Successful treatment of complete traumatic transection of the suprahepatic inferior vena cava with veno-venous and cardiopulmonary bypass with hypothermic circulatory arrest ✩
2022-01-07PuloMrtinsJulinnBuhwldBkMovhediUlisesTorresTimothyEmhoffJenniferWlkerMihelDeBuskAdelBozorgzdeh
Pulo N. Mrtins ,# , Julinn E. Buhwld ,# , Bk Movhedi , Ulises Torres ,Timothy Emhoff , Jennifer Wlker , Mihel G. DeBusk , Adel Bozorgzdeh ,
a Department of Surgery, Division of Transplantation, University of Massachusetts, Worcester, MA 01655, USA
b Department of Surgery, Division of Trauma, University of Massachusetts, Worcester, MA 01655, USA
c Department of Surgery, Division of Cardiac Surgery, University of Massachusetts, Worcester, MA 01655, USA
TotheEditor:
Complete traumatic transection of the suprahepatic inferior vena cava (IVC) has almost invariably a fatal outcome. There are very few cases in the literature of patients that survived this type of injury. Here we presented a case that was approached multidisciplinary (trauma surgeon, liver transplant surgeon, perfusionist,anesthesiologist, and cardiac surgeon) with a successful outcome including early recovery of all body functions and quality of life.We also reviewed the literature of cases of survival following blunt incomplete and complete IVC transection including those treated with cardiopulmonary bypass.
A 57-year-old female presented to the emergency room (ER)of our hospital (Level 1 trauma center) 1 h following an unrestrained motor vehicle accident involving collision with a pole and no airbag deployment. The patient presented oriented to self, time,and place but was hemodynamically unstable with a systolic blood pressure of less than 80 mmHg. Additionally, the patient had a positive focused assessment with sonography for trauma (FAST)exam, Glasgow score of 15, and no neurological deficit. The injury severity score (ISS) was 54 (out of 75) on the ISS scale [1] . Her initial blood pressure was 64/52 mmHg with abnormal lab values of Na+149 mmol/L, hematocrit 36%, lactate 4.3 mmol/L, pH 7.33, PO2195 mmHg, and HCO3-19.3 mmol/L.
After our initial attempt to optimize her in the ER being unsuccessful, the patient was sent to the operating room (OR) (time from arrival at ER to arrival at OR was about 30 min). The decision was made to operate given that the patient presented as hemodynamically unstable with severe hypotension and a positive FAST exam in the setting of an unrestrained motor vehicle accident without air bag deployment. At arrival in the OR, the patient arrested and underwent cardiopulmonary resuscitation with chest compressions and manual bag ventilation for 10 min. In addition, the patient received a bolus of adrenaline. Upon laparotomy, the trauma surgeon noted a type V liver injury as per organ injury scale [2] and a complete transection of the suprahepatic IVC. Lacerations of the liver capsule, diaphragm, and spleen capsule were also identified. The abdomen was packed and a Pringle maneuver was performed to prevent bleeding during the veno-venous bypass (inferior mesenteric vein/portal vein and femoral vein/IVC to the internal jugular vein) ( Fig. 1 , Video S1) while allowing for increased blood return to the heart with liver perfusion and bowel decompression. A clamp was placed at the suprahepatic IVC stump and the liver transplant team and a cardiac surgeon performed a sternotomy (extending the initial xyphopubic incision). The IVC was then clamped just below the right atrium to control bleeding and prevent air embolism. We combined the use of a Finochietto sternal retractor(Millennium Surgical, Bala Cynwyd, PA, USA), an Iron Intern retractor (Automated Medical Products, Edison, NJ, USA), and a Bookwalter retractor (Symmetry Surgical, Antioch, TN, USA) ( Fig. 1 , Video S1) to allow for maximal exposure. The cannulas were placed in the aorta, right atrium, inferior mesenteric vein/portal vein, and left femoral vein (through a cut-down). The inferior mesenteric vein/portal vein and left femoral vein were cannulated with fenestrated cannulas and connected by a Y-connector to the outflow line. The left internal jugular vein was cannulated as inflow to the heart.
The liver was mobilized and vasculature isolated, a radial opening of the diaphragm was created, a pericardiotomy was performed, and a vascular clamp on the intrapericardial IVC was placed. The inferior mesenteric vein was then cannulated and the liver bypass circulation was started. The aorta was briefly clamped until the blood pressure improved and the cardiopulmonary bypass circulation was started, followed by hypothermia and cardiac arrest due to the injury extending to the right atrium.
To repair this injury, we used a 4-cm long and 2.5-cm diameter Dacron graft that was initially sutured to the liver side of the IVC. The hepatic veins were not injured. The graft was then anastomosed to the atrium. The abdomen and chest were left open with placement of ABThera VAC dressing.

Fig. 1. Schematic (created with BioRender.com) ( A ) and photograph of the operative field ( B ) showing the suprahepatic inferior vena cava (IVC) repaired with Dacron prosthesis and the cardiopulmonary and the liver veno-venous (inferior mesenteric vein/portal vein and femoral vein/IVC to the jugular vein) bypasses. Aorta cannula (a),right atrium cannula (b), inferior mesenteric vein/portal vein cannula (c), Dacron graft prosthesis (d), left femoral vein/IVC cannula to jugular vein (e).
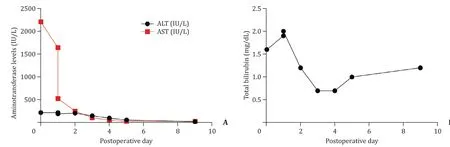
Fig. 2. Liver function tests indicating aminotransferase ( A ) and total bilirubin ( B ) levels following repair of the traumatic inferior vena cava transection.
The total duration of the operation was 310 minutes. The patient was fully heparinized during the operation because of the extracorporeal circuit. The cardiopulmonary bypass time was 45 minutes of hypothermia (24 °C) with 13 minutes of cardiac circulatory arrest. The time on liver veno-venous bypass was 90 minutes. The estimated blood loss was 12 L, and we used 20 U of packed red blood cells, 24 U of fresh frozen plasma, 3 U of cryoprecipitate,4 U of platelets, 1 L of albumin, and 4.1 L of cell saver blood. The urine output during the entire case was 1450 mL.
The patient had a relatively uncomplicated postoperative course with no deterioration of liver, kidney, and lung function and no associated neurological deficit. The postoperative anticoagulation consisted of standard subcutaneous heparin for deep vein thrombosis prophylaxis. On postoperative day 1 (POD 1), the patient returned to the OR for a second look, washout, cholecystectomy, sternotomy closure, diaphragm reconstruction, and liver biopsy. We performed a cholecystectomy because of concerns of possible ischemic cholecystitis caused by shock in the setting of liver vascular isolation. The liver biopsy on POD 1 was normal, with liver function also returning to normal several days after the surgery( Fig. 2 ). The diaphragm defect was repaired with Permacol ( Fig. 3 ).Her echocardiogram was normal on POD 5 (ejection fraction 70%).Abdominal CT scan with intravenous contrast on POD 7 confirmed successful IVC reconstruction with well-perfused liver parenchyma( Fig. 4 , Videos S2-S4).
The patient’s length of stay in the ICU was 6 days and in the hospital 18 days. The patient is now nearly 4 years after the accident and is back to baseline with no neurological or physical deficit.
Blunt suprahepatic IVC transection is very rare and frequently fatal. It is usually associated with major injuries to the brain,heart, liver, spleen and chest and is also associated with exsanguination, cardiac tamponade, and air embolism leading to cardiopulmonary collapse and death at the scene. Initial survivors often die later due to multiorgan failure and sepsis. There are several approaches to suprahepatic IVC injury depending on the degree of injury including primary repair, vascular reconstruction with prosthesis (Dacron graft/pericardial patch), liver resection,ex vivobench repair and re-implantation of the liver, and conservative/endovascular approaches (in very selective cases) [ 3 -9 ]. Fast and efficient reestablishment of the circulation is of paramount importance and may include an atriocaval shunt, vascular isolation of the liver, liver veno-venous bypass, and cardiopulmonary bypass.

Fig. 3. Diaphragm reconstruction with decellularized skin (Permacol) on postoperative day 1.

Fig. 4. Abdominal CT scan with intravenous contrast on postoperative day 7 ( A ) demonstrating suprahepatic inferior vena cava reconstruction without any stricture ( A and C ). The liver parenchyma was well-perfused throughout ( B ) without any associated infarcted areas.
A review of the literature on cases of reported survival following blunt suprahepatic/juxtahepatic/hepatic incomplete IVC transection revealed 31 cases, with 22 below the age of 30 ( Table 1 ) [ 5 , 7 , 8 , 10 -23 ]. In addition, 8 of these cases required associated hepatectomy, while none required cardiopulmonary resuscitation. Furthermore, 1 out of the 8 cases used an atriocaval shunt which was eventually abandoned due to severe bleeding. Of the 31 cases involving incomplete IVC transection, only 5 used cardiopulmonary bypass which resulted in patient survival( Table 2 ) [ 24 -28 ].
When there is major laceration of the IVC and/or hepatic veins or complete transection of the IVC, complex vascular reconstructions are necessary. It is very challenging to control an IVC injury and repair it when there is massive bleeding and lack of an IVC cuff on the liver and heart. In those cases, the best approach may require cardiopulmonary bypass and liver bypass, partial hepatectomy, or evenexvivobench repair and reimplantation of the liver(auto-transplantation) [27] .
A review of the literature on cases reported following complete blunt IVC transection revealed only 3 survivors, with 1 using cardiopulmonary bypass via the right femoral vein and artery with placement of a venous cannula in the superior vena cava ( Table 3 ) [ 22 , 29 , 30 ].
Cardiopulmonary bypass and liver bypass require full heparinization, and take time to be set up. These procedures allow ideal technical conditions for reconstruction in an almost bloodless field with a still heart for clamping of the atria. Liver vascular isolation and veno-venous bypass also allow for better visualization of the injury and prevention of bleeding. The liver veno-venous bypass allows shunting of the inferior mesenteric vein/portal vein and femoral vein/IVC to the internal jugular vein to increase blood return to the heart and allows perfusion of the liver (avoiding prolonged Pringle maneuver and liver ischemia). In addition, veno-venous bypass allows bowel decompression caused by the portal vein cross-clamping (Pringle), preventing abrupt release of accumulated ischemic gut metabolites (lactic acid and cytokines) that lead to hemodynamic instability (reperfusion syndrome/declamping shock), while also preventing bowel edema [ 31 -33 ]. Veno-venous bypass has been very effective to obviate these hemodynamic and physiologic complications during the anhepatic phase of liver transplantation [33] .
The time to establish veno-venous bypass is short and the risk of complications is low in the hands of surgeons familiar with it. Some of the claimed disadvantages of using veno-venous bypass is that it leads to longer operative time and may cause postoperative thromboembolism secondary to vascular injury and stricture [ 34 -36 ]. In our case, the veno-venous bypass was established only after the massive bleeding was controlled with packing and vascular clamps and crucial time was then spent fixing the presenting injury.
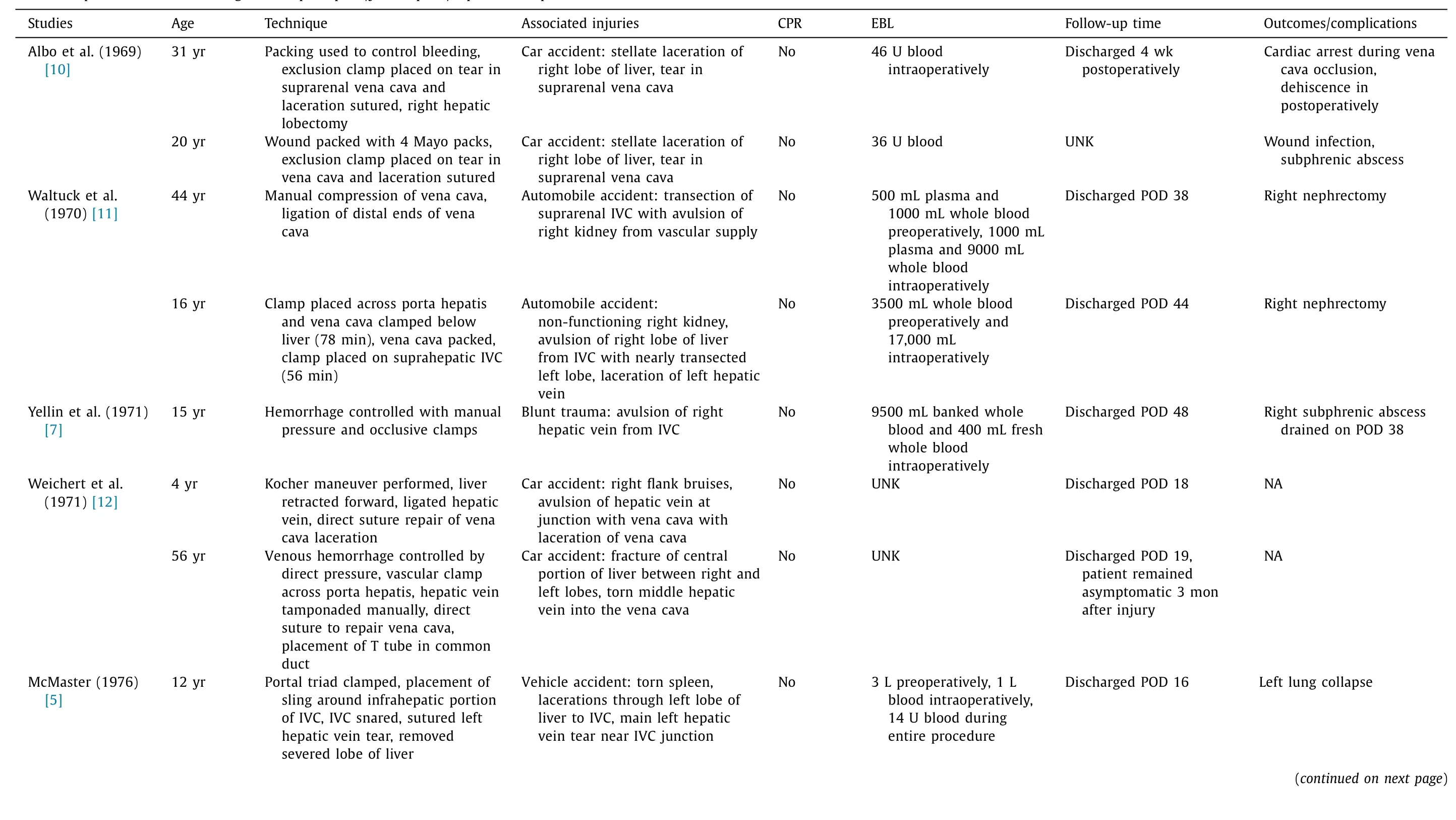
Table 1 Cases of reported survival following blunt suprahepatic/juxtahepatic/hepatic incomplete IVC transection.

Table 1 (continued)

Table 1 (continued)
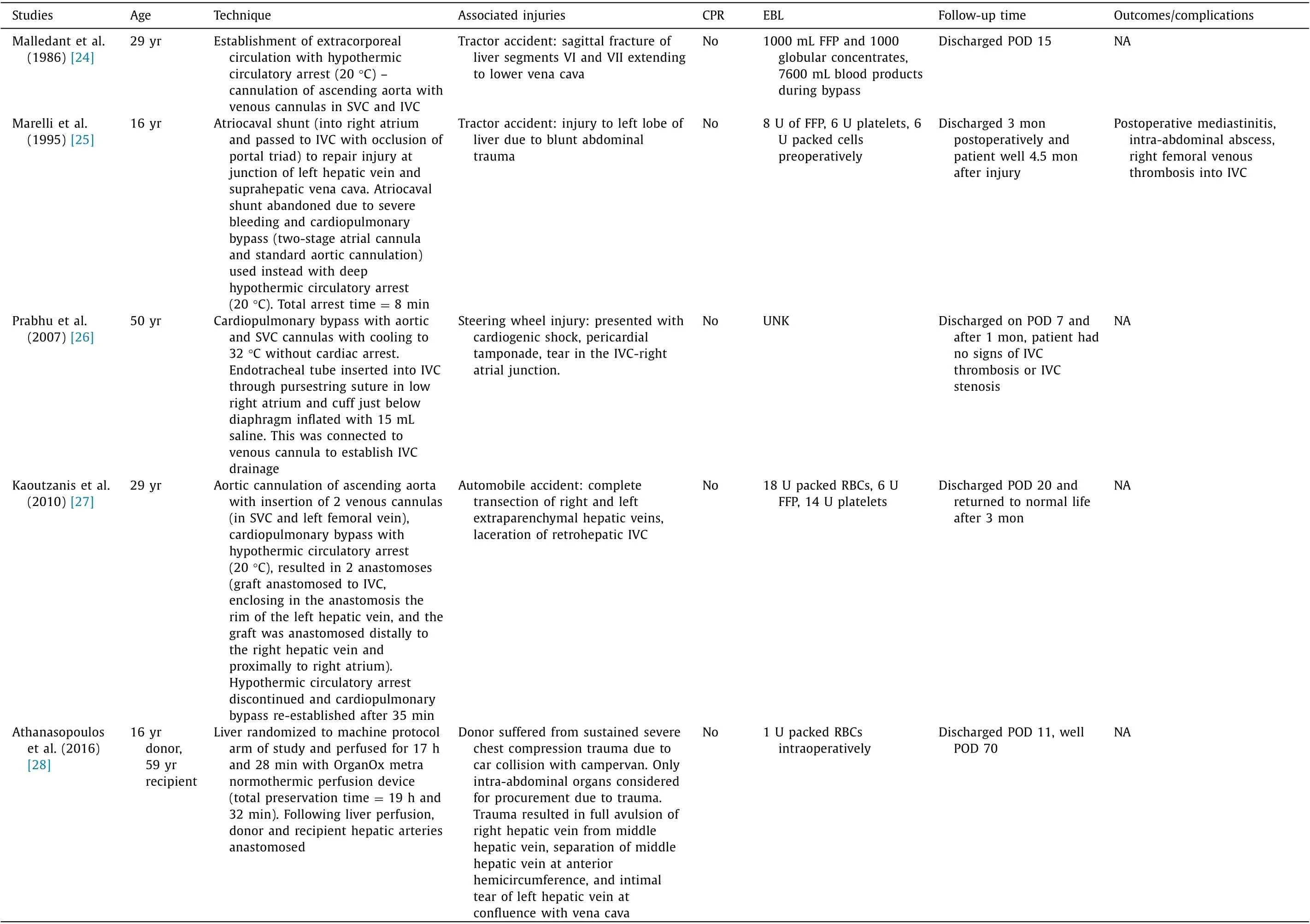
Table 2 Cases of survival of suprahepatic/juxtahepatic/hepatic inferior vena cava blunt trauma using cardiopulmonary bypass.
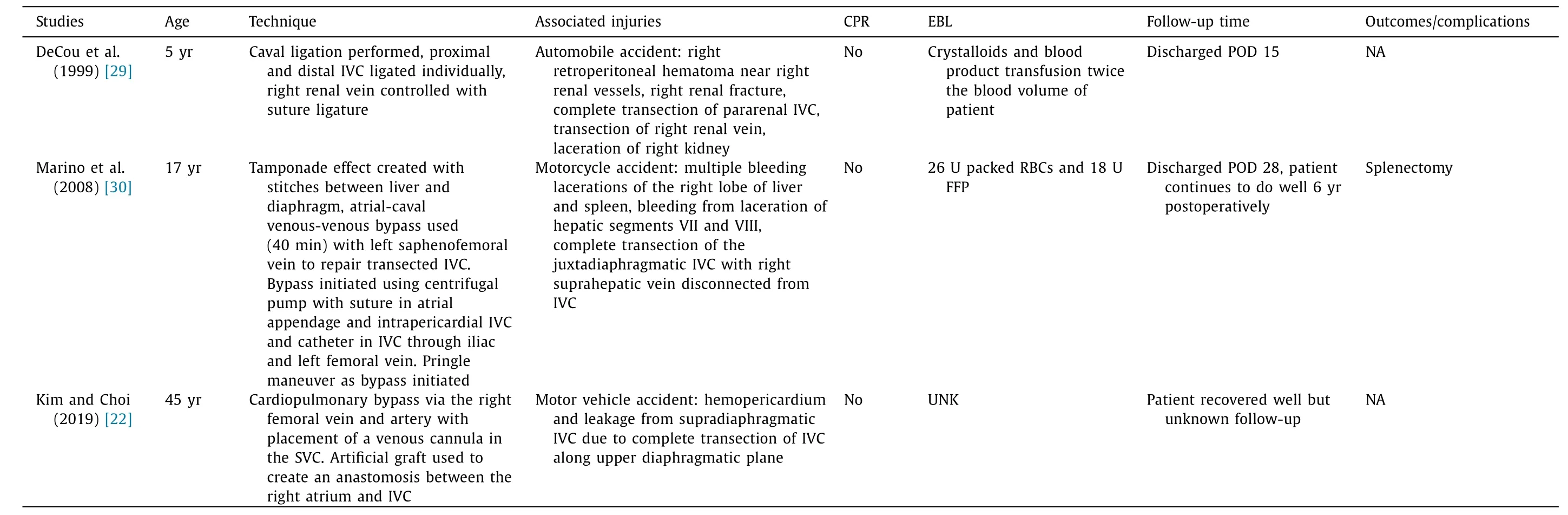
Table 3Cases of reported survival following blunt suprahepatic/juxtahepatic/hepatic IVC transection.
A review of the literature reveals only a handful of cases where IVC injuries were corrected with liver veno-venous bypass alone.Baumgartner et al. [15] reported 5 cases where veno-venous bypass (left common femoral venous shunt with outflow to left axillary vein) was performed following blunt trauma resulting in 4 cases of survival. None of the 5 patients underwent systemic heparinization, but heparin bonded tubing was implemented. Rogers et al. [17] performed total vascular isolation of the liver while using veno-venous bypass (saphenofemoral with return to axillary vein) to maintain the preload to the heart for repair of IVC injury.Marino et al. [30] reported use of atrial-caval veno-venous bypass between left saphenofemoral vein to repair the transected IVC. The bypass was initiated by using a centrifugal pump with a suture placed in the atrial appendage and intrapericardial IVC with placement of a catheter in the IVC through the iliac and left femoral vein. Lastly, Madigan et al. [21] reported use of veno-venous bypass in the right jugular and common femoral veins following an automobile accident resulting in suprahepatic IVC injury without the use of circulatory arrest.
In our case, we decided to use a veno-venous bypass and cardiopulmonary bypass because of a complete IVC transection. In these circumstances, placement of an atriocaval shunt is not appropriate given its challenging placement and risk of leakage around the shunt. An atriocaval shunt is usually quicker to establish in partial small lacerations but not in the case of complete transections.This is because the retrohepatic IVC would likely not be aligned with the suprahepatic IVC as a result of liver displacement due to hematoma formation, which could cause liver parenchymal injury when advancing the cannula caudally. Additionally, the removal of the liver and its re-implantation (auto-transplantation) was not considered in our case because control of the bleeding and establishment of the veno-venous bypass and cardiopulmonary circulation were performed quickly. Auto-transplantation may be an option in such cases where further IVC ease of access and rapid blood control is required and not controlled otherwise.
The main advantage of portal vein bypass is to avoid complete ischemia of the liver in complex and lengthy repairs, though there are survival cases that did not employ this approach. By using the veno-venous portal bypass, prolonged clamping of the liver hilum was avoided, allowing liver perfusion through the hepatic artery and likely some flow through the portal vein. Veno-venous bypass also prevented bowel congestion and partial ischemia/acidosis and reperfusion syndrome after release of prolonged portal vein clamping.
It is important to note that most liver transplant centers have abandoned the use of veno-venous bypass or have reserved this technique for very selective cases because it requires additional time and costs. Regardless of the necessity of its use, veno-venous bypass is associated with better hemodynamics during the anhepatic phase, as aforementioned. In our trauma case, we describe a different situation in which the patient already came into the operating room with severe hypotension and under cardiopulmonary resuscitation. Given these circumstances, the extension of the lesion could not be quickly repaired without the use of veno-venous bypass. The patient would have experienced prolonged low blood return to the heart, decreased cardiac output and organ damage(especially brain function), and total and prolonged liver ischemia.In similar cases where there is limited or no availability of liver transplant surgeons, it is difficult to suggest alternative options for trauma surgeons. Complete IVC transections are almost invariably fatal, even when all infrastructure and specialists are readily available, with the literature revealing only 3 total cases of reported survival following complete IVC transection ( Table 3 ).
In conclusion, prompt treatment by a specialized multidisciplinary team is essential to optimize results after severe injury of the suprahepatic IVC. Ideal exposure and a bloodless field are critical to repair complex suprahepatic IVC injuries. A veno-venous bypass including cannulation of the portal vein to improve cardiac output, prevent liver congestion, and decompress the intestine, in addition to cardiopulmonary bypass with hypothermic circulatory arrest to improve oxygenation and facilitate complex repair, may improve outcomes following traumatic IVC transection.
Acknowledgments
None.
CRediT authorship contribution statement
Paulo N. Martins: Conceptualization, Data curation, Formal analysis, Writing - original draft, Writing - review & editing.Julianna E. Buchwald: Conceptualization, Data curation, Formal analysis, Funding acquisition, Writing - original draft, Writing - review & editing. Babak Movahedi: Conceptualization, Data curation,Formal analysis, Writing - review & editing. Ulises Torres: Conceptualization, Data curation, Formal analysis, Writing - review &editing. Timothy Emhoff: Conceptualization, Data curation, Formal analysis, Writing - review & editing. Jennifer Walker: Conceptualization, Data curation, Formal analysis, Writing - review & editing.Michael G. DeBusk: Conceptualization, Data curation, Formal analysis, Writing - review & editing. Adel Bozorgzadeh: Conceptualization, Data curation, Formal analysis, Writing - review & editing.
Funding
This study was supported by a grant from the National Institutes of Health (NIH) ( T32GM1070 0 0 ).
Ethical approval
Informed consent for publication was obtained from the patient.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Supplementary materials
Supplementary material associated with this article can be found, in the online version, at doi: 10.1016/j.hbpd.2020.12.017 .
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Hepatocellular-cholangiocarcinoma with sarcomatous change:Clinicopathological features and outcomes
- Successful withdrawal of antiviral treatment in two HBV-related liver transplant recipients after hepatitis B vaccination with long-term follow-up
- High perioperative lactate levels and decreased lactate clearance are associated with increased incidence of posthepatectomy liver failure
- An NSQIP survey of outcomes after resection of choledochal cysts in adults
- Glucagonoma syndrome with necrolytic migratory erythema as initial manifestation
- A rare type of choledochal cysts of Todani type IV-B with typical pancreaticobiliary maljunction