs among research groups.
杂志排行
World Journal of Stem Cells的其它文章
- Stem cell-derived biofactors fight against coronavirus infection
- Application of mesenchymal stem cells derived from human pluripotent stem cells in regenerative medicine
- Strategies to improve regenerative potential of mesenchymal stem cells
- Regulating the fate of stem cells for regenerating the intervertebral disc degeneration
- Bone marrow mesenchymal stem cell therapy regulates gut microbiota to improve post-stroke neurological function recovery in rats
- SmartFlareTM is a reliable method for assessing mRNA expression in single neural stem cells
